Putting Together a Good Faith Estimate
Healthcare rules and regulations are constantly changing. In late 2021, Congress passed the No Surprises Act. One of the Act's goals is to eliminate unexpected health care bills and minimize payment disputes between patients and providers.
When the No Surprises Act took effect in 2022, it also introduced the concept of the Good Faith Estimate. Providers need to give patients who are self-pay or uninsured an estimate of the cost of their treatment before the treatment begins. Although a Good Faith Estimate doesn't have to be exact, it must contain certain information. It's also critical that the actual cost of treatment not be substantially more than the estimated amount.
Learn more about the requirements for a Good Faith Estimate and how to put one together.
Table of Contents
- How the Good Faith Estimate Relates to the No Surprises Act
- What Is the Good Faith Estimate and Who Is It For?
- Who Is Required to Create a Good Faith Estimate?
- When Should Clients Be Given a Good Faith Estimate?
- What Information Should Be Included in a Good Faith Estimate?
- Steps to a Good Faith Estimate
- Good Faith Estimate Concerns
- How to Systematize Good Faith Estimates
- FAQs
How the Good Faith Estimate Relates to the No Surprises Act
No one wants to receive a surprise bill or have to pay much more than they were anticipating for a service or treatment. The No Surprises Act seeks to end the practice of balance billing, which often leads to high health care bills.
Balance billing typically occurs when a patient seeks treatment from a provider or facility outside their insurance network. Insurance companies usually don't cover the total cost of out-of-network care. Previously, that meant a facility or provider could bill the patient for the remaining balance. In some cases, the balance could be thousands of dollars and difficult for patients to pay.
In addition to banning balance billing, the Act also requires facilities to give patients a notice that explains billing protections.
Another component of the No Surprises Act is the Good Faith Estimate. While eliminating balance billing protects people with health insurance, the Good Faith Estimate requirement protects the uninsured or people who might decide to self-pay for a particular service or treatment.
Under the Act, any uninsured or self-pay patient needs to receive an estimate for the cost of care before treatment or service begins.
What Is the Good Faith Estimate and Who Is It For?
A Good Faith Estimate lets patients know the anticipated cost of any services or treatments they might receive from a clinician. The estimate is intended for a patient who either doesn't have insurance or who decides not to use insurance to cover the cost of behavioral health services.
While the estimate needs to be made in good faith, it doesn't have to be perfect or reflect the exact costs of care. There can be some discrepancy between the estimated amount and the actual cost of treatment.
Uninsured or self-pay patients have a right to a Good Faith Estimate even if there's a chance that their costs will be zero. For example, a facility that covers the cost of patient care through grants still needs to give patients an estimate, as there's a chance that charges won't be $0.
While the Good Faith Estimate doesn't have to perfectly align with a patient's actual costs, it should be in the ballpark. If the patient's bill ends up being $400 or more than the quoted amount, they have the right to dispute the bill.
Who Is Required to Create a Good Faith Estimate?
Any healthcare provider with a license or certification needs to create and provide a Good Faith Estimate to self-pay or uninsured patients. A provider might also need to give an estimate to an insured patient who requests one.
Good Faith Estimates are required from behavioral health providers and medical providers.
When Should Clients Be Given a Good Faith Estimate?
Clinicians should provide clients with a Good Faith Estimate before care or treatment begins. In some cases, that can be the day before a scheduled treatment. A patient might also ask a provider to give them a Good Faith Estimate before scheduling treatment or care.
If a patient schedules care or treatment at least 10 days away, a provider must deliver the estimate within three days. A provider also needs to give an estimate to a patient within three days of a request, even if no treatment is scheduled.
What Information Should Be Included in a Good Faith Estimate?
A good faith estimate is an estimate, not a guess. That means it should be based on the services or treatments a provider reasonably expects to offer. The cost of those treatments should be based on a providers' cash pay rate or what a provider would charge an insurer if they were to bill insurance.
Along with an estimate of the cost of care, the Good Faith Estimate should contain information such as:
- Patient's name
- Patient's date of birth
- Description of the primary service or treatment and the scheduled date, if available
- Itemized list of services or treatments that might be performed
- Relevant diagnosis codes
- Relevant billing codes
- Estimated cost of each service
- Name and ID number of each provider who will treat the patient
- A list of supplemental services or treatments a patient might need before, during or after care
- Disclaimers that inform patients of their rights, note that actual costs might differ and that additional treatments might be recommended and scheduled separately
The US Centers for Medicare and Medicaid Services (CMS) has a template clinicians can use when creating Good Faith Estimates. ICANotes also has a Good Faith Estimate template built in to streamline the process.
Steps to a Good Faith Estimate
Under the No Surprises Act, providers are responsible for discussing potential costs with their patients upfront. There are several steps to take to verify that you need to provide an estimate and to create it.
The first step is to ask a patient about their insurance status. You don't need to give an estimate to patients who have private insurance coverage or who are using coverage such as Medicare or Medicaid.
If a patient is self-pay or uninsured, your practice needs to tell them that a good faith estimate is available. The estimate needs to be given to a patient in a written format, either paper or digital. If the estimate is digital, it should be in a format that a patient can download, save and print. The estimate should be in the patient's language and should be easy to understand.
It's also possible to give a patient a verbal estimate of costs. Any verbal estimate should be followed up with a written one. A behavioral health clinician might not know what treatments or services a patient will need or how long treatment will last before meeting with a patient. It can be a good idea to provide an estimate to a patient for the intake session. Then, if additional sessions or treatments are needed, you can provide the patient with a second estimate.
You might also have to update the patient's good faith estimate if anything changes, such as the recommended treatment or the provider. The updated estimate should be given to the patient at least one day before care begins.
Good Faith Estimate Concerns
While Good Faith Estimates can help patients get a better sense of how much their behavioral health care will cost and help them plan for the costs of care, some potential complications can arise.
One issue that might concern providers is estimating a patient's care trajectory early in the relationship. Often, it can take several sessions before a clinician understands a patient's story and needs. One way to work around that is to provide a Good Faith Estimate for each session. Doing so gives clinicians a chance to get to know their patients. After several sessions, you're likely to have a better sense of the treatment needed and can provide a more in-depth and longer-term estimate then.
Some patients might be concerned about having the estimate in writing, creating a paper trail. Providers can ensure patients that HIPAA protects their privacy and that the provider's practice complies with health care privacy laws.
Another concern is that some patients might experience sticker shock when they see the cost of treatment presented as a lump sum. If that occurs, remind patients that it's possible to pay as they go or that you can work out a payment plan to make the cost of care more affordable.
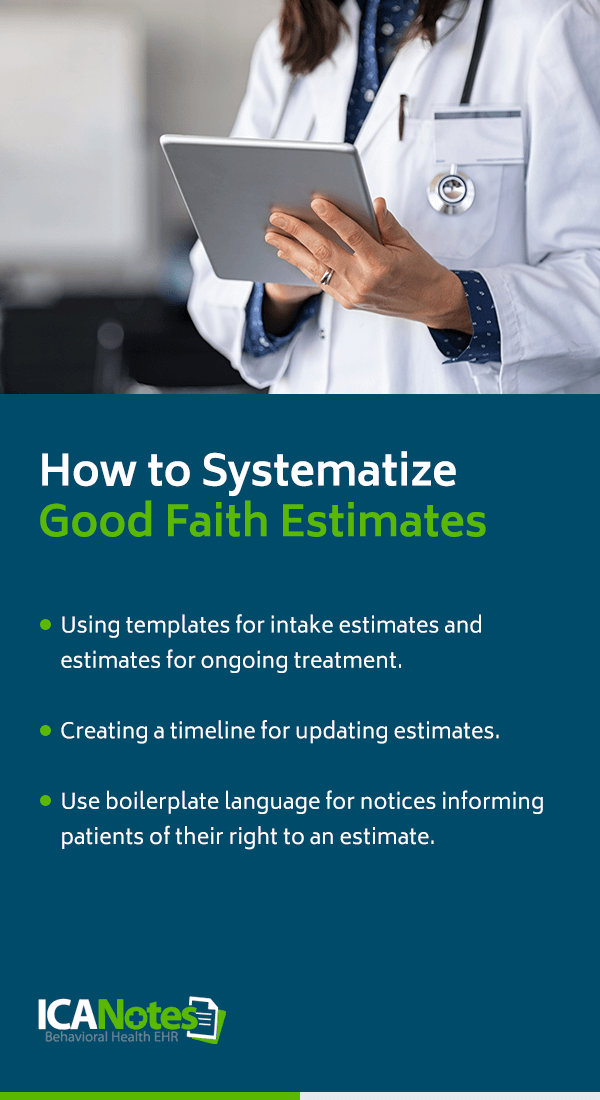
How to Systematize Good Faith Estimates
Systematizing how your practice manages Good Faith Estimates will streamline the process and save your providers time. A few things you can do to make it easier for providers to create and update estimates include:
- Using templates for intake estimates and estimates for ongoing treatment.
- Creating a timeline for updating estimates.
- Use boilerplate language for notices informing patients of their right to an estimate.
FAQs
Since the Good Faith Estimate is a relatively new requirement, many providers have questions about how it works or what's required of them. Take a look at some answers to commonly asked questions.
Can clients waive their right to a Good Faith Estimate?
The Act doesn't specifically give patients the option to waive their right to an estimate, the way it allows them to waive some balance billing protections. Even if a client isn't interested in getting an estimate, a provider must give it to them.
Is the good faith estimate binding?
The prices quoted in the estimate aren't binding, as a Good Faith Estimate is only an estimate. A patient might end up needing fewer treatments or less service than anticipated or they might need more. However, if the cost of care ends up being more than $400 above the quote, a patient can dispute the estimate.
What happens if my estimate is wrong?
Patients have a right to dispute bills that substantially exceed the amount of the estimate. Substantially exceeds means the cost was more than $400 higher than the estimated price. Patients can file a dispute online to start the resolution process.
When estimating costs, can I use a range?
You can use a range when providing patients with an estimate, particularly if you're not sure how many sessions a patient might need.
How can I estimate costs or services for clients I haven't met?
The Good Faith Estimate isn't set in stone. You can revisit the estimate after meeting a patient for the first time and make updates to it as necessary. Another option is to give a patient an estimate for the first session and then a second estimate for subsequent treatment.
Can the Good Faith Estimate be part of a patient's intake paperwork?
The Good Faith Estimate shouldn't be integrated into your standard intake paper. It's essential that patients be made aware of it. For that reason, the estimate should be a separate document you give or send to patients. Additionally, you need to provide patients with the estimate based on the rules of the Act, such as within three days of scheduling treatment.
How should I document delivery of the Good Faith Estimate?
A patient's estimate becomes part of their medical record, so it should be kept with their other files. When putting the estimate into a patient's electronic health record (EHR), be sure to include the date it was delivered and the delivery method, such as email or postal mail.
Do these requirements apply to existing patients?
Yes, you need to provide existing uninsured or self-paying patients with a Good Faith Estimate of the cost of services.
How is an incorrect good faith estimate resolved?
If a patient disputes a bill that substantially exceeds the estimated amount, a third party, known as a dispute resolution entity, will review the case. The entity will review the estimate, bill and information provided by the practice to determine whether the patient should pay the amount on the estimate, the billed amount or something in between.
What happens if I don't create a Good Faith Estimate?
If your practice doesn't provide self-pay or uninsured patients with a Good Faith Estimate, you can be fined for non-compliance.
Good Faith Estimate Templates and More with ICANotes
The Good Faith Estimate requirement adds another item to clinicians' already full to-do lists. Fortunately, you can streamline the process and ensure compliance with the new regulations with ICANotes.
Our EHR provides quick and simple workflows for Good Faith Estimates for clinicians. You can access a Good Faith Estimate template through the “Forms and Assessments” section of every patient's chart. The form will auto-populate with the patient's information, your practice name and the date. Once you enter the diagnosis and the number of sessions, the form can fill in the estimated cost for you. You can also manually enter estimated cost information.
Our template also includes the necessary disclaimers for Good Faith Estimates. Once you've prepared the estimate, you can compile the note and print or send it to the patient.
ICANotes Is Here for Your Good Faith Estimates
The Good Faith Estimate requirement makes the cost of treatment more transparent for patients but can add additional burdens on providers. With ICANotes, you can comply with the No Surprises Act while continuing to offer your patients high-quality care. Schedule a free trial today to see how our EHR and practice management software simplifies the estimate process.
Sources
- https://www.cms.gov/newsroom/fact-sheets/no-surprises-understand-your-rights-against-surprise-medical-bills
- https://www.portagehealth.org/for-patients-visitors/understanding-your-healthcare-costs/good-faith-estimate
- https://welllifetherapyllc.com/good-faith-estimate
- https://www.apaservices.org/practice/legal/managed/good-faith-estimate-compliance
- https://www.healthindustrywashingtonwatch.com/2022/02/articles/department-of-health-and-human-services/no-surprises-act-good-faith-estimates-what-they-are-and-when-you-need-them/
- https://therapyreimagined.com/modern-therapist-podcast/the-january-2022-surprise-of-good-faith-estimates-requirements/
- https://www.apaservices.org/practice/legal/managed/billing-disclosure-requirements
- https://www.cms.gov/CCIIO/Resources/Regulations-and-Guidance/Downloads/Good-Faith-Estimate-Patient-Provider-Dispute-Resolution-Process-for-Uninsured-or-Self-Pay-Individuals.pdf
- https://www.experian.com/blogs/healthcare/2021/12/no-surprises-act-good-faith-estimate-faq-with-an-expert/
- https://nosurpriseact.gr8.com/