Best Practices for Psychiatric Rehabilitation Program (PRP) Documentation

Adults struggling with mental health issues may be admitted to a psychosocial rehabilitation program (PRP). This type of program is intended to provide a variety of treatments, services and support for these patients. A PRP aims to improve patient recovery and the associated outcomes by integrating them with their community and social resources to elevate their quality of life.
Each patient has unique symptoms and qualities, and PRPs help them establish a sense of independence and community by focusing on their needs. This individualized patient focus allows the program to provide the necessary therapy and medication. As a PRP therapist, you must document patients' experiences to help ensure proper care.
Table of Contents
The Purpose of PRP Documentation
The purpose of PRP documentation is to track the psychiatric rehabilitation process. Note-writing is essential for documenting a patient's symptoms, behaviors, diagnosis and progress. Without this documentation, tracking a patient's recovery is challenging. Track the major steps of PRP with documentation to identify and measure a patient's progress and how close they are to their desired outcome.
Though it can vary for each patient, some psychosocial rehabilitation examples include:
- Treatment
- Rehabilitation
- Crisis intervention
- Enrichment
- Case management
- Basic support
- Wellness
- Prevention
Tracking your patient's progress through documentation is crucial because it provides a way to know they're moving forward and progressing toward their goal and recovery.
As a therapist, note-writing also helps you identify the focus for every treatment option and session and determine whether changes should be made. By tracking a patient's progress, you can determine what level of specificity is needed in documentation based on the patient's needs.
Information to Document for PRP
Your practice can decide how you want to format your psychosocial documentation for your psychiatric rehabilitation program. However, you should be sure to include all of the necessary information, such as the initial treatment plan, goals and objectives, changes in patient behavior, patient progress and changes in the treatment plan. Some psychosocial rehabilitation program notes examples include the following:
1. Record the Initial Treatment Plan
An initial treatment plan is a customized plan for an individual patient and is used to engage the patient throughout their treatment. This plan is essential for guiding the patient toward their rehabilitation goals and helping the therapist monitor progress and determine when to make adjustments to treatment.
Typically, a treatment plan follows a simple format and includes the following information:
- The patient's demographics
- The patient's personal information
- The patient's psychological history
- The measurable objectives
- The timeline for treatment progress
- The patient's high-priority treatment goals
- The diagnosis for the patient's current mental health issue
- Space to track the patient's progress
Treatment planning is a joint effort between the therapist and the patient. The patient's initial treatment plan should be developed by their 20th day of PRP attendance and should not exceed two months from the patient's date of admission into the program. Following the date of the initial timeframe, the plan should be reviewed every three months.
2. Record Goals and Objectives
Setting goals and identifying objectives is crucial to a successful psychiatric rehabilitation program. With goals to aim toward, patients may be able to:
- Set priorities
- Feel satisfied
- Achieve more
- Improve focus
- Stay motivated
- Boost confidence
Goals are general statements of what the patient wants to accomplish, while objectives are specific skills that the patient needs to learn to reach the goal. Some psychosocial rehabilitation goals and objectives examples include the following:
- Learn methods to express frustration in a healthy way.
- Build positive communication skills.
- Learn how to cope with negative feelings without the use of a substance.
- Learn to manage anxiety in triggering situations.
On the other hand, objectives are measurable and provide a patient with clear directions on behavior. Goals and objectives work hand-in-hand, as they are specific ways a patient can reach their goals. The following are some examples of objectives:
- For a patient struggling with positive communication, an objective may be to keep an assertiveness log to learn healthy communication skills.
- For a patient dealing with depression, an objective may be to take antidepressant medication to relieve symptoms.
- For a patient dealing with substance abuse, an objective may be to attend meetings for recovery.
- For a patient dealing with anxiety, an objective could be implementing mindfulness-based cognitive behavioral techniques to calm themselves in triggering situations.
Update the patient's treatment plan during every plan review so it contains an updated list of current rehabilitation objectives and goals. Objectives and goals should be written in behavioral terms. Avoid non-behavioral terms like “improving self-esteem” when developing rehabilitation objectives and goals.
Vague terms like “improving social skills” can make determining whether a patient has reached rehabilitation objectives and goals challenging. Instead, it's best to specifically define what the patient can do or improve to attain their rehabilitation goals.
Write objectives in a clear way that the patient can easily understand. For example, an objective to “improve the social support network” will likely be unclear to the patient. State the objectives in common language and avoid jargon to ensure patients understand their exact goals. Instead, you could state the objective as, “The patient will develop a list of people they can contact if they are unable to solve a problem at home.”
Use consecutive numbering as new goals are developed to further help with clarity. Label objectives with the respective goal numbers and unique letters.
3. Report Time in, Time out and Services Received
Each day the patient attends the psychosocial rehabilitation program, the designated staff person should fill out the patient's exact time of arrival. At the end of the program, the patient will circle the services received during that day. Record the exact time of departure and have the patient sign the statement to attest to receiving those services on that day.
List the services under the corresponding column for the performance area the service addressed, such as:
- Educational
- Vocational
- Self-maintenance living
- Social
- Illness management and wellness
Include reimbursable services at the top of the record and nonbillable services near the bottom. Ensure your practice maintains separate written descriptions of services that give a complete overview. This description includes the purpose, who may be interested in the service, contact persons, expected outcomes and goals, and the place, time and frequency of meetings.
4. Record Changes in Patient Behavior
After you and your patient identify the rehabilitation goals and objectives, work together to choose the methods and services that will be used to accomplish these objectives. As your patient moves through the steps of the PRP, it's essential to record the changes in patient behavior.
5. Record Patient Progress
Talk with the patient about their current status in every area of focus, any changes you have noted and their interest in making changes in different areas. To accurately track progress, you should first work with your patient to choose suitable target dates for objectives to be accomplished and target dates for goals. These target dates should be reasonable estimates and based on the specific objective.
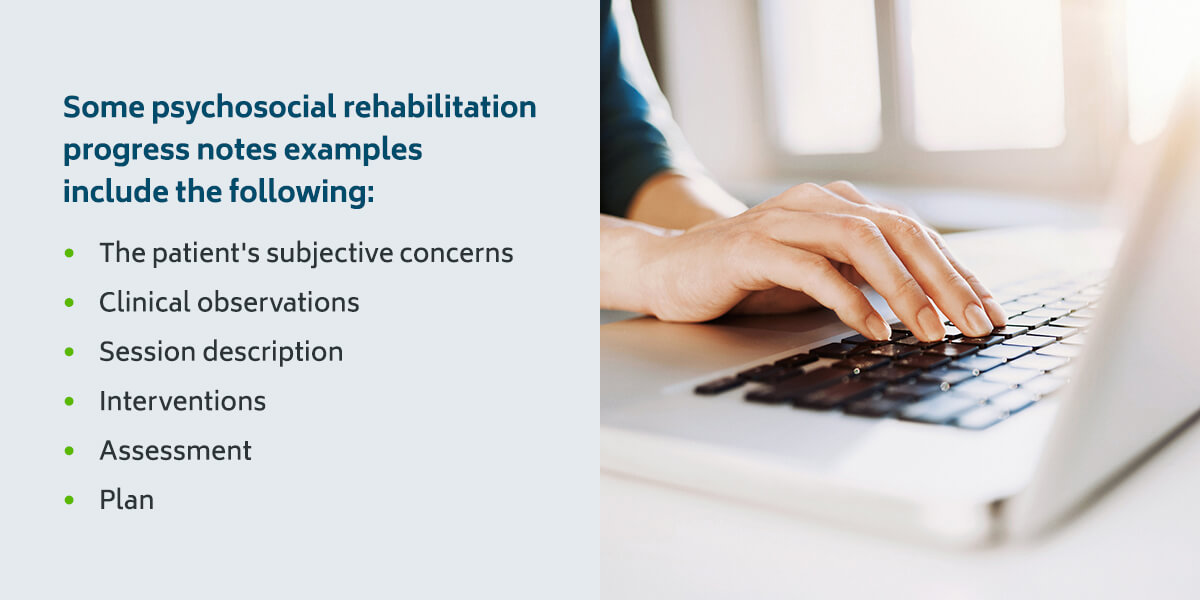
Some psychosocial rehabilitation progress notes examples include the following:
- The patient's subjective concerns: Anything the patient has noticed about their mood, energy level, motivation and interpersonal relationships.
- Clinical observations: The patient's physical appearance, body language, emotional affect and movements.
- Session description: What you spoke about with the patient in the session, for example, increased difficulty managing their symptoms, reactions to prescribed medication and any changes in their routine.
- Interventions: Any changes or additions to the treatment plan, often including evidence-based practices used by the clinician to support the patient's goal progression.
- Assessment: The clinician's observations at the end of the session, including risks and improvements.
- Plan: Action items at the end of the session, such as the patient agreeing to focus on nutrition or sleep.
Reviewing a patient's progress can also be a good time to identify any barriers that may be preventing them from making further progress or reaching their goals. As the patient makes progress, they'll likely need new areas to focus on, so this is a good time to update the master list of the patient's goals and objectives.
6. Record Any Changes in the Treatment Plan
You should also document any changes in the treatment plan, including the rehabilitation goals and objectives. As the patient progresses and displays behavior changes, their treatment plan should be adjusted accordingly. When you discuss these changes with your patient, consider any unmet needs, as well.
Status changes to record include when a rehabilitation objective or goal is revised, canceled or accomplished. If barriers are identified, you also want to adjust the treatment plan accordingly.
7. Relate the Services and Progress Notes to the Rehabilitation Goals
Finally, the services and progress notes should be connected to the rehabilitation goals, and you should make note of that connection in your PRP documentation. Be sure to also discuss with your patient the other services and supports that may be required to help them reach their rehabilitation objectives and goals. When the patient identifies other services and supports, these should be included in their plan.
Patients should sign and date the services plan, and they can opt to write comments about the plan if they choose. If you are responsible for overseeing the plan's development, you should sign and date the plan, as well. Each rehabilitation goal should have its own number. Objectives, on the other hand, are identified by the objective's own letter and the rehabilitation goal number.
Tips for Effective PRP Note Writing
Every behavioral healthcare clinician has preferred note-writing methods and routines. Some like to record impressions immediately, while others need time to decompress before writing their observations. However, the following best practices can help you refine your note-writing:
Be Specific
Relying on subjective or vague statements can hamper patient recovery and create ambiguity when you refer to your notes in your next session. Try to include specific and objective details in addition to any subjective points you add to your notes. For example, you may be tempted to rely on general statements like, “client is depressed,” or opinions like “client is a model employee."
Instead, consider qualifying these statements, like “client is experiencing sleep disturbances and low motivation” and “client displays positive feelings toward their job and believes others perceive them as a good worker.” It's also helpful to use the phrase “as evidenced by” when providing these examples, such as “client is experiencing low motivation as evidenced by difficulties completing daily tasks.”
Including facts and details makes your notes more valuable with the licensing board, judicial system and program administrators. It also helps other team members understand the client so they can provide additional support.
Consider the Details
Try and be concise in your notes wherever possible. Keep descriptions simple and to the point, provided you include all the relevant information. When a situation calls for detailed notes, like negotiating ethical dilemmas or managing high-risk patients, include as much detail as you can. How much detail to include is a judgment call, but try and include details that align with the situation.
Include the Positive
As a clinician, it's natural to focus on documenting areas that require attention. However, this practice creates a one-sided view of patient progress. Include clients' achievements and strengths in your note writing to provide a well-rounded view of their experiences so you can recognize and build on their positive outcomes and experiences.
Avoid Shorthand
Always imagine a colleague taking over your patient when you take notes. Would they be able to understand the content when they reviewed your documentation? Use plain, unambiguous language so there can be no misunderstandings about patient care.
FAQs About PRPs
Below we address frequently asked questions regarding psychosocial rehabilitation programs and documentation.
What Are the Types of PRP Models?
PRPs have different models to account for a patient's diagnosis, willingness to participate and severity of symptoms. The types of PRP models include:
- Disability: At the disability stage, mental illness can lead to a lack of ability or restrictions in ability to perform an activity or role that is considered normal. This can be displayed in the form of homelessness or unemployment.
- Dysfunction: A patient with a mental illness at the dysfunction level lacks the ability to perform typical activities or tasks that are considered normal. Dysfunction may include a lack of social adjustment skills.
- Impairment: Impairment is defined as mental illness that leads to abnormality or loss of physiological or psychological function or anatomical structure. Impairment can display in a variety of forms like depression, delusions or hallucinations.
- Disadvantage: At the disadvantage stage, severe mental illness interferes with the patient's ability to perform an activity or fulfill a normal role associated with their sex, age and social and cultural factors. Disadvantages may include poverty and discrimination.
What Are the Phases of PRP?
As a therapist, you can better keep track of a patient's progress by segmenting the PRP process into phases. Use documentation at each step to track patient progress, and make adjustments to goals and objectives as needed. The main phases of PRP include:
- Diagnosing: The diagnosing phase determines how ready the patient is for rehabilitation. The therapist helps the patient set goals and evaluate their skills and strengths related to their goals. Resource and functional assessments should also be conducted during this phase, as they are essential tools for the rehabilitation process.
- Planning: The planning phase involves planning for skills and resource development to reduce symptoms. Additionally, the therapist will develop high-priority objectives and supports for the patient's rehabilitation goals.
- Intervention: The intervention phase involves implementing the rehabilitation plan to help achieve the patient's goals by changing the patient or their environment with the progress of their supports and skills. In this phase, direct skills are taught and utilized, along with resource coordination and modification.
How ICANotes Can Help With PRP Documentation
ICANotes can aid in PRP documentation. Our technology makes completing case management notes and documenting your PRP easier. The advantages your practice can enjoy with ICANotes software for PRP documentation include:
- Converting paper forms to digital files: With ICANotes, your practice can convert paper documents to electronic files. You'll upload the scanned images of the paper forms and attach these to patient charts. Our software can support a variety of file types, such as DOC, PDF, GIF, PNG and JPG.
- Eliminating paper: Our electronic health record (EHR) can help your practice eliminate paper. At ICANotes, we offer a patient portal that aids your transition from paper to digital documents.
- Incorporating a patient portal: A patient portal adds convenience for your patients, allowing them to log in anywhere to view their patient charts. They can also use this portal to enter their demographics and history. You can opt to create electronic intake forms that patients fill out and sign via the patient portal. These forms will be displayed in PDF form on the patient chart.
- Exchanging clinical documents: Our clinical document exchange allows your practice to send patient documents to other health providers electronically via direct messaging or electronic fax.
- Providing access to multiple users: Our software is secure and accessible to authorized remote users.
You can both reduce documentation time and improve compliance with ICANotes. With our EHR, your practice can develop treatment plans, initial assessments, clinical summaries, case management notes, group therapy notes and discharge summaries.
Streamline Your PRP Documentation With ICANotes
As a therapist doing PRP therapy, you need a method for documentation. At ICANotes, we can streamline your psychiatric rehabilitation program documentation. You'll spend less time creating documents and feel reassured that your documentation will comply with regulations. You can also say goodbye to revenue loss due to under-coded notes or rejected claims. Features of our EHR include:
- Scheduling: Efficiently manage appointments with our user-friendly patient scheduling solution.
- Secure messaging system: You can securely communicate in and out of the office with our HIPAA-compliant messaging system.
- Document management: Managing your documents is simple when you can easily scan and upload documents.
- Integrated billing system: Use our integrated billing system to easily create statements, CMS forms and superbills. Your practice can accept cash, checks and credit cards.
ICANotes is intended specifically for behavioral health practices and is ready out of the box. Our software can make your documentation speedy, sophisticated and fast enough to meet even the most rigid standards. ICANotes is compatible with any clinical discipline in an inpatient or outpatient setting and delivers the most intuitive and clinically robust charting solution. Sign up for a free trial of ICANotes today.