Mental and Behavioral Health Assessment Tools
75+ Rating Scales & Assessment Tools
The only behavioral health EMR improving compliance while reducing documentation time.
With the ICANotes Behavioral Health EHR, clinicians have access to more than 75 different electronic rating scales and assessment tools for adults and children. These rating scales and behavioral health assessments are integrated with the patient's mental health chart and treatment plans to ensure all patient records are easily accessible and secure. Built-in electronic assessments are available for depression, anxiety, PTSD, mood disorders, substance abuse and so much more, allowing clinicians to spend less time on paperwork and more time with patients.
We've integrated the most popular public domain behavioral health rating scales and assessment tools including:
Start Free Trial - no credit card required!
What are Assessment Tools?
Assessment tools are resources designed to help an individual recognize a need to visit a doctor or for a clinician to use when consulting with a patient. These resources can be in paper or digital format.
Assessment tools use a database of standardized questions to determine an individual's mental health and whether they pose a risk to themselves or others.
This informative overview of evidence-based Behavioral Health Assessment Tools includes a comprehensive list of assessments available in the public domain.
The Purpose of Mental and Behavioral Health Assessments and Screenings
Mental and behavioral health assessments are a valuable tool — but how do they work and what can they do for your practice?
What is a Behavioral Health Assessment?
A behavioral health assessment consists of a series of questions, interviews, and mental and physical examinations that clinicians use to understand patients. Behavioral health assessments are not intended to provide complete diagnoses. Instead, their purpose is to lay the groundwork and better frame your patient's concerns. Both children and adults benefit from the use of behavioral health assessments.
Why are Mental Health Assessments Important?
The information collected through the use of assessment tools offers valuable insight into patient health and provides a starting point for diagnosis and treatment.
Standardized mental health assessment tools provide an opportunity for clinicians to understand their patients better — their struggles, concerns, habits and behaviors. Through the use of assessment tools, you can evaluate these symptoms, behaviors and concerns and compile them to create a personalized profile of their case. Assessment tools allow you to form a big-picture view of your patient's overall well-being.
Mental health assessments also allow both patient and clinician to set and measure goals during treatment.
What Does a Mental Health Assessment Include?
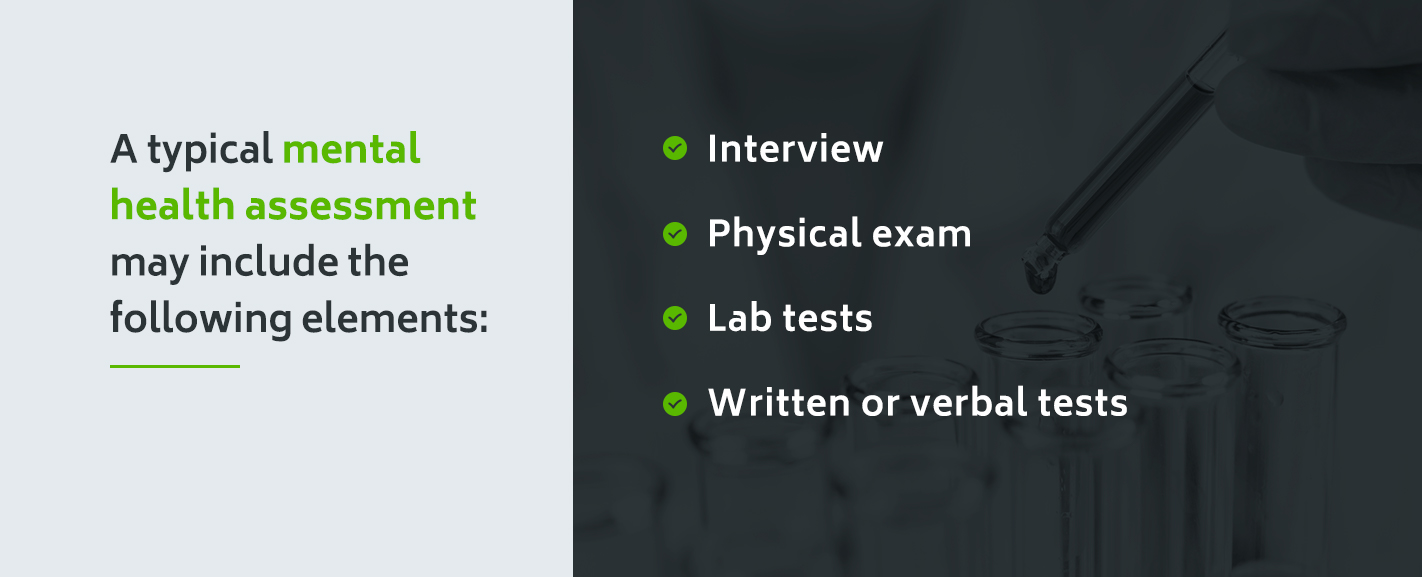
Each mental health assessment you administer will differ based on your patient and their symptoms.
A typical mental health assessment may include the following elements:
- Interview: General interviews allow you to note your patient’s mood and presentation. Asking questions about the patient’s symptoms and concerns, as well as their life situation and thought patterns, can help reveal initial areas on which to focus.
- Physical exam: To help distinguish between symptoms resulting from a mental disorder and symptoms related to bodily illness, you may need to complete a physical exam. Ask about your patient’s personal and family medical history, as well as any medications they may take.
- Lab tests: Some symptoms may prompt the need for lab tests or scans. Blood or urine samples and MRI, EEG or CT scans may be helpful when assessing a patient.
- Written or verbal tests: You may want to administer a test to help identify specific problems, test certain functions or further assess a patient’s well-being.
Mental and behavioral screening tools can help assist and guide your assessments by pinpointing symptoms and providing valuable data. Consider the following factors when selecting a tool:
- Reliability: Does the test have the reliability to produce consistent results?
- Validity: Does the test have the validity to differentiate between a patient with a problem and one without?
- Sensitivity: Does the test have the sensitivity to identify a problem accurately?
- Specificity: Does the test have the specificity to identify individuals who do not have a problem?
Selecting a screening tool that conforms to the above factors will help make your results as accurate and helpful as possible. Disorder-specific assessments are valuable tools when working with patients, but how can you know which areas to test for? Screening tools can be the starting point that illuminates these risk areas.
Watch our On-Demand Webinar on Behavioral Health Assessment Tools
In the intricate web of copyrights, infringement patents, and license fees, many clinicians are unsure of which mental health screening tools are valid, research-verified, and completely free to use. We have done the research for you! In our video, you will learn which assessments are available free for the most common behavioral health disorders.
10 Examples of Assessment Tools
for Mental and Behavioral Health Professionals
Assessment tools can be used to assist patients — young, old, and in between — with several mental and behavioral health concerns. Below are 10 types of mental health tools for adults and children, as well as popular examples from each category.

1. Anxiety
Anxiety assessment tools, such as those listed below, can help identify which type of anxiety your patient's symptoms are most closely associated with, as well as the severity of those symptoms:
- Depression Anxiety Stress Scale (DASS)
- Generalized Anxiety Disorder Screener (GAD-7)
- Hamilton Anxiety Rating Scale
- Zung Anxiety Scale

2. Addiction
There are several tools available for all types of addictions, including addiction to drugs, alcohol and gambling. Useful addiction assessment tools include:
- Addiction Severity Index (ASI)
- Brief Addiction Monitor
- Drug Abuse Screening Test (DAST)
- Alcohol Use Disorders Identification Test (AUDIT-C)
- South Oaks Gambling Screen Assessment

3. Mood Disorders
Because the symptoms of different mood disorders may manifest similar symptoms, assessment tools can be used to help identify which disorder your patient most closely aligns with. For example, the Mood Disorder Questionnaire and the Bipolar Spectrum Diagnostic Scale could be used in tandem to help determine whether your patient is experiencing symptoms of bipolar disorder rather than borderline personality disorder or something similar.

4. Depression
Each patient experiences symptoms of depression differently from one another. Depression screening tools can help you direct sessions or tests toward your patient's specific needs. Two examples of depression assessment tools are the PHQ-9, the Geriatric Depression Scale and the Zung Self-Rating Depression Scale.

5. Personality Disorders
Personality disorder tools include the Borderline Personality Screener, a self-report scale that is used to assess the presence and severity of symptoms of borderline personality disorder in adults. Another personality disorder scale is the International Adjustment Questionnaire which is used to identify individuals who may be at risk for adjustment disorder.

6. Suicide
If a patient is displaying suicidal warning signs, assessment tools like the Columbia Suicide Severity Rating Scale can help gauge the severity of those tendencies.

7. Trauma
Trauma has several sub-categories. Two common tools for diagnosing trauma are the Post-Traumatic Stress Disorder Checklist and the International Trauma Questionnaire, a self-report measure that assesses exposure to traumatic events as well as symptoms of PTSD and depression.

8. Eating Disorders
The Eating Disorder Diagnosis Scale is helpful when handling cases of suspected anorexia, bulimia or binge-eating disorder.

9. Behavioral
Behavioral health assessments are designed to provide a better view of the patient's home life, mental wellbeing, daily activities, habits and more. Data from these assessments can be used to support and make sense of information gathered from other tests. A few examples of behavioral assessment tools are:
- Wahler Self-Description Inventory
- Daily Living Activities
- Parental Stress Scale

10. Children and Youth
Mental health assessment tools are not just for adults. There are many screening tools to assist in the diagnosis and treatment of children and youth. Examples include:
- Revised Children's Anxiety and Depression Scale (RCADS)
- Traumatic Events Screening Inventory for Children (TESI-C)
- Mood and Feelings Questionnaire (MFQ)
- Child PTSD Symptom Scale
- Problem-Oriented Screening Instrument for Teenagers (POSIT)
- Pediatric Symptom Checklist (PSC)
How is a Mental Health Assessment Done?
A mental health assessment typically begins with a patient scheduling an appointment with their general practitioner. The GP will conduct physical examinations and other medical tests.
Once they have ruled out the presence of physical illness, they will then refer the patient to a mental health specialist, who will complete a brief problem checklist and administer further mental health assessment forms.
These tests will be formal and standardized or informal and non-standardized. They can be self-reported assessments completed by the patient or conducted by a therapist.
Some standard formats for mental health assessments are:
✅ Observation ✅ Interview
✅ Family Interview ✅ Checklists
✅ Rating Scales ✅ Questionnaires
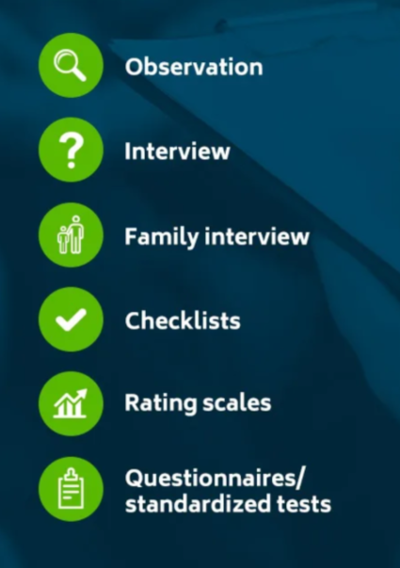
1. Observation
Observation can help you uncover clues to a patient’s condition. Note your patient’s words, actions, expressions and attitudes in various surroundings to develop an understanding of their situation beyond what they communicate. To use this tool well, pay close attention to your patient and observe them with a professional, neutral demeanor.
2. Interview
Psychiatric interviews can help you establish a relationship with your patients and collect information about their symptoms and experiences. Allow your patients to speak without interruption and guide their responses with open-ended questions. Keep diagnostic reasoning in mind while you ask questions. If you want to build trust with your patients, ensure they feel validated and understood. Allowing your patients to present their feelings and experiences can reveal the factors contributing to their symptoms.
3. Family Interview
In some scenarios — especially when working with younger children — you may opt to interview a patient’s family members. Family interviews can provide additional insight into a patient’s condition and help the family better understand what the patient is experiencing. You may want to review the Health Insurance Portability and Accountability Act before getting family members involved.
4. Checklists
Like many screening tools, assessment tools feature checklists to provide insight into a patient’s mental health status. A targeted list can be a quick and efficient way to supplement your knowledge. The DSM-5 contains lists to identify and classify patient symptoms, but you should use these lists with caution. Checklists do not consider all biological, psychological, sociological and cultural variables possible in a patient’s life. However, checklists can be appropriate tools when used in conjunction with other assessment methods.
5. Rating Scales
Rating scales provide numerical data and help patients sort confusing feelings and emotions into simple responses. They can be valuable when working with patients who have difficulty communicating about their illness or as a general assessment tool to determine the severity of symptoms at a given point.
6. Questionnaires/Standardized Tests
Assessment questionnaires function like screening questionnaires, except they often go into greater detail about a specific illness and its severity. If screening test results show the potential for particular disorders, a disorder-specific assessment can help you gather further data. One typical standardized assessment includes the Global Mental Health Assessment Tool, which can screen and assess various mental health issues.
Throughout these assessments, clinicians also take note of a patient's appearance, behavior, attitude, mood, insight, cognition and more. All of the information collected from health assessments and tools can now be used to compile a profile that provides a big-picture view of your patient's mental and behavioral health.
Let ICANotes EHR Software Handle Your Assessment Tools
ICANotes is the only EHR software that actually thinks like a clinician. We help you save valuable documentation time by having all your mental and behavior assessments conveniently linked to your patient records. Our software is always HIPAA compliant and ensures the privacy of your notes, including the prevention of alteration or destruction of your records.
ICANotes Behavioral Health EHR is ideal for any mental and behavioral setting, including:
Contact us today to learn more about what ICANotes can do for your practice or click here to request a free trial of our EHR system.
Assessment Tools Included With ICANotes
We have over 75 mental health screenings and rating scales within ICANotes. Simply navigate to a patient's chart and click the custom forms and assessments option to find the screening tool or behavioral health assessment you wish to complete. It will then be linked to your patient's EHR.
What is the Difference Between a Screening Tool and an Assessment Tool?
At nearly 1,000 pages, the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) contains hundreds of potential disorders you may see in your facility. Administering detailed assessments for all possible problems would be illogical and time-consuming, which is why clinicians use screening tools.
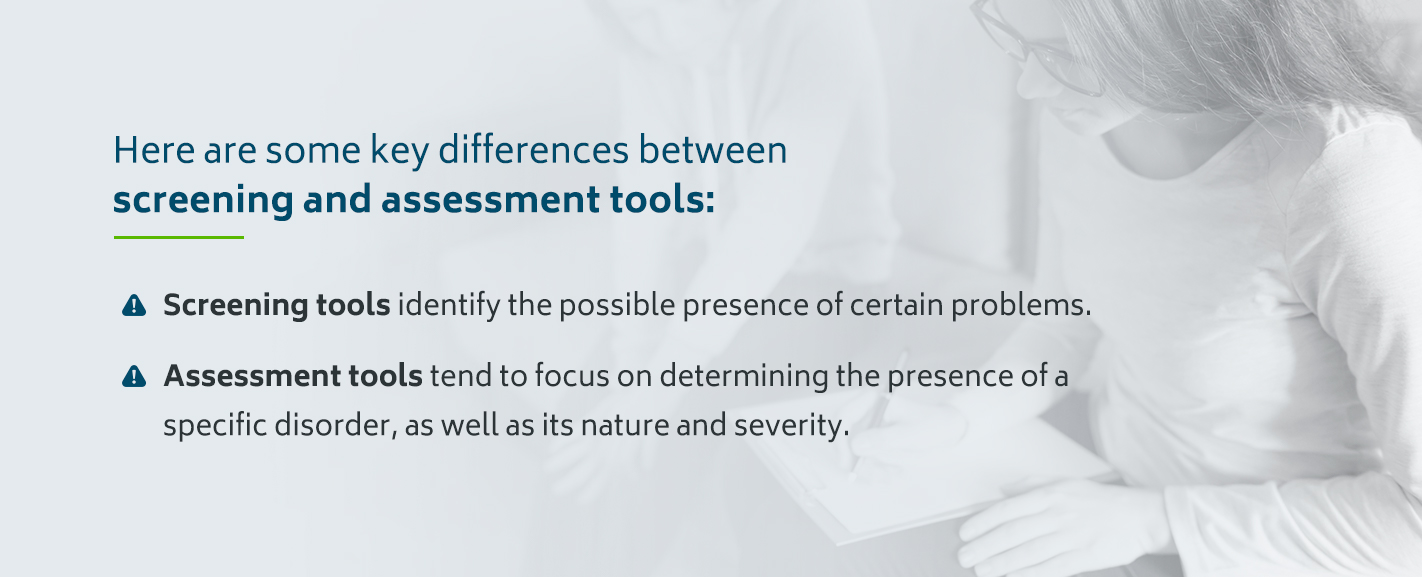
Here are some crucial differences between screening and assessment tools.
- Screening tools identify the possible presence of specific problems: Usually given in a checklist or questionnaire format, screening tests may be broader in scope than assessments. Clinicians typically use screening tools early on when working with a patient to help focus on potential disorders.
- Assessment tools provide a complete picture: Assessment tools tend to focus on determining the presence of a specific disorder and its nature and severity. Clinicians typically use assessment tools to dig deeper into screening results. Assessment tools are available for a range of topics and come in a wide variety of formats.
Mental health screening and assessment tools are beneficial because they help clinicians diagnose and treat patients quickly and accurately. Understanding the different types of screening and assessment tools available allows you to make an informed decision for each patient.
7 Types of Screening Tools for Behavioral Healthcare
The appropriate screening tool depends on your client's self-awareness level and evident symptoms. If mental illness is present in your patient’s family medical history, you may also wish to screen for those disorders.
Here are seven common types of screening tools to consider using:
1. General
In some situations, your patient may not recognize the symptoms and disorders they are experiencing. General mental health screenings like the Kessler Psychological Distress Scale, Patient Stress Questionnaire or My Mood Monitor checklist check for early signs of mental health symptoms. Primary care doctors may also use these screenings during regular checkups to refer at-risk patients to behavioral and mental health specialists.
2. Depression
If your patient shows signs of depression or has a family history of depression, screenings like the Patient Health Questionnaire (PHQ) may help give a more definitive answer.
3. Drug and alcohol use
Screenings for drug and alcohol use may help identify destructive habits or addictions in patients. For example, the World Health Organization’s Alcohol Use Disorders Identification Test checks for hazardous or harmful alcohol use. Other common drug and alcohol screenings include the Drug Abuse Screening Test and the Tobacco, Alcohol, Prescription Medication, and Other Substance Use Tests.
4. Bipolar Disorder
To help identify symptoms of bipolar disorder, clinicians may use the Mood Disorder Questionnaire. Because bipolar disorders exist on a spectrum, it may also help to use the Bipolar Spectrum Diagnostic Scale to determine where or if your patient registers.
5. Suicide Risk
You can help determine if your patient is at risk for suicide by using the Suicide Assessment Five-Step Evaluation and Triage, Columbia-Suicide Severity Rating Scale or Ask Suicide-Screening Questions. To promote your patient’s safety and reduce risk, screening for suicide risk is an essential preventive measure.
6. Anxiety Disorders
Anxiety disorder screening can help you determine if your patient exhibits symptoms of generalized anxiety disorder, obsessive-compulsive disorder, panic disorder, post-traumatic stress disorder (PTSD) or social phobia. Some relevant anxiety screenings include the Generalized Anxiety Disorder seven-item (GAD-7) scale, the Post-Traumatic Stress Disorder Checklist for DSM-5 and the Hamilton Anxiety Rating Scale.
7. Trauma
To screen for potentially traumatic events in your patient’s life, you may use the Life Events Checklist for DSM-5. This tool checks for common sources of PTSD or extreme distress.
Talk to your patient to determine which screenings may be necessary. After you have highlighted areas of concern, you can use assessment tools to understand the depth and scope of individual problems.
Screening Tools for Different Ages
Different age ranges have unique needs regarding screening tools. For example, a young child might lack the vocabulary to describe their symptoms as fluently and accurately as an adult can. They need a screening test they can respond to.
Clinicians must consider how age influences each patient’s ability to express their feelings and experiences and choose screening tools accordingly. Here are recommendations for depression and anxiety screening — two of the most common mental disorders — for various age groups.
Children and Adolescents
According to the Centers for Disease Control and Prevention, 4% of children aged 3 to 17 have received a depression diagnosis. Depression is a risk factor for substance use, suicide, declining academic performance and poor health choices.
Despite depression’s severity, it often goes undiagnosed in young patients, partially because children and adolescents may have difficulty expressing how they feel. In particular, teens might repress their feelings or turn to friends rather than adults for help with depression or anxiety. Fortunately, screening tests help physicians and behavioral health professionals catch depression and anxiety early on, so they can begin treatment.
The U.S. Preventive Services Task Force (USPSTF) recommends that primary care physicians screen adolescents aged 12 to 18 for major depressive disorder if the clinician can ensure an accurate diagnosis and effective treatment. Effective and widely used screening tools for depression in adolescents are the PHQ-9 and the Patient Questionnaire for Adolescents — a slightly modified version of the PHQ-9. You might also use the Kutcher Adolescent Depression Scale to screen for depression in patients ages 12 to 17.
Pediatricians, psychiatrists and other health professionals might use the Pediatric Symptom Checklist, a short questionnaire, to screen for depression and anxiety in children ages 4 to 16. The Child Depression Inventory, a modified version of the Beck Depression Inventory, is another way to screen for depression in children ages 7 to 17. Parents can collect the information to help a young child complete a screening test.
Anxiety is even more common than depression in childhood and adolescence, with 7.1% of children aged 3 to 17 having a diagnosis of this condition. To screen for anxiety in children, you might choose the Spence Children’s Anxiety Scale for patients ages 2 to 12, the Screen for Child Anxiety-Related Disorder for patients aged 8 to 18 or the GAD-7 for adolescents.
Adults
Anxiety disorders affect about 18% of the adult population every year, and half of those diagnosed with anxiety also have depression. Depression and anxiety can make it challenging for people to meet daily responsibilities, maintain relationships and take care of their health. According to the World Health Organization, depression is the top cause of disability worldwide.
Due to the prevalence and severity of depression in adulthood, the USPSTF and American Academy of Family Physicians recommend screening all adults over 18 for depression, regardless of risk factors. PHQs are the most widely used depression screening tools for adults. You might use the PHQ-2 initially and the PHQ-9 or clinical interview if you identify depression.
Physicians should also consider screening for depression in pregnant and postpartum women. Postpartum depression can have a cascade of adverse effects on a child’s development and family relationships. The USPSTF, American College of Obstetricians and American Academy of Family Physicians suggest screening all pregnant and postpartum women for depression. You might use the PHQ-2, PHQ-9, Edinburgh Postnatal Depression Scale or the Postpartum Depression Screening Scale.
To screen for anxiety in adults, consider the GAD-7 or the Kessler Psychological Distress Scale. According to a review published in BMC Psychiatry, both of these tools were the most commonly validated for anxiety disorders.
Older Adults
Screening for depression and anxiety becomes more challenging for older patients. Patients might have a chronic medical condition contributing to a mental disorder and the symptoms they’re experiencing. If a patient has dementia, clinicians must choose an appropriate mental health screening tool.
Anxiety is widespread among older adults, affecting as much as 10 to 20% of the older adult population. Anxiety often goes undiagnosed in older adults because patients and doctors might assume a medical condition or prescription medication causes the condition. Older patients may also be more hesitant to discuss mood disorders with their doctor or think it’s normal to feel that way. If left untreated, anxiety can lead to physical health issues, cognitive dysfunction and a lower quality of life.
Screening tools designed for older adults can help them get treated. You might use the Geriatric Depression Scale, which features yes-or-no questions, to screen for depression in older adults, including patients with cognitive impairment. For patients with dementia, the USPSTF recommends the Cornell Scale for Depression in Dementia. The PHQ-2 is another valuable screening tool for depression in older patients.
The Geriatric Anxiety Scale is a widely used anxiety screening and assessment tool for older adults. According to a 2019 systemic review, the Rating Anxiety in Dementia scale is a validated screening tool for anxiety symptoms in patients with dementia.
Does Your EHR Support Your Needs?
Behavioral and mental health screening and assessment options exist to help you make informed decisions as you work with patients. Using the right tools can help maximize your appointments and help you provide the best care possible.
When your screening and assessment tools integrate into your EHR, you’ll be able to track your patient’s data in one secure location. ICANotes can help keep your office organized with an intuitive EHR built with a behavioral and mental health professional in mind.
For more information about our mental health screening and assessment tools, therapy note templates, and EHR best practices, contact us today!
Why Trust Us for Mental and Behavioral Health Assessment Tools?
ICANotes software thinks like a clinician because our company was co-founded by a clinician. He saw how writing the same repetitive information robbed him of time he could spend with patients.
Mental health screenings and assessments are essential — especially when they don't hamper your workflow. That's why we've integrated these tools into the ICANotes chart-centric workflow. With the push of a button, we've given you access to a comprehensive list of electronic rating scales and assessment tools for adults and children that can seamlessly link to your patients' charts.
Since 1999, we've listened to our peers and adapted, assembling features to streamline your practice. The result is a fully configured EMR that we know will eliminate the stress caused by redundant administrative burdens.
Sign up for Your Free Trial of ICANotes
Ready to optimize your EHR with mental and behavioral health assessment tools linked to your patient records? ICANotes is designed to optimize your documentation and compliance with convenient screening tools within our digital charting solution.
For more information about our mental health screening and assessment tools, therapy note templates and EHR best practices, sign up for your free trial.
Posts Related to Mental Health Assessment Tools
Valerie Barfield
APRN, GNP-BC, Sage Lifecare, Memphis, TN
"ICANotes creates a narrative note that is readable and thorough. I get lots of compliments on my documentation and I feel more confident in my coding.”
Intuitive, Accessible, Time-Saving
ICANotes - the only EHR software that actually thinks like a clinician.