Blog > Treatment Strategies > Assessing & Managing Suicidal Ideation in Behavioral Health
Assessing and Managing Suicidal Ideation in Behavioral Health Practice
Behavioral health clinicians face the difficult yet vital task of assessing and documenting suicide risk. This guide explains how to assess for suicidality, apply the ICD-10 code for suicidal ideation, and manage suicidal patients ethically and effectively. Learn evidence-based assessment tools, legal reporting requirements, and documentation strategies that protect both your clients and your clinical practice.

Last Updated: November 21, 2025


What You'll Learn
- How to differentiate passive vs. active suicidal ideation and identify warning signs
- The ICD-10 code for suicidal ideation (R45.851) and documentation best practices
- Evidence-based tools for assessing for suicidality (C-SSRS, SAFE-T, PHQ-9)
- Legal and ethical guidelines for when clinicians must report suicidal thoughts
- Practical steps for developing safety plans and managing suicidal patients
- How ICANotes streamlines suicide risk documentation and compliance
Contents
- Clarifying What Suicidal Ideation Means
- From Recognition to Action: The Importance of Assessing for Suicidality
- ICD-10 Coding and Documentation for Suicidal Ideation
- A Framework for Working with Suicidal Clients
- Legal, Ethical, and Reporting Considerations for Clinicians
- Embedding Suicide Risk Documentation into your EHR Workflow
- FAQs: Assessing for Suicidal Ideation
- Conclusion: Strengthening Suicide Risk Assessment and Documentation
Understanding Suicidality: A Core Clinical Responsibility
For behavioral health clinicians, few conversations carry more weight, or more risk, than those involving suicide. According to the CDC, suicide claimed more than 49,000 lives in 2022, underscoring the importance of early identification and consistent assessment of suicidal ideation in every clinical setting.
Discussing suicide with a client requires a balance of clinical skill, compassion, and structure. A well-guided conversation not only helps identify risk but also strengthens trust and safety in the therapeutic relationship.
Clarifying What Suicidal Ideation Means
Before clinicians can effectively assess or document suicide risk, it’s essential to understand what constitutes suicidal ideation, and how it differs from related concepts.
Suicidal ideation refers to thoughts about death or self-harm that can range from vague wishes not to live to detailed planning of suicide. These thoughts fall along a continuum from passive to active ideation:
- Passive suicidal ideation: A wish to die without intent or a plan (e.g., “I wish I wouldn’t wake up tomorrow”).
- Active suicidal ideation: Specific thoughts about suicide, often accompanied by intent or preparation (e.g., “I’ve thought about taking an overdose”).
Clinicians must also differentiate suicidal ideation from suicidal intent. Ideation concerns the content of thoughts; intent involves the motivation and likelihood of acting on them. Understanding this distinction helps clinicians gauge immediacy of risk and determine the level of intervention required.
Free Download:
Suicide Risk Assessment Guide
Turn tough conversations into a clear, defensible workflow. Get scripts, checklists, and templates that help you assess, document, and plan for safety in one visit.
What you’ll get
-
Conversation prompts (what to ask—and what to avoid)
-
A ready-to-use Suicidal Ideation Checklist to spot red flags fast
-
Plug-and-play Safety Plan and Treatment Plan templates
From Recognition to Action: The Importance of Assessing for Suicidality
Once suicidal ideation is recognized, the next step is a structured assessment to determine the immediacy and severity of risk, as outlined in Step 1 of the six-step crisis intervention process. While clinical intuition and rapport play important roles, standardized instruments provide the reliability, objectivity, and documentation consistency that behavioral health settings require.
At the same time, assessment is not an endpoint. When suicidal ideation is present, clinicians must be prepared to move from evaluation to intervention using a structured, safety-focused framework to guide clinical decision-making and next steps.
These tools help clinicians assess not just if suicidal ideation exists, but how serious, persistent, and actionable it may be. Incorporating one or more into your evaluation process ensures that your clinical decisions are both evidence-based and defensible.
Validated Screening Tools
1. Columbia-Suicide Severity Rating Scale (C-SSRS)
The C-SSRS is one of the most widely used suicide risk screening tools worldwide. It assesses the full spectrum of suicidality, from passive wishes to die to active attempts, through a series of structured questions.
It can be administered verbally or in writing, making it ideal for intake, follow-up sessions, and crisis assessments. The scale evaluates four key dimensions:
- The severity of ideation (ranging from passive to active intent)
- The frequency and duration of suicidal thoughts
- Any preparatory behaviors or attempts
- The immediacy of risk based on client responses
Using the C-SSRS within your EHR ensures consistent phrasing, quantifiable data, and defensible documentation that can be tracked over time.
2. SAFE-T (Suicide Assessment Five-Step Evaluation and Triage)
Developed by SAMHSA and the Suicide Prevention Resource Center, the SAFE-T protocol is both a guide and a decision-making framework. Rather than a single questionnaire, it outlines a five-step process that integrates risk factors, protective factors, and clinical judgment:
- Identify risk factors (psychiatric disorders, substance use, recent stressors).
- Identify protective factors (social supports, coping skills, reasons for living).
- Conduct a direct suicide inquiry (thoughts, plans, behaviors, intent).
- Determine risk level and select interventions.
- Document and follow up.
SAFE-T is particularly useful for clinicians who want a repeatable structure that aligns with both ethical and documentation standards. It’s ideal for embedding into ICANotes templates, ensuring every session involving suicide risk follows a consistent, comprehensive framework.
3. Patient Health Questionnaire–9 (PHQ-9)
While not designed specifically for suicide assessment, the PHQ-9 is a cornerstone of routine mental health screening.
Item 9 (“Thoughts that you would be better off dead, or of hurting yourself in some way”) functions as an early warning flag.
A positive response here should always prompt further exploration using a more detailed tool such as the C-SSRS or SAFE-T.
Because the PHQ-9 is widely accepted by insurers and care networks, documenting follow-up after a positive Item 9 response helps demonstrate medical necessity and risk management diligence, both of which support reimbursement and clinical compliance.
Helpful Clinical Prompts for Discussing Suicidality
While validated screening tools add reliability and consistency, they don’t replace the human element of assessment. Clients often disclose suicidal thoughts only when they feel truly heard and understood. Empathic dialogue allows clinicians to interpret subtle cues, clarify meaning, and gauge the depth of intent that may not surface on a checklist.
These prompts are designed to help you explore suicidal ideation in a way that feels natural, collaborative, and clinically effective. They can be used before, during, or after a formal screening to expand on the client’s responses.
Opening the Conversation
Begin with nonjudgmental, open-ended questions that normalize the topic and invite honesty.
“Sometimes when people feel overwhelmed, they think about death or not wanting to live. Have you had any thoughts like that lately?”
“When things get really difficult, do you ever find yourself wishing you could escape or not wake up?”
This approach validates the client’s experience while gently introducing the topic without leading or assuming risk.
Related: Watch our on-demand webinar: Compassionate Conversations: Navigating Suicidal Ideation with Clients
Exploring the Nature of Ideation
Once a client acknowledges suicidal thoughts, shift to clarifying frequency, duration, and control.
“How often do these thoughts come up for you?”
“When you notice these thoughts, how intense are they?”
“Do you find that you can dismiss them, or do they feel intrusive or overwhelming?”
These questions help you differentiate fleeting, passive ideation from active, persistent, or intrusive thoughts that signal higher risk.
Assessing Intent, Planning, and Means
Move gradually from ideation to intent and preparation, maintaining empathy and calm throughout.
“Have you thought about how you might act on those thoughts?”
“Have you made any preparations or taken steps toward a plan?”
“Do you have access to any means that concern you — such as medications, weapons, or other items?”
These questions mirror the C-SSRS structure and help you assess not just whether ideation exists, but how close it is to action.
Identifying Protective Factors
Always balance risk exploration with questions about reasons for living and sources of hope.
“What helps you hold on or stay safe when these thoughts come up?”
“Who or what gives your life a sense of meaning or responsibility?”
“If you’ve had these thoughts before, what helped you get through that time?”
These questions remind clients of internal and external supports and offer crucial documentation points for protective factors in your EHR note.
Closing the Discussion
End the assessment by collaboratively summarizing what was discussed and emphasizing safety.
“I appreciate your honesty in sharing this with me. Let’s talk together about how we can keep you safe right now.”
This closing reinforces the therapeutic alliance and sets the stage for the next phase — safety planning and documentation.

Clinical Documentation Tip
When documenting these conversations, include both the content (what was said) and your clinical impression (tone, affect, risk judgment). For example:
“Client reports intermittent passive suicidal ideation without current plan or intent. States, ‘Sometimes I wish I could just sleep and not wake up.’ Protective factors include family support and commitment to therapy. Denies access to lethal means.”
ICD-10 Coding and Documentation for Suicidal Ideation
Accurate documentation turns compassionate conversation into a defensible clinical record. The ICD-10 code for suicidal ideation is R45.851, and it should be used alongside any primary mental health diagnosis contributing to risk — such as depression (F32–F33), PTSD (F43.1x), or substance use disorder (F10–F19).
When documenting suicidal ideation:
- Quote the client’s own words where possible.
- Specify intent and planning level (passive vs active ideation and presence or absence of plan or means).
- Note protective factors and strengths (e.g., family, pets, faith).
- Describe clinical interventions and safety planning steps.
- Record consultations and supervision when applicable.
This level of detail not only supports continuity of care but also protects clinicians in the event of audit or legal review. Structured EHR templates — such as those in ICANotes — can simplify this process with pre-configured menus that ensure every element, from ideation to safety plan, is clearly recorded.
A Framework for Working with Suicidal Clients
After assessment, clinicians must transition from identifying risk to actively managing it. The following framework offers a natural progression from immediate safety to long-term stabilization.
1. Know the Laws and Ethical Standards
Every state defines the clinician’s duty to protect differently. Review local regulations and professional guidelines so that you can act decisively when a client’s safety is at stake.
2. Prepare for the Discussion
Approach the topic calmly and non-judgmentally. Framing suicide as a symptom of distress rather than moral failure helps reduce shame and invites honesty.
3. Build Rapport and Normalize the Conversation
Express empathy: “I’m glad you told me; these thoughts are painful, and we’ll work through them together.” Validation decreases isolation and sets the stage for collaborative planning.
4. Evaluate Risk and Protective Factors
Gather a complete picture of both danger and safety. Access to means, previous attempts, and hopelessness indicate risk, while supportive relationships and a sense of purpose often mitigate it. Use the following table of common risk and protective factors as a framework to:
- Guide assessments: Document both risk and protective factors to balance clinical judgment.
- Support treatment planning: Align goals around strengthening protective factors (e.g., social connection, coping skills).
- Enhance documentation quality: Integrate these terms into progress notes or risk assessment templates for defensibility.
- Develop safety plans: Focus interventions on modifiable risk factors — especially access to lethal means and hopelessness.
Common Risk and Protective Factors for Suicidal Ideation
Use this quick-reference table to document balanced suicide risk assessments and inform safety planning.
| Risk Factors | Examples / Clinical Indicators | Protective Factors | Examples / Clinical Indicators |
|---|---|---|---|
| Mental Health Disorders | Major depression, bipolar disorder, PTSD, anxiety, schizophrenia | Strong Therapeutic Alliance | Trust and ongoing engagement with a clinician or treatment team |
| Previous Suicide Attempt | History of prior attempt(s) or self-harm behaviors | Social Support and Connection | Supportive family, friends, peer networks, or community involvement |
| Substance Use Disorders | Alcohol or drug misuse increasing impulsivity or disinhibition | Sense of Purpose or Responsibility | Commitment to children, pets, faith, or meaningful life roles |
| Hopelessness or Despair | Expressions of worthlessness, feeling trapped, or perceiving no future | Effective Coping Skills | Use of problem-solving, emotion regulation, or mindfulness techniques |
| Access to Lethal Means | Availability of firearms, medications, or other means | Restricted Access to Means | Safe storage or removal of medications and firearms; means reduction |
| Chronic Pain or Serious Illness | Long-term pain, disability, or terminal conditions | Engagement in Mental Health Treatment | Consistent therapy attendance, adherence to medication, use of crisis supports |
| Trauma or Adverse Life Events | Abuse, neglect, loss, relationship conflict, financial stress, legal issues | Cultural or Religious Beliefs Discouraging Suicide | Faith-based values, community identity, moral convictions promoting resilience |
| Social Isolation | Living alone, lack of belonging, or withdrawal from relationships | Problem-Solving & Conflict-Resolution Skills | Ability to manage stressors or seek help before crisis |
| Recent Discharge from Psychiatric Care | Transition gaps in care, limited follow-up, medication nonadherence | Access to Behavioral Health Resources | Knowledge of crisis lines, outpatient supports, and safety-planning tools |
5. Create a Collaborative Safety Plan
Work with the client to identify personal warning signs, coping strategies, crisis contacts (including the 988 Suicide & Crisis Lifeline), and professional resources. Avoid “no-harm contracts”; evidence shows that collaborative planning is far more effective.
Related: Mental Health Safety Planning: Why It's No Longer Optional for Clinicians
6. Document Every Step
Include not only what was said but your reasoning for each clinical decision. Documentation demonstrates sound judgment and fulfills ethical and legal standards.

Example Documentation Entry
“Client presents with moderate suicide risk due to major depressive episode, recent job loss, and passive suicidal ideation. Protective factors include strong family support and willingness to engage in therapy. Denies access to firearms. Safety plan reviewed and updated.”
7. Plan and Implement Targeted Interventions
Once immediate safety has been established, the next step is to develop a comprehensive treatment plan that addresses both acute risk and the underlying causes of suicidal ideation. Effective treatment planning involves aligning goals, objectives, and interventions that are specific, measurable, and documented clearly within the client’s chart.
Core Components of a Suicide-Focused Treatment Plan
Problem/Need Statement: Describe the nature of suicidal ideation and contributing factors (e.g., depression, trauma, hopelessness, isolation).
Goal: Support the client in achieving safety and improving mood stability through ongoing therapy and skill development.
Objectives:
- Identify triggers that increase suicidal thoughts.
- Strengthen coping and distress-tolerance skills.
- Engage in regular therapy and medication management.
- Increase connection with supportive people or activities.
Interventions:
- Implement cognitive-behavioral strategies to reduce hopelessness and self-critical thoughts.
- Use DBT emotion-regulation and mindfulness skills for crisis management.
- Create and update a collaborative safety plan during each high-risk period.
- Coordinate care with prescribers, case managers, or family supports as appropriate.
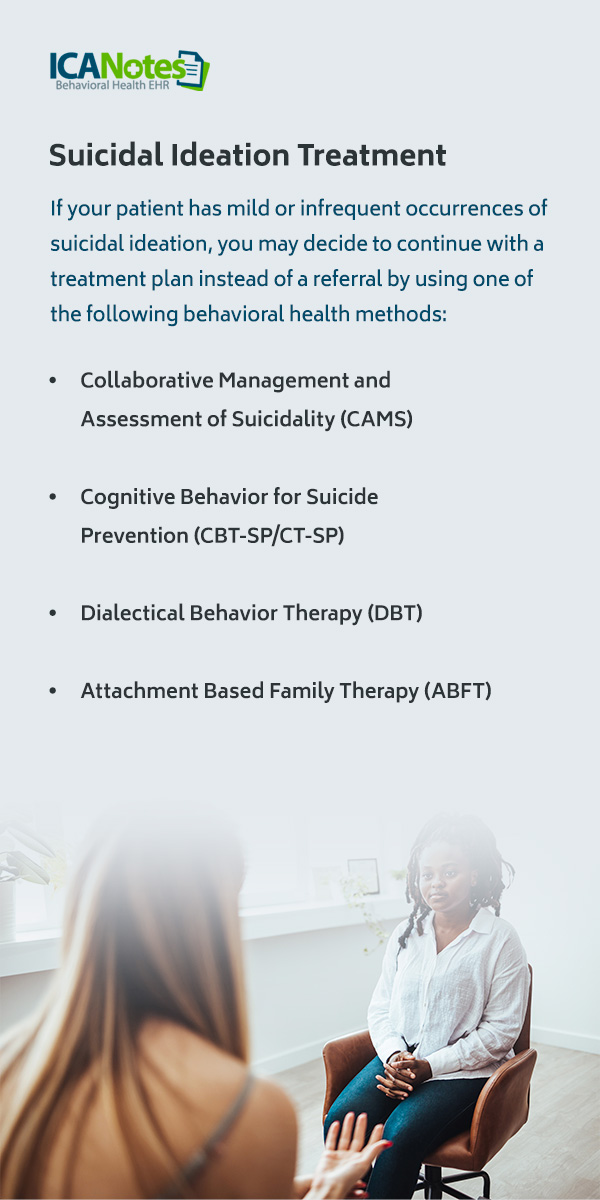
Evidence-Based Treatment Approaches
Clinicians may choose interventions drawn from empirically supported models:
- Dialectical Behavior Therapy (DBT): Helps clients tolerate distress and manage self-destructive urges.
- Collaborative Assessment and Management of Suicidality (CAMS): Focuses on understanding the function of suicidal thoughts and building individualized coping plans.
- Cognitive Behavioral Therapy for Suicide Prevention (CBT-SP): Targets distorted thinking and teaches behavioral activation techniques.
- Attachment-Based Family Therapy (ABFT): Helps adolescents and parents rebuild trust and emotional communication, directly addressing relational ruptures that contribute to suicidal thoughts.
Documenting Treatment Progress
Each session should capture the client’s progress toward goals and any change in risk level. For example:
“Client demonstrated improved ability to use distress-tolerance skills when experiencing intrusive suicidal thoughts. Reports decreased frequency of ideation since last session. Continues to engage in DBT group and safety-plan review.”
EHR systems like ICANotes make this process easier by linking goals, objectives, and interventions directly to progress notes, ensuring every entry supports medical necessity and continuity of care.
8. Management of the Suicidal Patient: From Risk to Recovery
Effective management of suicidal ideation begins with identifying the level of risk and matching interventions to the client’s safety needs. Clinicians should consider both the immediacy of danger and the client’s protective factors when deciding on next steps.
Low to Moderate Risk
- Develop a collaborative safety plan (avoid “no-harm” contracts).
- Identify coping strategies and crisis contacts (988 Suicide & Crisis Lifeline).
- Increase session frequency; involve supports as appropriate.
High or Imminent Risk
- Conduct or facilitate an emergency evaluation.
- Coordinate with crisis response teams or inpatient facilities.
- Document rationale and steps taken; plan follow-up post-discharge.
Evidence-based interventions such as DBT, CAMS, CBT-SP, and ABFT are shown to reduce suicidal behaviors. ABFT, in particular, focuses on repairing attachment ruptures and strengthening family bonds — key protective factors for adolescents experiencing suicidal ideation.
Legal, Ethical, and Reporting Considerations for Clinicians
Clinicians often ask: When do therapists have to report suicidal thoughts? The duty to protect or warn arises when a client presents imminent risk — for example, if they have both intent and a plan and the means to carry it out.
Suicidality Best Practices
- Clearly document your risk assessment and decision-making process.
- Consult with supervisors or colleagues when uncertain.
- Inform clients of your obligation to act if safety is at risk.
- When necessary, contact emergency services or arrange for hospitalization.
Documentation should include the rationale for actions taken or not taken. A well-documented record is a clinician’s best protection in high-risk situations.
Related: Suicide Risk: Documentation, Duty to Warn, and Forseeability
Embedding Suicide Risk Documentation into Your EHR Workflow
Behavioral health clinicians must ensure that every stage of treatment, from assessment to intervention, is reflected in defensible documentation.
With ICANotes, you can:
- Document suicide risk assessments using structured templates aligned with clinical standards.
- Auto-populate billing codes (including R45.851 for suicidal ideation).
- Track interventions and safety plans over time.
- Maintain a complete audit trail to demonstrate compliance and continuity of care.
Example documentation language:
“Client reports passive suicidal ideation, denies active intent or plan. Protective factors include strong family support. Crisis resources reviewed; safety plan developed collaboratively.”
FAQs: Assessing for Suicidal Ideation
Conclusion: Strengthening Suicide Risk Assessment and Documentation
Behavioral health clinicians must ensure that every stage of treatment, from assessment to intervention, is reflected in defensible documentation.
With ICANotes, you can:
- Document suicide risk assessments using structured templates aligned with clinical standards.
- Auto-populate billing codes (including R45.851 for suicidal ideation).
- Track interventions and safety plans over time.
- Maintain a complete audit trail to demonstrate compliance and continuity of care.
Example documentation language:
“Client reports passive suicidal ideation, denies active intent or plan. Protective factors include strong family support. Crisis resources reviewed; safety plan developed collaboratively.”
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
- Complete Notes in Minutes - Purpose-built for behavioral health charting
- Always Audit-Ready – Structured documentation that meets payer requirements
- Keep Your Schedule Full – Automated reminders reduce costly no-shows
- Engage Clients Seamlessly – Secure portal for forms, messages, and payments
- HIPAA-Compliant Telehealth built into your workflow
Complete Notes in Minutes – Purpose-built for behavioral health charting
Always Audit-Ready – Structured documentation that meets payer requirements
Keep Your Schedule Full – Automated reminders reduce costly no-shows
Engage Clients Seamlessly – Secure portal for forms, messages, and payments
HIPAA-Compliant Telehealth built into your workflow
Related Posts
About the Author
Dr. October Boyles is a behavioral health expert and clinical leader with extensive expertise in nursing, compliance, and healthcare operations. With a Doctor of Nursing Practice (DNP) and advanced degrees in nursing, she specializes in evidence-based practices, EHR optimization, and improving outcomes in behavioral health settings. Dr. Boyles is passionate about empowering clinicians with the tools and strategies needed to deliver high-quality, patient-centered care.









