What Providers Need to Know About Out-of-Network Insurance Reimbursement
Out-of-network providers are clinicians who do not have a contract with a specific insurance plan, meaning they aren’t part of that plan’s preferred network. This status can significantly affect how, and how much, they’re reimbursed for services. For behavioral health professionals, navigating out-of-network reimbursement comes with unique challenges and opportunities. Understanding the implications can help providers protect their revenue, support their clients, and make informed decisions about practice management.

Fatima Davis, RCM Manager
Last Updated: July 17, 2025

This blog post offers a practical overview of what behavioral health clinicians need to know about working as out-of-network providers. It explains how out-of-network status affects reimbursement, highlights key differences from in-network participation, and outlines best practices for discussing costs with clients. You will also learn how to use tools like superbills and courtesy billing to support patient reimbursement, and how to stay compliant with laws like the No Surprises Act. Whether you're new to private practice or considering leaving insurance panels, this guide helps you navigate out-of-network billing with clarity and confidence.
Do You Have to Sign Up to Be Out of Network?
Typically, a provider does not have to sign up to be out of network. You are automatically an out of network provider if you do not sign a contract with an insurance plan, so no additional steps are needed on your part to be out of network. However, some insurance plans require you to register as an out of network provider.
Why Insurance Payers Want You to Join Their Network
Insurance payers want you to join their network for two reasons — they can ensure you meet their quality standards and pay you a prearranged rate for services. Insurance companies want to be able to control and predict costs, and they do so by maintaining a network of providers.
Being an in-network provider can mean that you accept a reduced payment, and you may face restrictions or requirements to be an in-network provider. On the other hand, an insurance company may discourage members from going to out of network providers and incentivize visits to in-network providers. Ultimately, you should consider the pros and cons of being an in-network clinician or an out of network clinician before determining which is the right option for you.
The Benefits of Being In Network
If you choose to be an in-network provider, you may enjoy the following benefits:
- Automated marketing: Being an in-network provider provides automated marketing because members will search their insurance plan's database for preferred providers. Being part of an insurance plan's database can improve your visibility to potential clients. The more networks you belong to, the more organic client leads you can potentially receive.
- More affordable for clients: Clients using in-network benefits can typically enjoy reduced costs. Greater affordability can mean your clients are more likely to return for repeat sessions.
- Larger client pool: Since being an in-network provider can make your services more affordable for clients, you may have access to a larger pool of potential clients. Other providers may also refer clients to your practice if you belong to the same insurance network.
Want to master your mental health billing process?
Download our complete guide to billing for mental health services
Simplify behavioral health billing, avoid common coding mistakes, reduce claim denials, and get paid faster with this step-by-step guide—perfect for solo clinicians or billing staff.
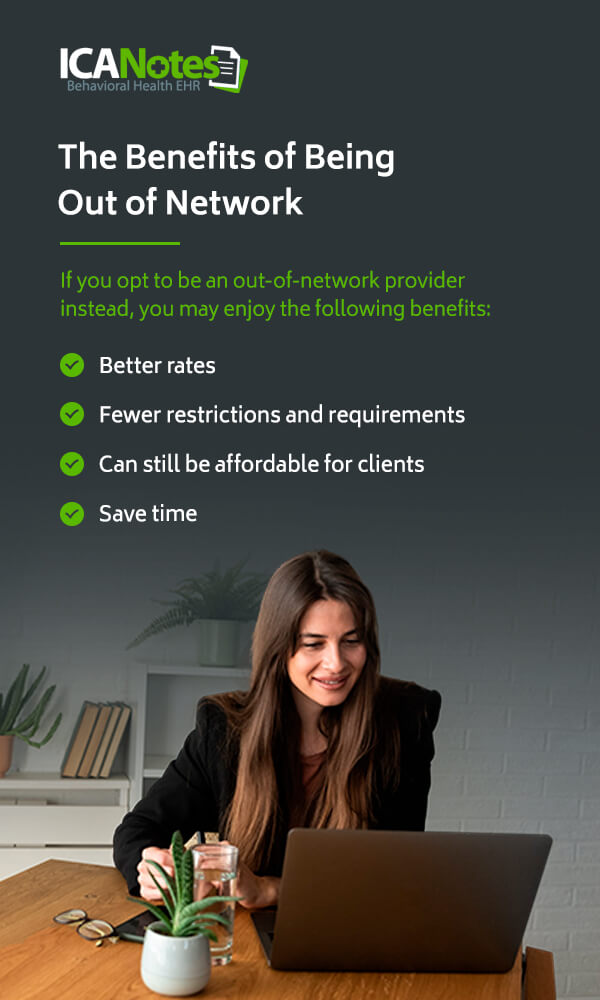
The Benefits of Being an Out of Network Provider
If you opt to be an out of network provider instead, you may enjoy the following benefits:
- Better rates: When you choose to remain an out of network provider, you may be able to set higher rates than you would as an in-network provider.
- Fewer restrictions and requirements: There is greater freedom when you choose to be an out of network provider, as there are often restrictions and requirements for in-network providers to remain in an insurance provider's network.
- Can still be affordable for clients: Going to an out of network provider can still be affordable for clients, especially if they have some coverage for out of network reimbursement. Depending on their insurance plan, an in-network provider can still be expensive to visit between copays, coinsurance and deductibles.
- Save time: Applying to be an in-network provider can take time — and can be a waste of time if the insurance company rejects your application. Additionally, making an in-network claim can be a lengthy process due to all the insurer requirements, meaning remaining out of network may save you time.
Be Transparent About Being Out of Network
You should be transparent with your patients about being out of network. Your patients need to understand the implications and what the costs for their behavioral health treatment could be as a result. Be clear with your patients about your fees and how the payment process works. For example, let your clients know if payment is due in full at the time of the service or if you will bill their insurance plan first and then charge them the remainder.
Let your clients know if you are open to helping them apply for out of network reimbursement from their insurance plan. Helping your clients with their insurance can help them afford your services and help you retain patients. In some states, an ethical code may require you to help clients with third-party providers, so be sure to give your clients all the information they need about this process.
How Being Out of Network Affects Your Practice
You can lose new clients when they discover you are an out of network provider, which can negatively impact your business. To help combat the loss of new clients, you can offer to contact the potential client's insurance plan about their out of network reimbursement coverage. In this case, the potential client should give you the information off their insurance card, and you can call their insurance plan and let the client know about their out-of-network coverage.
For example, even if you are not an in-network provider, the client may still be eligible for some out of network reimbursement that covers a percentage of their costs and makes treatment affordable. If the potential client has a deductible, you can let them know how that would factor into their costs. Taking this step can get you a new client, ensure affordable care for them and demonstrate that you care about their health, which can lead to a long-lasting clinician-patient relationship.
Today, it can be difficult for clients to find in-network therapists, so the next best option is often an out of network provider with whom a client can still get receive some out of network reimbursement. If you build a connection with a potential client over the phone, and they cannot find a therapist in their network, they may return to you because of the care you demonstrated. If you are actively trying to fill slots in your practice, taking this step can be well worth your time.
What is Courtesy Billing?
Courtesy billing is a less risky billing method in which your client pays you upfront, but you submit the bill to your client's insurance plan on their behalf as a courtesy to your client. The insurance company will then reimburse the client as they would have if the client had submitted the bill themselves.
In the behavioral health field, this can eliminate an administrative burden for clients already struggling with anxiety, depression or other mental health issues. Additionally, you can ensure you still get paid in full and don't take on any financial risk. Though this means additional time spent on administrative tasks for you or your staff, courtesy billing can attract new clients or retain existing clients who may be struggling with the billing process.
Out of Network and W-9s
If you are an out of network provider, your client's insurance plan may request a W-9 form before they provide reimbursement. Since you are not an in-network provider with that insurance plan, they are not familiar with your information, such as your tax ID number or National Provider Identifier (NPI). A W-9 confirms that you are a clinician and verifies your information with your signature. The insurance plan can then add your information into their system.
You can print and complete the W-9 form or fill it out online. The insurance plan may request that you or your client submit the form, so be sure to note the plan's instructions. Completing a W-9 form is simple and free and will ensure your client receives out of network reimbursement.
The No Surprises Act
The 2021 No Surprises Act protects consumers from surprise medical bills. This act most likely applies to your services, so it's crucial to understand this new law as an out of network provider and ensure you comply. For example, you must inform your clients that out-of-network care could be more costly and offer options that could help clients avoid balance bills. Watch our on-demand webinar to learn more about the No Surprises Act. ICANotes simplifies the process of providing clients with a good faith estimate as required by the No Surprises Act. We have a built-in good faith estimate form. Book a demo and one of our product experts will show you how it works.
Contact ICANotes
At ICANotes, we understand the increasing complexity of the healthcare environment has made your job more challenging than ever. We want to help you spend fewer hours creating documentation, give you peace of mind that your documentation will pass regulatory scrutiny and improve the content and legibility of your clinical documentation. If you are losing revenue because insurance companies are rejecting your claims or you are under-coding your notes, ICANotes can help.
ICANotes is ready to immediately make your behavioral health documentation comprehensive, sophisticated and fast enough to meet even the most stringent standards. Contact us at ICANotes to learn more about out-of-network providers or request your free trial of ICANotes today.
Schedule a Live Demo
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals—built to streamline documentation, improve compliance, and enhance patient care.
Simplify clinical charting
Stay organized with appointment scheduling
Reduce no-shows with automated reminders
Improve client engagement with a secure patient portal
Provide flexible care with HIPAA-compliant telehealth
Related Posts
Fatima C. Davis is the RCM Manager at ICANotes and a seasoned expert in behavioral health revenue cycle management. With over 20 years of experience, she specializes in optimizing collections, reducing denials, and ensuring compliance across diverse payer landscapes. Fatima has led RCM operations for large multi-agency systems and is passionate about helping behavioral health practices achieve financial sustainability.