Creating a Depression Treatment Plan
As a behavioral health professional, it's crucial to know how to create a depression treatment plan that shows insurance companies you provide the best care possible to your clients. You'll also want to demonstrate that your client is improving to justify the treatment.
Even if you don't accept insurance, it's still a good idea to create treatment plans for depression with your client to help them meet goals. Overall, treatment plans help you get reimbursed for your services and enable you to put your talents to use. This post will show you how to write a treatment plan for depression and how ICANotes can help reduce your documentation burden. We've also included a downloadable sample treatment plan for depression.
Depression is a prevalent mental health disorder and one of the primary causes of disability. A growing number of Americans face depression every day. According to the 2023 Gallup National Health and Well-Being Index, the percentage of adults who have been diagnosed with depression in their lifetime has reached 29%, nearly 10 percentage points higher than in 2015. Symptoms of depression include persistent feelings of sadness or hopelessness, which can significantly impact a person's life and ability to function.
Fortunately, depression is treatable with therapy and, in some cases, antidepressants. A depression treatment plan is a vital component of effective treatment because it guides the counselor and client toward reaching goals and tracking progress. Depression treatment plans may also be necessary to get reimbursed by insurers. These plans help prove a client's therapy is medically necessary and that the treatment is a clinically appropriate service that helps them overcome depression symptoms.
Download a Sample Treatment Plan for Depression
What is a Depression Treatment Plan?
A depression treatment plan is a detailed, individualized strategy created to help clients reach goals and overcome depression. It's an essential tool in getting clients engaged with their treatment.
In general, treatment plans follow a simple format and include a client's goals, measurable objectives and a timeline for progress. They're a roadmap to provide clients with clear directions on how to get to an improved condition. Treatment plans can also give clients a sense of accomplishment and strengthen the therapeutic relationship.
A depression treatment plan focuses specifically on treating depression and relieving related symptoms. However, since counselors tailor treatment plans to each person under their care, a depression treatment plan might also include goals related to co-occurring disorders, such as anxiety or substance use disorder. The treatment plan must focus on the client's priorities and immediate areas of need to build trust and increase their motivation. You and your client will collaborate when writing the treatment plan and adjust accordingly as they progress and symptoms change or improve.
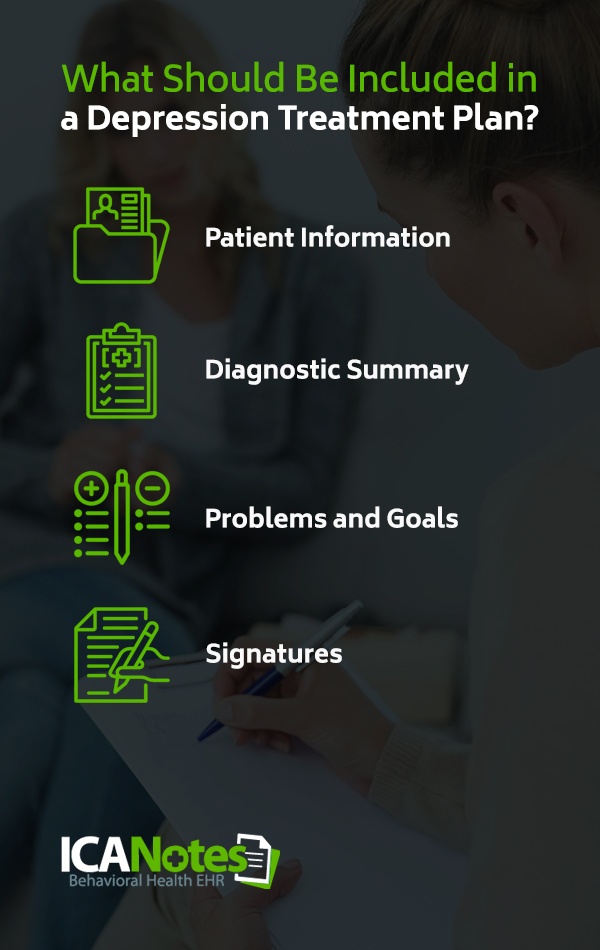
What Should Be Included in a Depression Treatment Plan?
Behavioral health practices have unique templates for creating treatment plans, whether they see clients with depression or other mental health issues. Still, most treatment plans include information needed to justify the services provided and guide clients toward reaching mental health goals. Here's what to put in a depression treatment plan.
1. Patient Information
A depression treatment plan should begin with the client's personal information, such as their name, date of birth and insurance plan. You might also write down the date you created or reviewed the treatment plan at the top of the document.
2. Diagnostic Summary
The diagnostic summary is a complete and accurate description of a client's diagnosis. In your description, note the client's symptoms, how long they've been experiencing them, and their intensity. It's crucial to list all the client's current mental health diagnoses because a dual diagnosis can impact depression treatment.
For insurers to consider treatment medically necessary, the client must have a diagnosis as defined by the current Diagnostic and Statistical Manual of Mental Disorders. During a treatment review, insurance companies will ensure the client's symptoms match their diagnosis.
3. Problems and Goals
Clearly describe the client's current problems and list specific symptoms. You might also include how the client's symptoms interfere with daily functioning and impair their ability to work, study, or maintain relationships. If an event has led to the patient seeking treatment for depression, write a brief description.
The treatment plan for depression should also contain the client's long- and short-term goals. Each goal should directly correspond with a problem and reflect something the client wants to change in their life. Ensure short-term goals consist of specific and measurable objectives aimed to accomplish long-term goals and relieve depression symptoms.
For example, a client with depression might have the long-term goal of reducing the frequency and intensity of depression symptoms to improve daily functioning. If the client struggles to get out of bed due to depression, they might set a short-term goal of starting their day earlier and creating an objective to get out of bed at 8 a.m. every morning.
To help keep clients motivated, you should also include target dates for completing goals.
4. Signatures
Ensure the depression treatment plan includes your and your client's signatures to prove that your client participated in developing their treatment plan and agrees with the problems and goals listed in the document.
Download our Guide to Writing Effective Treatment Plans
Setting SMART Goals for Depression Treatment Plans
Many mental health experts recommend setting SMART goals as part of a successful depression treatment plan. SMART goals provide a clear path to follow, so clients understand what they need to do to progress and find relief from depression. The acronym SMART stands for the following.
- Specific: Once a client has defined goals, it's time to set objectives to help them reach their goals. Objectives describe the actions your client needs to take or skills they need to learn to reach their goals. Objectives should be clear and specific. For example, if a client wants to experience depressed moods less often, they might aim to replace negative self-talk with positive self-talk.
- Measurable: Objectives need to be measurable in some way, so you and your client can gauge their progress. For instance, if the client aims to practice positive self-talk, they might measure this objective by completing a depression questionnaire once a month and see if their score decreases.
- Achievable: Help clients set goals and objectives they can realistically meet within a given timeframe. If targets are too demanding or unrealistic, clients can become discouraged and unmotivated to continue treatment. Focus on a client's strengths, resources and motivation levels when setting achievable goals and objectives.
- Relevant: Goals and objectives should relate to the client's depression and the symptoms they're experiencing. The goals should also be meaningful to the client and seem worthwhile.
- Time-bound: Make sure your client's objectives have deadlines to create a sense of urgency and keep them motivated. While goals can be short- or long-range, objectives should include specific dates for completion.
Some of your clients might know what they want out of treatment, while others may need assistance identifying goals. If your client doesn't know what SMART goals to set, you can help them determine what's most valuable to them. To get started, consider the following questions:
- Why are you seeking treatment?
- What are your symptoms?
- How has depression impacted your life and relationships?
- What do you hope to gain from therapy?
- What are your dreams?
- What are your top priorities?
- What thoughts or behaviors exacerbate depression symptoms?
- What barriers do you need to address to reach your goals?
- What can you do differently to change harmful behaviors?
- Are you capable of meeting specific goals on your own?
- What can your therapist do to help you reach goals and objectives?
It's essential for every client to understand what they hope to accomplish with therapy when creating their treatment plan. Pay close attention to the specific issues your clients wish to address.
For example, imagine you have a client named Mary. Mary has received a major depression diagnosis and has trouble sleeping. While depression has also made it challenging for her to go back to work, her priority is to improve her sleep quality. With this example, you'll want to help Mary set objectives that will help her reach her goal of sleeping better because it impacts other critical areas of her life. You might begin treatment by suggesting she keep a sleep journal, so you and Mary can measure the quantity and quality of her sleep and identify any unhealthy habits she needs to address. Depending on a client's goals, you may need to coordinate care with other health professionals.
By creating a client-focused treatment plan, you'll help clients stay engaged and more committed to treatment. Overall, this can improve treatment outcomes and client satisfaction.
Therapies to Include in Depression Treatment Plans
Therapy can help clients overcome barriers that are keeping them from reaching SMART goals. Depending on the client and your background, you might blend therapy methods to meet their unique needs. You can include a brief, but specific, description of the techniques or interventions used beneath the client's objectives on their treatment plan. Here are some common forms of therapy used to treat depression.
Cognitive Behavioral Therapy
Cognitive behavioral therapy (CBT) is one of the most evidence-based interventions for depression treatment. CBT focuses on identifying and changing negative thinking patterns and behaviors that maintain depression. CBT also aims to help clients recognize irrational thinking and look at their problems and concerns more realistically.
With CBT, you'll work with your clients to list specific problems and set goals to relieve depression-related symptoms that impair functioning. You can address several issues contributing to depression with CBT, such as job stress or relationship issues. You might use CBT to reduce depression symptoms as an independent treatment or in addition to medications.
Mindfulness-Based Cognitive Therapy
Mindfulness-based cognitive therapy (MBCT) combines mindfulness practices, such as breathing exercises and meditation, with elements of CBT. With MBCT, you can help clients change their relationship with negative emotions and break harmful thought patterns before they cause a depressed state.
Dialectical Behavior Therapy
Dialectical behavior therapy (DBT) aims to help clients regulate their emotions and accept uncomfortable feelings. Like MBCT, you might teach clients mindfulness techniques along with skills for coping with challenging situations. DBT can also treat other conditions a client has, such as an eating disorder, substance use disorder or post-traumatic stress disorder.
Psychodynamic Therapy
Psychodynamic therapy explores negative thinking and behaviors that originated in life experiences. During a psychodynamic therapy session, you'll ask the client questions and identify patterns in their responses. You'll help them understand how their experiences have created feelings, thoughts and behaviors that contribute to their depression. From there, you can develop goals with your client to overcome these behaviors and emotions.
Interpersonal Therapy
Interpersonal therapy focuses on improving the relationships that contribute to a client's depression. With interpersonal therapy, you'll identify negative patterns in your client's social interactions, including interactions with friends, family members or their spouse. After you recognize unhealthy behavior, you can help the client learn new, more positive ways to interact with others.
Creating Depression Treatment Plans with ICANotes
Creating a treatment plan for clients with depression may seem like a daunting task with all the different areas to cover. Even though treatment plans should be thorough and specific, they don't have to add too much time to your current workload. With electronic health record (EHR) software like ICANotes, you can seamlessly add depression treatment plans to your workflow.
At ICANotes, we designed our EHR software to meet behavioral professionals' documentation needs. ICANotes includes comprehensive lists of common mental health issues and goals that automatically populate based on your selections. With ICANotes, you can create a treatment plan in a few simple steps using a customizable template and point-and-click data. The easy-to-use EHR system will store and organize each treatment plan securely, along with other essential mental health notes, such as progress notes and discharge summaries. Overall, with ICANotes' EHR, you'll type less, save time and enjoy greater peace of mind knowing your notes are extensive, accurate and compliant with privacy laws.
Try ICANotes Today
Treatment plans are at the foundation of effective therapy for depression. They also help provide the proof you need to get reimbursed by insurance companies for your services. If you're concerned that depression treatment plans will add to your documentation burden, ICANotes can help. EHR software from ICANotes can let you complete treatment plans faster and easier and ultimately guide your clients toward their goals.
Are you ready to try creating a depression treatment plan with ICANotes? Request your free trial today or contact our support team to learn more.
Schedule a Live Demo
Sources
- https://www.who.int/news-room/fact-sheets/detail/mental-disorders
- https://news.gallup.com/poll/505745/depression-rates-reach-new-highs.aspx
- https://www.samhsa.gov/data/sites/default/files/reports/rpt29393/2019NSDUHFFRPDFWHTML/2019NSDUHFFR1PDFW090120.pdf
- https://www.mayoclinic.org/diseases-conditions/depression/symptoms-causes/syc-20356007
- https://navigatingtheinsurancemaze.com/articles/treatmentreviews2/
- https://documentationwizard.com/7-reasons-document-medical-necessity-even-dont-take-insurance/
- https://www.guilford.com/excerpts/leahy.pdf?t
- https://www.depressioncenter.org/toolkit/i-want-stay-mentally-healthy/goal-setting
- https://www.indeed.com/career-advice/career-development/difference-between-goals-and-objectives
- https://www.med.upenn.edu/bbl/assets/user-content/documents/TreatmentPlanning_Schmidt.pdf
- https://www.apa.org/depression-guideline/assessment
- https://ctacny.org/sites/default/files/trainings-pdf/Treatment%20Plans-webinar%203.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4070877/
- https://www.helpguide.org/articles/depression/depression-treatment.htm
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7001356/
- https://adaa.org/understanding-anxiety/depression-treatment-management
- https://www.medicalnewstoday.com/articles/types-of-therapy#psychodynamic
- https://www.sccgov.org/sites/bhd-p/Policies-Procedures/adult-system-of-care--policy-procedure/Documents/Clinician_Gde_toolkit.pdf
- https://support.therapynotes.com/article/117-how-to-complete-a-psychotherapy-treatment-plan
- https://www.takingcharge.csh.umn.edu/what-types-psychotherapy-are-helpful-anxiety-and-depression
- https://www.psychologytoday.com/us/therapy-types/mindfulness-based-cognitive-therapy
- https://pubmed.ncbi.nlm.nih.gov/22340145/
- https://www.verywellmind.com/mindfulness-based-cognitive-therapy-1067396
- https://www.verywellmind.com/types-of-psychotherapy-for-depression-1067407