2018 Updates to the EHR Incentive Program
With past electronic health record (EHR) incentive programs, behavioral health professionals were excluded from the list of eligible professionals (EPs). This means they were unable to participate in EHR incentive programs and could not receive incentive payments for using EHR technology in their practice. However, as medical professionals and government officials are recognizing the value of EHR technology in regards to patient care, changes are being made to include behavioral health practices.
Now, due to recent bill approvals by both the US Senate and Congress, it is likely behavioral health EHR incentive programs are in the making, and mental health professionals can prepare to jump on board with certified EHR technology. To give clinicians an idea of what to expect in the coming years, we will look at changes made to the EHR Incentive Program over the years, and how they affect all healthcare professionals. As you will see, healthcare providers must meet certain requirements to qualify for incentives and avoid penalties. Behavioral health professionals, particularly those who accept Medicare and Medicaid, might expect similar regulations in future incentive programs.
In this post, we will answer questions about Medicare and Medicaid EHR incentive programs and share the updates you need to know as a behavioral health professional.
In 2011, the Centers for Medicare and Medicaid Service (CMS) established the Medicare and Medicaid EHR Incentive Programs. The EHR Incentive Program was developed to encourage eligible healthcare providers to adopt and demonstrate meaningful use of EHR technology. An EHR, also called an electronic medical record (EMR), allows healthcare professionals to document patient information electronically rather than on paper. To participate in the EHR Incentive Program, you must:
- Be an eligible professional (EP)
- Demonstrate the meaningful use of certified EHR technology (CEHRT)
The EHR Incentive Program gives payments to providers who use EHR technology in ways that benefit their patients. Healthcare providers must meet certain objectives to receive payments and do not automatically qualify just by purchasing and owning EHR software. It is important for healthcare professionals to know that not all EHR software is certified to meet program requirements.
The original EHR Incentive Program for Medicaid and Medicare spanned from 2011 to 2015 and has since gone through some changes to offer more flexibility for physicians and other healthcare providers. As of February 2018, more than 544,000 healthcare providers received payment for participating in Medicare and Medicaid incentive programs.
What Is the Promoting Interoperability (PI) Program?
In 2018, the CMS decided to update the EHR Incentive Program and rename it the Promoting Interoperability (PI) Program, to demonstrate a new focus on improving patients’ access to their medical information and making program requirements less of a burden for eligible providers. The goal is to make it easier and less time-consuming for physicians to participate in incentive programs, and give patients the power to control their own healthcare data and how it is used.
PI Program regulations vary between Medicaid and Medicare PI programs. For example, starting in 2015, Medicare EPs who do not demonstrate meaningful use of EHR technology are subject to payment reductions starting at one percent and increasing up to five percent for each year the EP does not demonstrate meaningful use.
Eligible providers who accept Medicaid receive higher incentive payments over a six-year period. The last year an EP could start participation in the Medicaid PI Program was 2016, and incentive payments extend through 2021.
In 2009, the Health Information Technology for Economic and Clinical Health (HITECH) Act was passed in a movement to update the nation’s infrastructure. The HITECH Act supports the CMS incentive programs and the meaningful use of EHR.
Meaningful use means that healthcare providers cannot just own EHR technology — they must demonstrate to the CMS that they use the technology to benefit their patients to receive incentive payments. The CMS developed objectives to guide providers in demonstrating meaningful use. The “five pillars” of meaningful use are as follows:
- To improve quality, safety, efficiency and reduce health inequalities
- To engage patients and families in their health
- To improve care coordination
- To improve population health
- To ensure sufficient privacy and security of personal health information
Healthcare providers who practice meaningful use of EHR technology help patients get more involved in their health by allowing them easier access to their health information and ensuring their information is secure. Providers benefit from the meaningful use of EHR software because it boosts efficiency and helps them make important decisions about patient care.
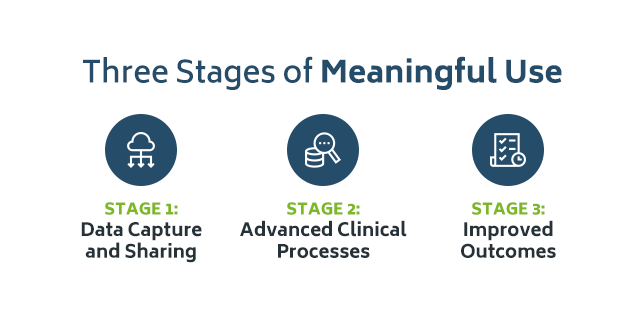
What Are the Three Stages of Meaningful Use?
From 2011 to 2015, the CMS developed three stages of meaningful use to guide EPs and ensure they were meeting program requirements. Each stage has its own set of rules to help providers demonstrate meaningful use of EHR technology. Since 2015, changes have been made to allow for greater flexibility.
Stage 1: Data Capture and Sharing
In 2011, the CMS and Office of the National Coordinator for Health Information Technology (ONC) presented the final rules of meaningful use, published in the Federal Register. Stage 1 focuses on the following objectives:
- Electronically capturing health information in a structured format
- Using that information to track clinical conditions and communicating the information to promote care coordination
- Using clinical decision support tools to aid disease and medication management
- Using EHR technology to engage families and patients
- Reporting clinical quality measures (CQMs) and public health information
In general, the goal of Stage 1 was to familiarize EPs with certified EHR technology and to build a strong foundation for future use. Specific rules and measures are listed in the Federal Register.
Stage 2: Advanced Clinical Processes
In 2013, the CMS and ONC set the final requirements that healthcare providers must meet to receive incentive payments. They also set the criteria that EHR technology must meet to obtain certification. In general, Stage 2:
- Expands on Stage 1 goals to encourage the meaningful use of EHR technology, improve patient care and promote a structured and secure exchange of health information
- Includes more demanding requirements such as e-prescribing and structured laboratory results
- Includes the objective to report cancer cases to a cancer registry using EHR technology
The overall goal of Stage 2 is to maximize the potential of EHR technology.
Stage 3: Improved Outcomes
In 2015, the final rules for the incentive program were set as well as modifications to Stage 2. To receive incentive payments and to avoid negative payment adjustments under the Medicare EHR Incentive Program, EPs must meet the final requirements of Stage 3 starting in 2019. The goals of Stage 3 focus on:
- Improving quality, safety and efficiency to promote better outcomes
- Decision support for national high-priority conditions
- Patient access to self-management tools
- Improving population health
Each stage has its own suggested measures and requirements, published in the Federal Register, to keep EPs on track and help them reach their program goals.
Eligible professionals who could participate in the Medicare EHR Incentive program included individual providers such as:
- Doctors of medicine, osteopathy, dental surgery or dental medicine, podiatry and optometry
- Chiropractors
Those ineligible for the Medicare EHR Incentive Program included:
- Practices
- Medical groups
- Hospital-based professionals
Behavioral health professionals who do not prescribe medication were not included in the EHR Incentive Programs. This may be partially due to slower adoption of EHR technology in the behavioral health field. In the past, mental health professionals have expressed concerns over patient privacy with EHR use. According to the American Health Information Management Association (AHIMA), a 2012 survey found that only 21 percent of behavioral health organizations used EHR technology.
Other factors such as questioning the usefulness of EHRs and the importance of patient-to-therapist relationships is believed to have slowed down adoption. The adoption of EHR technology benefits patients and behavioral health professionals, especially in practices that treat individuals with substance use disorders. With EHR technology, psychiatrists and psychologists can easily access a patient’s medical records and prescribe proper treatment for complex disorders. Overall, treatment planning is safer and more efficient with EHR.
Learn More About Writing Individualized Treatment Plans
To help combat the national opioid crisis, the U.S. House of Representatives recently passed new bills, including legislation to test incentive payment programs for behavioral health professionals using EHRs. The bill H.R.3331, in particular, states that the Center for Medicare and Medicaid Innovation (CMMI) can test providing incentive payments for behavioral health providers for:
- Adopting EHR technology
- Using EHRs to improve care and coordination of care
This new legislation allows providers who were not offered funds in the original EHR Incentive Programs to participate. The goal is to close the gap between behavioral health care and primary care to improve care coordination and provide better treatment and prevention services.
Behavioral health professionals who accept Medicaid might be interested in participating in a future EHR incentive program. Medicaid is the largest payer for mental health services in the U.S. and is becoming more involved in the reimbursement of substance use disorder treatment. Although all states offer the Medicaid PI Program voluntarily and are responsible for determining timelines and reporting periods, healthcare providers who participated in the program can receive payments through 2021. The last year a provider could start participation was 2016. Nevertheless, with new programs likely underway, behavioral health professionals might consider how former programs worked to help them prepare for future participation.
If a behavioral health professional has the opportunity to participate in a Medicare incentive program, they may be subject to payment reductions if they are eligible but choose not to participate, based on past Medicare EHR Incentive Program regulations. Either way, if a behavioral health provider adopts EHR technology, they can make better decisions and safely treat patients who also spend a lot of time in the hospital or primary care office. Individuals with mental health problems commonly use other healthcare services. For example, in 2007, almost 12 million emergency department visits in the United States involved patients with a substance use disorder, mental health disorder or both.
Other updates for healthcare professionals to be aware of include:
- Stage 2 has been modified to ease reporting requirements.
- Stage 3 focuses on using CEHRT to improve health outcomes.
- The CMS has proposed changes to Medicare Payment rates and policies under the Long-Term Care Hospital (LTCH) Prospective Payment System (PPS) and the Inpatient Payment System (IPPS).
- The CMS is proposing to overhaul the Medicare and Medicaid EHR Incentive Programs to improve flexibility and focus on the electronic exchange of health information between patients and providers.
- Beginning with the calendar year (CY) 2019 reporting period, all eligible hospitals will be required to use 2015 edition CEHRT.
The CMS is currently in the process of finalizing updates, and providers are encouraged to frequently visit their landing page to stay on top of the recent news.
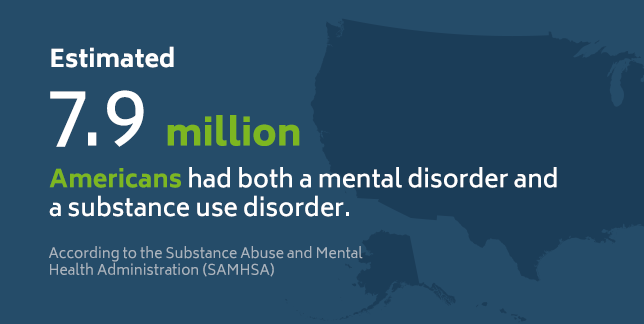
How Are EHRs Beneficial to Patients and Providers?
EHR technology is beneficial to both patients and providers in many ways, especially with the number of patients who cope with multiple disorders. For example, according to the Substance Abuse and Mental Health Administration (SAMHSA), an estimated 7.9 million Americans had both a mental disorder and a substance use disorder. Also, according to the National Institute on Drug Abuse, individuals who struggle with substance abuse, often have one or more associated health issues.
These issues might include heart disease, lung disease, cancer or other conditions. EHR technology helps mental health professionals and physicians communicate with ease and coordinate the most effective treatment plans for their patients. However, that is just one benefit. Here’s a list of the many benefits patients and providers enjoy with EHR technology:
- Reduced paperwork
- Improved healthcare quality
- Fewer reporting errors
- More efficient administrative tasks
- Greater patient satisfaction
- Population health management
- The ability to consistently evaluate the effectiveness of treatment
- Accurate and up-to-date patient information
- Quick and easy access to patient records
- Secure exchange of information with patients and other doctors
- Increased healthcare convenience
- Improved patient and doctor interactions
- Safer prescribing
- Legible and complete documentation
- Private and secure patient information
- More time to spend with patients
- Reduced costs due to decreased paperwork, improved safety and health, and reduced duplicate testing
- Promotes preventive medicine
- Better decision-making due to integrating patient information from many sources
Stage 3 certification is a vital component of the PI Program. To meet Stage 3 requirements, all providers must use technology certified to the 2015 edition. A provider may also use EHR technology certified to both 2014 and 2015 editions. However, a 2014 edition alone will not meet the requirement starting in 2019. Failure to meet this requirement may lead to Medicare reimbursement penalties. These regulations went into effect on January 14, 2016.
The 2015 CEHRT is designed to support Stage 3 meaningful use objectives such as:
- Protection of patient health information
- Electronic prescribing
- Clinical decision support
- Computerized provider order entry
- Patient access to health information
- Coordination of care through patient engagement
- Health information exchange
- Public health and clinical data registry reporting
Certification criteria required to satisfy the 2015 edition EHR definition includes technology that has the capacity to:
- Provide clinical decision support
- Support physician order entry
- Capture and question information relevant to healthcare quality
- Exchange electronic health information with other sources
- Include patient demographic and clinical health information
The 2015 edition of CEHRT is important because it includes revisions and new capabilities that the 2014 edition does not have such as:
- Implantable device list
- Social, psychological and behavioral data
- Auditing actions on health information for privacy and security
- Exchange and reconciliation of clinical data between systems
- Patient access to data via API
For EHR software to support Stage 3 of the PI Program, it must meet all objectives. The 2015 edition allows healthcare providers to demonstrate meaningful use to its full potential. As of June 2018, over nine in 10 hospitals have 2015 edition CEHRT available from their EHR developer. Behavioral health professionals who want to benefit patients by integrating their information should use Stage 3 CEHRT.
The Certification Process
In 2016, the EMR market was $28 billion according to Kalorama Information, a market research firm, and it is projected to rise to $36.6 billion by 2021. Government incentives have helped these numbers rise. There are over 1000 EMR providers, but it is unknown how many are specially designed to suit the needs of behavioral health clinics while also satisfying Stage 3 requirements.
The ONC operates the ONC Health IT Certification Program to help make sure developers are meeting incentive program standards. The ONC does not grant certification or perform conformance testing but collaborates with other organizations that it evaluates, approves and authorizes to grant certification. The program is voluntary and was launched in 2010 to support the Medicare and Medicaid EHR Incentive Programs.
The EHR certification process is carried out in the following steps:
- The ONC issues certification criteria.
- Developers create programs that meet set standards and certification criteria.
- Programs are tested based on the standards and certification criteria.
- ONC-approved certification bodies certify successfully-tested technology.
- Certification bodies submit product information to the ONC for posting on the Certified Health IT Product list.
- Providers and hospitals use certified EHR technology.
Certified health IT products, such as 2015 CEHRT, promote interoperability better than past editions and enable health information exchange with new and enhanced capabilities.
With recent changes in the PI Program and new legislation, it’s reasonable to say behavioral health EHR incentive programs are underway. If you are a behavioral health professional excited to join the expanding network of healthcare professionals utilizing the benefits of EHR technology, ICANotes is here to help. We understand that there are a lot of rules and regulations behind the certification process, and as a professional, you want to make sure you use only the best for your patients and your staff. You might also want to avoid future penalties for not using certified EHR technology. ICANotes takes the worry out of your hands so that you can focus on other matters.
ICANotes is currently undergoing the process of completing Stage 3 certification and successfully completed certification for Stage 1 in 2011 and Stage 2 in 2014. ICANotes customers will soon be able to participate in future behavioral health incentive programs and save time, money and effort sticking to a name they know they can trust. Also, they’ll enjoy the many benefits of rigorously-tested EHR technology.
Psychologists, psychiatrists and other behavioral health professionals who are new to EHR and ready to upgrade their system can turn to ICANotes for the best EHR technology on the market. They can rest assured that their patient’s information is kept up-to-date, easily accessible and securely stored in technology that is compliant with all HIPAA regulations. By choosing a certified EHR, you’ll be prepared to participate in future incentive programs and avoid penalties.
If you’ve been excluded from the former incentive programs, or if you are currently using uncertified software, ICANotes is ready to help you transition to new technologies. Our EHR software will also help you:
- Stay at the top of your field
- Enjoy a more efficient workplace
- Keep clients satisfied
- Have more time with patients
- Spend less time with paperwork
Integrating healthcare information helps you make better decisions and provide the best patient care possible. Contact us to learn more about our Behavioral Health EHR software, start your free trial or watch a live demo today!
Related Posts:
Are Mental Health Record Guidelines the Same for Every State?
How Electronic Health Records Are Improving Patient Care
Biggest Challenges Facing Clinical Psychologists in 2018
How to Give Patients Access to Their Mental Health Records