Blog > Documentation > Guide to Creating Mental Health Treatment Plans
Guide to Creating Mental Health Treatment Plans
This comprehensive guide walks behavioral health professionals through every aspect of creating effective mental health treatment plans, from setting goals and objectives to ensuring compliance and insurance reimbursement. Learn how to streamline your documentation process, improve patient outcomes, and build collaborative, personalized plans with practical templates and proven strategies.

Last Updated: June 20, 2025


What You'll Learn
- How to create personalized, goal-oriented treatment plans that improve patient engagement and outcomes
- The essential components of an effective treatment plan, including goals, objectives, interventions, and timelines
- Best practices for writing SMART goals and collaborating with clients during the planning process
- Tips for staying compliant with documentation and insurance requirements using templates and structured formats
Contents
- What Is a Mental Health Treatment Plan?
- What Is the Purpose of a Treatment Plan?
- Mental Health Treatment Plan Goals and Objectives
- How to Write a Treatment Plan for Mental Health
- Key Considerations for Creating Personalized Mental Health Treatment Plans
- Mental Health Treatment Plan Tips
- How a Mental Health Treatment Plan Complements Other Therapy Notes
What Is a Mental Health Treatment Plan?
A mental health treatment plan is a structured personalized document that outlines a patient's clinical needs, therapeutic goals, and strategies for achieving meaningful progress. Treatment plans are an effective tool for improving patient engagement in their treatment because they outline their current struggles and how they will overcome them with a therapist's help. While treatment plans vary depending on a patient's needs, they typically follow the same general format, which includes:
- Their personal, demographic and insurance information.
- Their psychological history, if necessary.
- Their current mental health diagnosis or condition.
- A timeline to monitor their progress.
- High-priority goals to achieve during treatment.
- Clear and measurable objectives that are relevant to their goals
What Is the Purpose of a Treatment Plan?
A mental health treatment plan, sometimes called a therapy or psychotherapy treatment plan, aims to help patients achieve their goals by relieving symptoms and helping them overcome the challenges they're experiencing in their initial treatment session. Treatment plans also help behavioral health professionals, like counselors, monitor a patient's progress and determine if treatment adjustments are necessary.
Without a treatment plan, it may be difficult for patients to visualize the path they need to take to reduce their negative thinking patterns or improve their habitual behaviors. Lacking this structure can make it more difficult for patients to set and accomplish their therapy goals. Goal-setting is a significant treatment plan component that contributes to the effectiveness of a mental health intervention. Setting goals in a treatment plan helps patients:
- Feel motivated.
- Focus their efforts.
- Boost their self-esteem.
- Engage with their treatment.
- Feel a sense of accomplishment.
- Concentrate on their priorities.
- Avoid distraction.
Treatment plans are also a valuable tool for clinicians, providing a clear framework that supports consistent, high-quality documentation. Treatment plans contain essential information about a patient's progress in a clear and organized format, with measurable goals and target completion dates. With this information readily available, documenting progress toward goals in each individual session note becomes an easier part of the job.
Mental health treatment plans are individualized roadmaps that behavioral health professionals use to help patients focus on meeting their goals. These plans help clinicians stay organized and record patient progress during treatment. An effective treatment plan empowers behavioral health counselors to deliver comprehensive care to meet each patient's needs.
In addition, mental health treatment plans make it easier for therapists to monitor a patient's growth and healing between sessions to determine if they need to make therapeutic adjustments. While creating a treatment plan isn't a requirement for all mental health professionals, it leads to more effective outcomes and benefits both the provider and the patient.
Learn everything you need to know about mental health treatment plans and how they can transform your normal therapeutic procedures.
Download Our Guide to Writing Better Mental Health Treatment Plans
Simplify treatment planning, avoid common mistakes, and stay compliant with practical templates, proven formats, and time-saving strategies to create effective, personalized plans that support better outcomes.
Mental Health Treatment Plan Goals and Objectives
Using a treatment plan is an effective way for therapists to engage patients in their care by collaborating on meaningful, personalized goals. These goals reflect the patient’s core challenges and aspirations, providing a roadmap for progress. Within the treatment plan, clinicians also define specific, measurable objectives that support each goal—creating a shared vision for the therapeutic journey.
Examples of Goals to Include
Treatment goals are broad, overarching outcomes that reflect what the patient hopes to achieve by the end of the therapeutic process.
Consider these examples:
- Managing negative emotions and feelings without turning to substances
- Learning interpersonal skills to communicate positively with others
- Learning healthy emotional management skills
- Establishing coping strategies for stress
- Reducing the frequency and severity of mood swings
- Managing hallucinations or delusions
- Improving self-care behaviors and habits
- Boosting self-esteem
Examples of Objectives to Include
Think of an objective as a rung on a ladder that gets the patient closer to their goals. Objectives tend to be smaller, specific tasks or skills a patient must accomplish to reach their larger treatment goals. These tasks should be clear and measurable, giving the patient direction toward their goals. For example, you may record objectives like:
- Attending substance abuse meetings to help with sobriety.
- Keeping a journal of daily communication to help develop effective communication skills.
- Taking antidepressant medication and attending therapy to reduce depression symptoms.
- Initiating conversation in social situations.
- Establishing a daily routine.
- Incorporating physical activity and proper nutrition.
- Following a consistent sleeping schedule.
Simply said, an objective is a specific way to reach a goal.
Common Goals Set in Mental Health Treatment
Because every patient presents with unique challenges and circumstances, their treatment goals and objectives should be tailored to their individual needs. When a patient is motivated to make changes but unsure where to begin, establishing a few initial goals can help provide structure and direction for their therapeutic journey.
A few goals to consider during mental health treatment include:
- Avoiding substance use.
- Building a supportive group of loved ones.
- Learning better communication skills.
- Confronting fears and anxieties.
- Managing depression symptoms.
- Overcoming symptoms of trauma.
- Developing stress relief techniques.
- Managing and reducing anxiety attacks.
- Reducing thoughts of suicide.
Once these goals are set, you and your patient can work on specific actions — or objectives — that can back up these overarching goals.
For instance, if a patient has extreme anxiety when leaving the house, they could set a goal of walking 30 steps outside their front door. Eventually, they can work up to going to the grocery store or practicing daily walks around the neighborhood. If your patient has difficulty interacting with others in a social setting, they may set a goal of talking to one new person each week or joining a club to practice conversing with others regularly.

How to Write a Treatment Plan for Mental Health
Writing an effective mental health treatment plan begins with gathering the right information through a two-step intake process: screening and assessment. During the initial screening, clients typically share a brief overview of the concerns that led them to seek therapy. This step helps you identify their presenting problems and determine whether further evaluation is needed. Once you’ve established a general understanding of their condition, the next step is to conduct a comprehensive biopsychosocial assessment to explore the nature, severity, and underlying factors contributing to their symptoms.
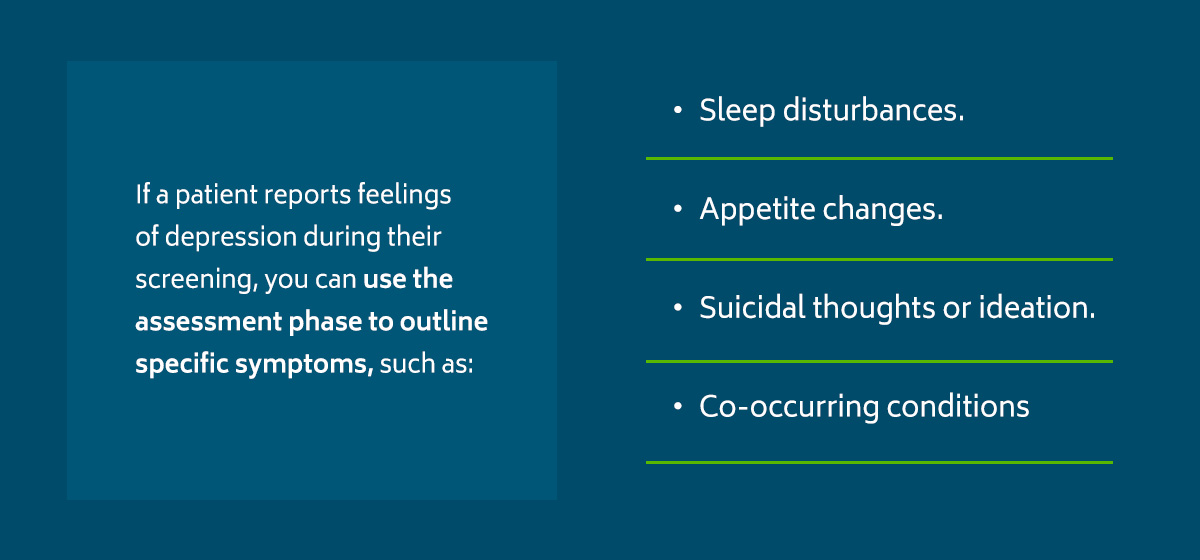
For example, if a patient reports feelings of depression during their screening, you can use the assessment phase to outline specific symptoms, such as:
- Sleep disturbances.
- Appetite changes.
- Suicidal thoughts or ideation.
- Co-occurring conditions like anxiety or substance abuse.
After a detailed assessment and discussion with your client, you'll be ready to draft a treatment plan tailored to their specific needs. At this time, you'll also need to identify and discuss possible goals with your client. Consider this last step a collaborative process — ensure that the goals outlined in the treatment plan are agreeable and realistic.
For example, if your patient reports severe social anxiety, a reasonable goal might be to manage physical symptoms of anxiety, such as a rapid heartbeat or shaking hands. This is an achievable starting point that will likely make your client feel more motivated to follow through with their therapeutic assignments.
Once you've created your treatment plan, you and your client must both sign the document. This demonstrates that you and your client agree on the treatment plan, including its goals and objectives. Keep in mind that treatment planning, just like therapy, is an ongoing process. You'll review and revise the treatment plan as needed because nothing is written in stone. A mental health treatment plan template will help you stay organized, but its information is unique to the client and open to changes.
Therapy Treatment Plan Template
Treatment plans are designed to be simple but specific to each individual and their needs. While every treatment plan will vary slightly depending on the patient's reason for seeking mental health treatment, a treatment plan template or document will generally contain the same categories, which include:
- Patient information: The first thing counselors should include in any treatment plan or document is any required patient information, such as their name, demographic details, insurance details emergency contacts and other relevant information.
- Diagnostic summary: The therapist should then include details about the patient's current diagnosis, past diagnoses and treatment history. Include information about the patient's current mental state or condition, if possible.
- Problems and goals: The treatment plan should include measurable objectives, issues and goals that allow the counselor and patient to track progress. Each of these categories should include a timeframe or deadline for completion. Aim for at least three or four goals.
- Signatures: In the final part of the treatment plan, the provider and patient must sign and date the document. Having the patient sign the form shows they know their treatment timeline and goals and that they participated in and agreed with the content.
Mental Health Treatment Plan Checklist
Your treatment plans should be thorough while only including relevant details. For many behavioral health professionals, it can be challenging to determine what details to include in a treatment plan. To avoid missing any crucial details, use this checklist as a helpful reminder:
- Issues: Do the issues reflect the six problem domains— medical status, employment, substance abuse, legal status, family or social status and psychiatric status? Are issues written in behavioral terms and a non-judgmental manner? Are they prioritized?
- Goals: Do the goals address the listed issues? Are they attainable during treatment? Does the patient understand the goals as written? Does the client seem ready to change and accomplish the goals?
- Objectives: Do the objectives address the goals? Are the objectives measurable and specific? Can the client take the time or steps necessary to complete objectives? Is there a timeframe for the objectives? Are they realistic for the patient's current situation? Does the client understand what is expected of them?
- Interventions: How will the counselor help the patient achieve their goals? What specific techniques and exercises align with the patient's emotional and physical circumstances? Is the patient ready to engage in the necessary steps toward their goals? Are they willing to accept and participate in the interventions and treatment options?
- Treatment modality: Does every goal have an applicable treatment modality? Does the treatment plan outline a frequency of sessions for reaching these goals and an anticipated completion date that can be measured?
- General: Is the treatment plan customized to suit the patient based on their unique skills, goals, lifestyle, educational background, culture and socioeconomic status? Are their strengths incorporated into the treatment plan? Has the patient participated in developing the plan? Does the plan contain the date and the patient's and counselor's signatures?
Mental Health Treatment Plan Insurance Requirements
As a behavioral health clinician, you have many clients to see and a long list of administrative tasks to manage. But if your treatment plan or therapy documentation contains missing or inaccurate information, it can lead to under-coding or denied insurance claims. Many therapists use the treatment plan as concrete justification for each session when billing insurance, so it’s essential to ensure everything is complete and accurate.
Though every insurance company has varying requirements, here's a brief overview of the general factors that demonstrate your patient's medical need for treatment:
- A current diagnosis/comorbid diagnoses
- Medications and dosages
- Severity and duration of symptoms
- Problems with daily functioning
- Risk factors, if any
- Treatment goals
- Objectives for reducing specific symptoms or behaviors
- Measurable outcomes
- Frequency of sessions
- Therapeutic interventions and modalities
- A timeline for patient progress
Here's another tip — when discussing your client's therapy goals, be sure to note how they will address specific medical symptoms rather than just achieving self-improvement. For instance, instead of stating that your client's goal is to improve their agoraphobia, you might say the goal is to decrease dizziness, fast heart rate and choking sensations when in an unfamiliar environment. Then, outline how the therapy treatment plan will help your patient achieve this.
Insurance companies look for evidence that treatment is a "medical necessity." If you have these elements included in your treatment plan, there's a good chance you've covered all your bases and will demonstrate that your client still requires treatment.
Key Considerations for Creating Personalized Mental Health Treatment Plans

Every patient brings a unique set of experiences, symptoms, and strengths to the therapeutic relationship, regardless of their diagnosis. A well-structured treatment plan helps clinicians stay organized, focused, and aligned with each patient’s specific goals and care needs.
To develop effective, individualized goals and objectives, consider these key factors that influence treatment planning:
-
Current Mental Health Status:
Assess the nature, duration, and severity of the patient’s symptoms or presenting concerns. Their current mental and emotional state should directly inform the pace and intensity of treatment. -
Strengths and Support Systems:
Identify personal strengths such as resilience, insight, or coping strategies as well as external resources like family support, community engagement, or stable housing. These assets can serve as building blocks toward recovery. -
Readiness for Change:
A patient’s motivation level can influence the success of any intervention. Tools like the Transtheoretical Model of Change can help determine where a client falls along the continuum, from precontemplation to maintenance, and guide realistic goal-setting. -
Cultural and Social Context:
Treatment plans should reflect the patient’s cultural identity, values, language preferences, and community experiences. This ensures goals are both respectful and relevant, increasing engagement and therapeutic alliance. -
Holistic Care Needs:
Mental health doesn’t exist in a vacuum. Consider incorporating goals related to physical health, social relationships, emotional regulation, and even spiritual well-being to support the patient’s overall functioning.
By thoughtfully addressing these factors, you can avoid generic plans and instead create treatment strategies that are meaningful, measurable, and truly patient-centered.
Mental Health Treatment Plan Tips

There are no set rules for developing a treatment plan for your patient because every plan is unique. Typically, you'll start with a mental health treatment plan template and modify it as necessary for your patient. Creating a mental health treatment plan can feel daunting, so here are a few best practices to help you through setting goals and planning.
1. Measure Success
To evaluate the effectiveness of the treatment plan, you track how the patient is doing. You can monitor their progress more effectively by asking them to record their thoughts, feelings and behaviors in a journal or document. Self-reports can give you a better glimpse of your patient's state of mind between sessions and over time.
You should also note observations and signs of improvement or decline during your sessions. For example, you may notice your patient has more relaxed body language each time you see them, indicating signs of improvement. As you measure your patient's success, you'll determine whether your treatment plan is effective or needs adjustments.
2. Set SMART Goals
Your patients may become overwhelmed if you set goals and objectives that are too challenging or far outside their comfort zone. For treatment to be effective, yet motivating for your patients, work with them to set goals they can actually reach. To do this, use SMART goals as a template for creating clear, realistic goals that guide them toward their intended accomplishments. SMART stands for the following:
- Specific: Goals should be clear and explicit. Set goals with plain language and strong verbs so your patient knows exactly what to do. Patients with specific goals will be able to complete them more effectively than goals that are too general or vague.
- Measurable: Goals with specific dates, times or amounts are easier to track and monitor. For instance, goals like completing an assigned task within two weeks or reducing the number of times they use substances within a month are easy to monitor.
- Attainable: Patients should be able to realistically meet their goals. This may require thorough conversations with your patient to determine what limitations may hold them back from certain goals. They will likely feel discouraged and defeated if their goals are too difficult or unreasonable from the start.
- Relevant: Goals and objectives should relate to the patient's individual needs outlined in the treatment plan. Consider what goals would help a patient reach their expected treatment outcomes and how they're relevant to the patient's progress.
- Time-bound: Deadlines make it easier for patients to feel motivated. These can be short- or long-term goals as long as they have a specific end date. For instance, a counselor may ask a patient to choose and join a community event or club by the end of the month to help with their anxiety. Time-bound goals also make measuring progress easier and hold the patient to the goal rather than seeming never-ending.
3. Set Goals That Motivate
Patients are more likely to complete objectives and work toward reaching a goal if the goal is personally important to them. Help your patients set goals that they have personal stakes in so they're motivated to make it happen. If a goal does not add value or meaning to their life, they will not have the motivation to work through objectives.
Ask patients to discuss goals that are meaningful to them. Make sure the goals are in order of importance so patients can focus on their priorities.
4. Use the Right Language
Adequately describing your patients' conditions and progress is essential to creating an effective treatment plan. Therapists often use various power phrases and words to describe their patients, though it's important to consider the emotion behind your word choice. For example, “obsessive” and “all-consuming” can be used synonymously in many cases, though the two words carry different connotations. Despite having the same meaning, describing someone or something as “obsessive” sounds more negative.
As a therapist, it's essential to maintain unbiased diagnoses and treatment plans. Using the right language can make a big difference in how you perceive a patient and how they perceive themselves. When creating your mental health treatment plans and other patient notes, consider your word choice and where you may use synonyms to elicit different emotions with your words.
5. Collaborate With Patients
A client-centered approach to treatment — one that involves your patients in the treatment plan process — is important for making them feel like an active participant in their own treatment. Let your patient know that you're on the same team and will use the treatment plan as a roadmap to their improvement or recovery. You might start by gathering information about their hopes, aspirations, concerns and expectations for treatment.
When you invite patients to collaborate with you in creating the treatment plan, you demonstrate that you value their thoughts and opinions. Seek their input throughout the treatment process to better understand them and their struggles.
Trust is also important between therapists and patients, so give your patient time to open up and engage as the treatment plan progresses. Giving them a say can prompt them to feel seen and understood, which can promote trust. Be sure to always consider their comfort level and preferences with therapy interventions or assigned tasks.
6. Leverage Templates
Proper documentation, organization and maintenance of behavioral health records are essential for ensuring accuracy, protecting patient confidentiality, providing comprehensive care and maximizing reimbursement. However, documenting notes by hand can take up a significant amount of your time, potentially leaving you stressed or frustrated. If you have a full caseload, capturing the same necessary details can feel demanding and repetitive.
With intuitive templates, you can benefit from effective treatment planning in much less time. Prebuilt note templates for all behavioral health disciplines and settings enable you to customize a treatment plan to your individual patient's needs. In addition to treatment plans, these templates can produce comprehensive initial assessments, progress notes and discharge summaries for a holistic view of care.
How a Mental Health Treatment Plan Complements Other Notes
A mental health treatment plan not only supports the patient’s progress but also strengthens collaboration across the behavioral health team. It promotes consistent communication among clinicians, ensures alignment of care goals, and provides essential documentation for reimbursement and regulatory compliance. As a core component of the patient’s medical record, the treatment plan also plays a vital role in meeting federal and state documentation standards. Below, we’ll explore how the treatment plan complements other key clinical records, including the initial evaluation, progress notes, and discharge summary.
1. Psychiatric Evaluation or Biopsychosocial Assessment
The initial psychiatric evaluation, or a comprehensive biopsychosocial assessment, serves as the foundation for understanding a patient’s mental health status. It involves gathering detailed information about the patient’s presenting concerns, history, behavior, thought processes, and functioning. This process often leads to a formal diagnosis, which informs the direction of care.
The treatment plan builds directly on the findings of the evaluation. It translates the diagnostic insights into a structured, goal-oriented roadmap for care. Each treatment goal and objective should clearly correspond to specific concerns identified during the assessment—ensuring that interventions are both relevant and measurable.
By linking the treatment plan to the initial evaluation, clinicians create continuity in care and make it easier for all providers on the care team to reference key information. A standardized treatment plan template further supports this process by promoting consistency, clarity, and compliance in documentation.
2. Progress Notes
Progress notes and treatment plans work in tandem to document and guide the course of care. While the treatment plan outlines the patient’s goals and objectives, progress notes capture the day-to-day movement toward those targets to provide a clinical narrative of what is working, what’s changed, and what needs adjustment.
Because progress notes often reference one or more specific treatment objectives, a well-structured treatment plan ensures that each note is purposeful, focused, and aligned with broader care goals. This alignment also helps meet insurance documentation standards and supports timely, accurate reimbursement.
For busy therapists and counselors managing multiple clients, progress notes serve as a valuable record of where each patient is in their therapeutic journey. They make it easier to pick up where the last session left off and track both short-term progress and long-term outcomes.
A typical progress note includes:
-
The treatment goals or objectives addressed in the session
-
Any changes in the patient’s condition or presentation
-
The patient’s response to interventions
-
Clinical observations and insights
-
The outcome of the session and next steps
A clearly defined treatment plan streamlines this process, making it easier to write defensible notes that reflect the patient’s progress and the therapist’s clinical reasoning.
3. Discharge Summary
A discharge summary is a critical document completed when a patient concludes treatment. It provides a comprehensive overview of the care delivered, the patient’s progress, and recommendations for ongoing support or follow-up services. A well-structured treatment plan serves as a valuable reference point during this process—helping clinicians accurately document the course of treatment and the rationale for discharge.
By reviewing the goals and objectives outlined in the treatment plan, clinicians can efficiently summarize interventions provided, assess how the patient responded to care, and demonstrate clinical improvement. This ensures the discharge summary reflects not just the end of care, but the progress made throughout the therapeutic journey.
Since many patients engage in treatment over extended periods, the treatment plan also functions as a visual timeline, making it easier to track symptom reduction, behavior change, and functional gains over time.
A discharge summary may include:
-
A summary of the patient's presenting problem(s) and diagnosis
-
Treatments and interventions provided
-
The patient’s progress toward each treatment goal
-
Clinical observations at discharge
-
The reason for discharge (e.g., goals met, patient decision, referral)
-
Recommendations for aftercare or continued services
Example summary statements:
-
The patient reports no longer experiencing suicidal ideation.
-
The patient demonstrates improved coping strategies for managing depression.
-
Mood is stable, with no current signs of depression, anxiety, or psychosis.
-
The patient expresses confidence in communicating effectively with others.
-
Behavior is appropriate, with no signs of delusions or hallucinations.
Using the treatment plan to inform discharge documentation helps ensure accuracy, compliance, and a smooth transition to the next phase of care.
Why Trust ICANotes for Treatment Planning?
In today’s fast-paced clinical environment, behavioral health providers need tools that reduce administrative burden without compromising care quality. That’s why ICANotes was purpose-built by behavioral health clinicians to streamline documentation while supporting clinical best practices. From treatment plans to progress notes and discharge summaries, our software is designed to make your workflow faster, more accurate, and more compliant.
With decades of combined experience in the mental health field, our leadership team understands the challenges clinicians face. Every feature in ICANotes reflects that firsthand insight, resulting in a platform that simplifies documentation while enhancing clinical clarity and defensibility.
Don’t just take our word for it, our customers consistently highlight how ICANotes helps them document more efficiently, improve reimbursement accuracy, and navigate audits with confidence. They also appreciate our responsive technical support and intuitive interface tailored specifically for mental health workflows.
Simplify Treatment Planning with ICANotes
ICANotes is designed to take the guesswork and repetition out of treatment planning—so you can create high-quality, personalized plans in less time. Our behavioral health EHR features pre-configured templates and clinically relevant content that align with best practices for goal-setting, compliance, and documentation standards.
In only a few steps, you can identify key problem areas, create SMART goals with clear objectives, and seamlessly link them to billing codes and session documentation. Guided prompts help you cover diagnostic requirements, monitor progress, and demonstrate medical necessity, so you don’t have to build everything from the ground up or risk overlooking important details.
Whether you're treating a new client or updating a long-term care plan, ICANotes gives you the structure and flexibility to document clearly and efficiently—so you spend less time writing and more time delivering care.
See how ICANotes can help you streamline treatment planning without compromising quality or compliance—start your free trial or schedule a live demo today.
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
Simplify clinical charting
Stay organized with appointment scheduling
Reduce no-shows with automated reminders
Improve client engagement with a secure patient portal
Provide flexible care with HIPAA-compliant telehealth
Frequently Asked Questions
Dr. October Boyles is a behavioral health expert and clinical leader with extensive expertise in nursing, compliance, and healthcare operations. With a Doctor of Nursing Practice (DNP) from Aspen University and advanced degrees in nursing, she specializes in evidence-based practices, EHR optimization, and improving outcomes in behavioral health settings. Dr. Boyles is passionate about empowering clinicians with the tools and strategies needed to deliver high-quality, patient-centered care.


