Blog > Documentation > Mental Health Documentation Guidelines & Cheat Sheet
Mental Health Documentation Best Practices: Guidelines & Cheat Sheet
In behavioral health and therapy, strong mental health documentation is more than record-keeping — it’s the backbone of consistent, safe, and defensible care. Clinicians rely on these notes to track progress, coordinate care, fulfill regulatory and billing requirements, and protect themselves legally. In this guide, we’ll walk through essential mental health documentation guidelines, share a mental health documentation cheat sheet, and offer best practices to elevate your documentation from good to excellent.

Last Updated: October 3, 2025


What You'll Learn
-
Why quality mental health documentation is essential for care, compliance, billing, and risk management
-
The core components every clinical note should include, with examples
-
Best practices for writing defensible, client-centered notes that align with mental health documentation guidelines
-
A practical, printable mental health documentation cheat sheet to use as a quick reference in daily practice
-
Tips for streamlining documentation with EHR tools and templates
Contents
Why Quality Mental Health Documentation Matters
General Process for Mental Health Documentation - Intake to Discharge
The Do's and Don'ts of Clinical Documentation
Documentation Requirements for Insurance Reimbursement
Other Mental Health Documentation Principles To Remember
Tips for Improving Behavioral Health Documentation
FAQs: Mental Health Documentation
Final Thoughts: Simplify Mental Health Documentation with ICANotes
Why Quality Mental Health Documentation Matters
Quality mental health documentation does more than record sessions — it supports clinical care, compliance, and professional accountability. Here are four key reasons why writing good notes matters.
1. Continuity of Care and Clinical Insight
Well-written notes help any clinician (or future you) quickly understand a client’s history, treatment trajectory, and clinical decisions.
2. Legal, Ethical, and Risk Management Defense
Documentation serves as your “best defense” if questions arise about treatment decisions or care continuity. In fact, experts recommend completing notes within 48 hours, when details are still fresh.
3. Justification for Billing and Medical Necessity
Strong documentation demonstrates that the sessions and interventions were necessary and appropriate, which is often required by payers and auditors.
4. Professional Accountability and Quality Control
Following mental health documentation guidelines helps standardize care, reduces ambiguity, and makes audits or peer reviews smooth.
General Process for Mental Health Documentation — Intake to Discharge
Effective mental health documentation isn’t just about keeping records—it follows a structured process that mirrors the client’s journey in treatment. By applying consistent mental health documentation guidelines from the first intake form to the final discharge summary, clinicians create records that are defensible, compliant, and clinically useful.
Below is a step-by-step outline of the general process for documenting client care.
1. Intake Documentation
At the intake stage, clinicians gather a wide range of baseline information: presenting concerns, personal and family psychiatric history, medical history, risk factors, and consent forms. This documentation establishes the foundation for treatment and ensures that the client’s care begins with a clear, informed baseline.
- Best Practice Tip: Always document informed consent and confidentiality agreements as these are key legal protections.
- For a complete guide to conducting a successful client intake, please read our related post: A Guide to Successful Mental Health and Psychiatry Intake
2. Initial Assessment Notes
Assessment documentation captures your clinical impressions and diagnostic reasoning. This may include results from standardized screening tools, observations from a mental status exam, and diagnostic impressions. Strong assessment notes justify the need for care and support medical necessity requirements for billing and insurance.
- Best Practice Tip: Link assessments directly to treatment goals for a clear "golden thread" in your documentation.
- Read our related articles for detailed guidance on writing a biopsychosocial assessment or initial psychiatric evaluation.
2. Treatment Planning
A treatment plan is the roadmap for care. It should include individualized, measurable goals, planned interventions, and expected outcomes. Documenting treatment plans in line with mental health documentation guidelines ensures alignment with payer expectations and provides a framework to measure progress.
- Best Practice Tip: Write goals that are SMART (Specific, Measurable, Achievable, Relevant, Time-bound).
- For more detailed information, read our related Guide to Creating Mental Health Treatment Plans.
3. Ongoing Progress Notes
Progress notes document what occurs in each session, including session details, interventions used, and the client’s response. Using structured formats like SOAP, DAP, or BIRP notes helps maintain consistency and defensibility. Thorough progress notes support continuity of care, demonstrate ongoing medical necessity, and protect clinicians in the event of an audit.
- Best Practice Tip: Use objective language — focus on observable behaviors and direct client quotes rather than vague impressions.
- For more information on writing the best progress notes, review our related articles:
How to Write Progress Notes That are Clear, Compliant, and Clinically Useful
How to Write Psychiatric Progress Notes Efficiently and Effectively
Therapist Notes: Complete Guide to Documentation Types & Best Practices
Core Components: What to Include in Your Notes
A high-quality mental health note should include the following elements (adapted from standard templates like SOAP, DAP, and BIRP).
| Section | What to Document | Why It Matters |
|---|---|---|
| Session Details | Date, time (start/stop), location, provider name/credentials, client identifiers | Ensures clarity and audit compliance |
| Subjective (S / Data / Behavior) | What the client says or reports; include direct quotes when relevant | Shows authenticity and the client’s voice |
| Objective (O / Observations) | Observable behavior and MSE indicators (appearance, speech, affect, thought process) | Grounds clinical impressions in facts |
| Assessment / Interpretation | Clinician’s interpretation of status, progress, barriers; diagnostic reasoning | Connects data to clinical decision-making |
| Interventions / Treatment | Techniques or approaches used (e.g., CBT, DBT, MI) and rationale | Demonstrates active therapeutic work |
| Response / Client Reaction | Client’s response to interventions (e.g., engaged, resistant, emotional) | Shows progress or lack thereof |
| Plan / Next Steps | Goals, homework, referrals, safety plan, next appointment | Keeps treatment moving forward |
| Diagnosis & Codes | DSM/ICD diagnosis and applicable billing codes (when relevant) | Supports clarity, coordination, and billing |
| Safety / Risk Assessment | Any suicidal ideation, self-harm risk, or risk to others; mitigation steps | Essential for client safety and liability reduction |
4. Discharge Summaries
At the end of treatment, discharge documentation provides a summary of care, client progress, remaining challenges, and aftercare recommendations. Discharge summaries are critical for both legal protection and continuity of care if the client transitions to another provider.
- Best Practice Tip: Document reasons for discharge (e.g., treatment goals met, referral, non-compliance) and include specific aftercare recommendations.
- Read our related article for detailed guidance on writing a mental health discharge summary.
Why This Process Matters
Following a clear, consistent mental health documentation process from intake to discharge ensures:
-
Clinical notes that meet professional and ethical standards
-
Compliance with payer and regulatory requirements
-
Continuity of care across providers and treatment stages
-
Protection for clinicians in case of audits, reviews, or legal concerns
For a quick reference, use our Mental Health Documentation Cheat Sheet to keep each stage clear, consistent, and defensible in your daily practice.
Access Our Sample Notes Library
Get instant access to our full library of sample behavioral health notes, including Initial Evaluations, Progress Notes, Treatment Plans, and Discharge Summaries. We have note samples for psychiatry, therapy, case management, PRP, substance abuse, group therapy, couples therapy, and more!
The Do's and Don'ts of Clinical Documentation
Following clear mental health documentation guidelines helps ensure your notes are professional, defensible, and clinically valuable. Use these do’s and don’ts as a quick reference when writing progress notes, treatment plans, and discharge summaries.
✅ Do’s of Mental Health Documentation
-
Do document promptly. Complete your notes within 24–48 hours to maintain accuracy and compliance with best practice standards.
-
Do use objective, descriptive language. Record observable behaviors (e.g., “client appeared tearful, with slow speech”) rather than vague impressions (“seemed upset”).
-
Do link notes to the treatment plan. Maintain the “golden thread” by tying progress notes and interventions directly to client goals.
-
Do include client strengths and progress. Highlight resilience and improvement alongside challenges to present a balanced clinical picture.
-
Do quote clients when appropriate. Direct quotes add authenticity and show that notes reflect the client’s own words.
-
Do ensure confidentiality. Protect client privacy by following HIPAA standards and limiting details to those clinically relevant.
-
Do use structured formats. SOAP, DAP, or BIRP templates promote consistency and align with common mental health documentation guidelines.
❌ Don’ts of Mental Health Documentation
-
Don’t use vague terms or jargon. Avoid words like “doing better” or shorthand that could be unclear to others reviewing the record.
-
Don’t include unnecessary personal details. Stick to clinically relevant information and avoid speculation.
-
Don’t alter or backdate notes. If corrections are necessary, make them transparently with dates and initials.
-
Don’t copy and paste previous notes. Each entry should reflect the unique session and client’s current status.
-
Don’t overlook risk factors. Always document suicidal ideation, self-harm, or harm-to-others risk thoroughly.
-
Don’t let notes pile up. Writing retroactively increases the risk of incomplete or inaccurate documentation.
-
Don’t forget signatures. Every entry should be dated and signed (or electronically authenticated in your EHR).
Applying these do’s and don’ts makes clinical notes clear, defensible, and aligned with mental health documentation best practices. By avoiding common pitfalls and sticking to proven strategies, clinicians can reduce liability, support billing requirements, and most importantly, deliver better client care.
Get Our Free Mental Health Documentation Cheat Sheet
Stronger notes mean better care — and fewer compliance headaches. Download our free quick-reference guide to learn what to include, what to avoid, and how to stay payer-ready from intake to discharge.
Documentation Requirements for Insurance Reimbursement
When it comes to billing, mental health documentation isn’t just about clinical accuracy — it’s also the proof payers require to authorize and reimburse services. Insurers look for specific elements in your notes to confirm that treatment is medically necessary, delivered as described, and compliant with regulatory standards. Failing to meet these mental health documentation guidelines can lead to denied claims, delayed payments, or even audits.
Key Documentation Elements for Insurance Claims
To support reimbursement, every clinical note should include:
-
Date and session details – Start and end time, type of service (e.g., psychotherapy, medication management), and whether the session was in person or telehealth.
-
Diagnosis codes – Document DSM-5/ICD-10 diagnoses clearly, as payers require coding that matches billed services.
-
Treatment plan linkage – Progress notes must connect back to goals and interventions in the treatment plan, showing the “golden thread” of care.
-
Medical necessity – Include clinical observations, client reports, and your interpretation that justify why the session was needed at that time.
-
Interventions provided – List techniques used (e.g., CBT, trauma-focused interventions) and client response.
-
Risk assessment – Note suicidal ideation, self-harm, or safety concerns when relevant, along with interventions taken.
-
Provider credentials and signature – Ensure each entry is signed (or electronically authenticated) with the correct professional designation.
Common Pitfalls That Lead to Denials
Insurance reviewers are trained to flag notes that don’t meet minimum requirements. Avoid these errors:
-
Vague documentation (e.g., “Client doing better” instead of measurable change)
-
Copy-pasted notes across sessions that fail to reflect actual progress
-
Missing treatment plan references, making it unclear how today’s session ties into the care plan
-
Omissions of session times, dates, or signatures
-
Lack of justification for medical necessity, especially for longer or higher-frequency sessions
Best Practices to Stay Compliant
-
Write notes promptly — within 24–48 hours — while details are fresh.
-
Use structured templates (SOAP, DAP, or BIRP) that align with mental health documentation guidelines.
-
Review payer-specific requirements; Medicare, Medicaid, and commercial insurers may have unique criteria.
-
Audit your documentation monthly to ensure billing alignment.
-
Leverage your EHR’s built-in tools to automate time-stamps, signatures, and treatment plan linkages.
Thorough documentation doesn’t just improve care — it ensures you get paid for the services you provide. By following these mental health documentation requirements for insurance reimbursements, clinicians reduce claim denials, protect revenue, and stay audit-ready. For a quick reference, keep our mental health documentation cheat sheet handy to double-check that each note includes all required elements.
Other Mental Health Documentation Principles to Remember
Beyond the essentials, there are additional mental health documentation guidelines that help ensure your notes are accurate, defensible, and clinically meaningful. These principles apply across all types of records — from intake notes to discharge summaries — and can help protect both client care and clinician liability.
Key Principles
-
Keep notes timely and accurate. Complete documentation as soon as possible after sessions (ideally within 24–48 hours) to ensure accuracy and compliance.
-
Maintain confidentiality. Follow HIPAA standards by documenting only clinically relevant information and avoiding unnecessary personal details.
-
Use clear, professional language. Avoid slang, jargon, or vague phrasing. Notes should be written so that another clinician or reviewer could easily understand the client’s presentation and your clinical decisions.
-
Focus on objectivity. Record observable behaviors and client quotes rather than interpretations alone. For example, write “client reported feeling anxious and was visibly shaking” instead of “client seemed nervous.”
-
Document risk consistently. Always include information about suicidal ideation, self-harm, or risk to others when applicable, along with your clinical response.
-
Highlight progress and setbacks. Capture both improvements and challenges to create a balanced, defensible record of care.
-
Ensure legibility and completeness. For handwritten notes, write clearly. For EHR notes, avoid excessive copy-pasting and make sure every section is complete.
-
Link to the treatment plan. Reinforce the “golden thread” by documenting how each session connects to established goals.
Why These Principles Matter
Applying these principles makes your notes clinically stronger, more legally defensible, and better aligned with mental health documentation best practices. Following consistent guidelines also reduces the risk of payer denials, supports continuity of care, and ensures that your documentation tells a clear, cohesive story of the client’s treatment journey.
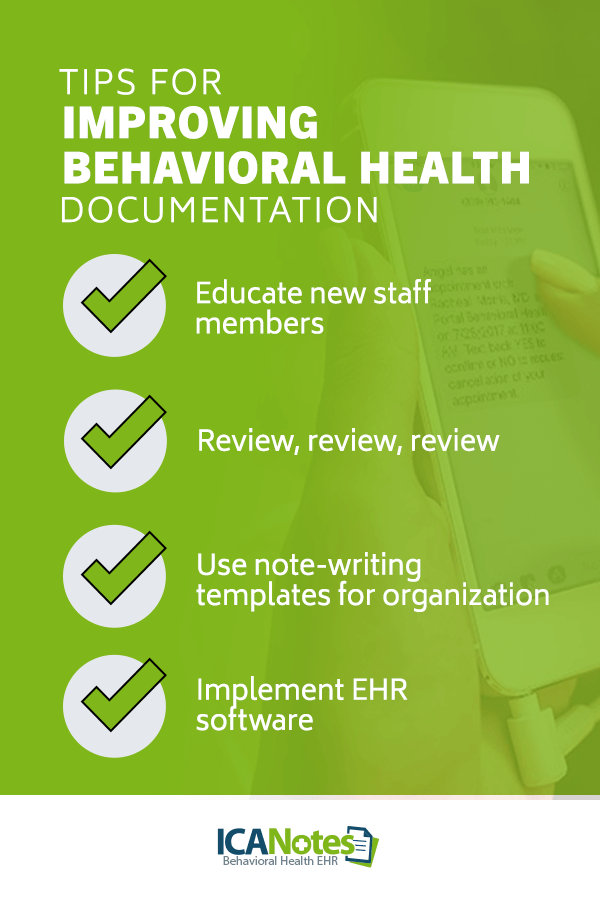
Tips for Improving Behavioral Health Documentation
Strengthening mental health documentation is about more than checking boxes — it’s about creating records that are efficient, accurate, and defensible. These practical tips can help clinicians and organizations elevate their documentation practices.
1. Educate and Train New Staff
Provide training for new team members on mental health documentation guidelines and your organization’s preferred note formats. A structured onboarding process reduces errors, promotes consistency, and ensures compliance from day one.
2. Review and Audit Documentation Regularly
Schedule periodic peer reviews or supervisor audits of notes. This not only helps catch missing elements but also reinforces best practices and provides opportunities for staff feedback and growth.
3. Use Plain, Professional Language
Write notes in clear, jargon-free language that another clinician, auditor, or payer can understand. Avoid slang or vague wording — clarity builds trust and reduces misinterpretation.
4. Capture Client Strengths and Context
Don’t just record symptoms or challenges. Document client strengths, resilience, and contextual factors (e.g., support systems, coping strategies) to give a more complete picture of their progress.
5. Leverage Technology Thoughtfully
Take advantage of your EHR’s features such as phrase banks, drop-down menus, and AI-powered tools. These can reduce documentation time while still supporting accurate and compliant notes.
Why These Tips Work
By focusing on staff education, quality review, clear language, and the thoughtful use of technology, clinicians can improve behavioral health documentation in ways that enhance compliance and efficiency — without adding unnecessary burden. These principles, paired with consistent training, ensure documentation supports both excellent care and reliable reimbursement.
Frequently Asked Questions: Mental Health Documentation Guidelines
Final Thoughts: Simplify Mental Health Documentation with ICANotes
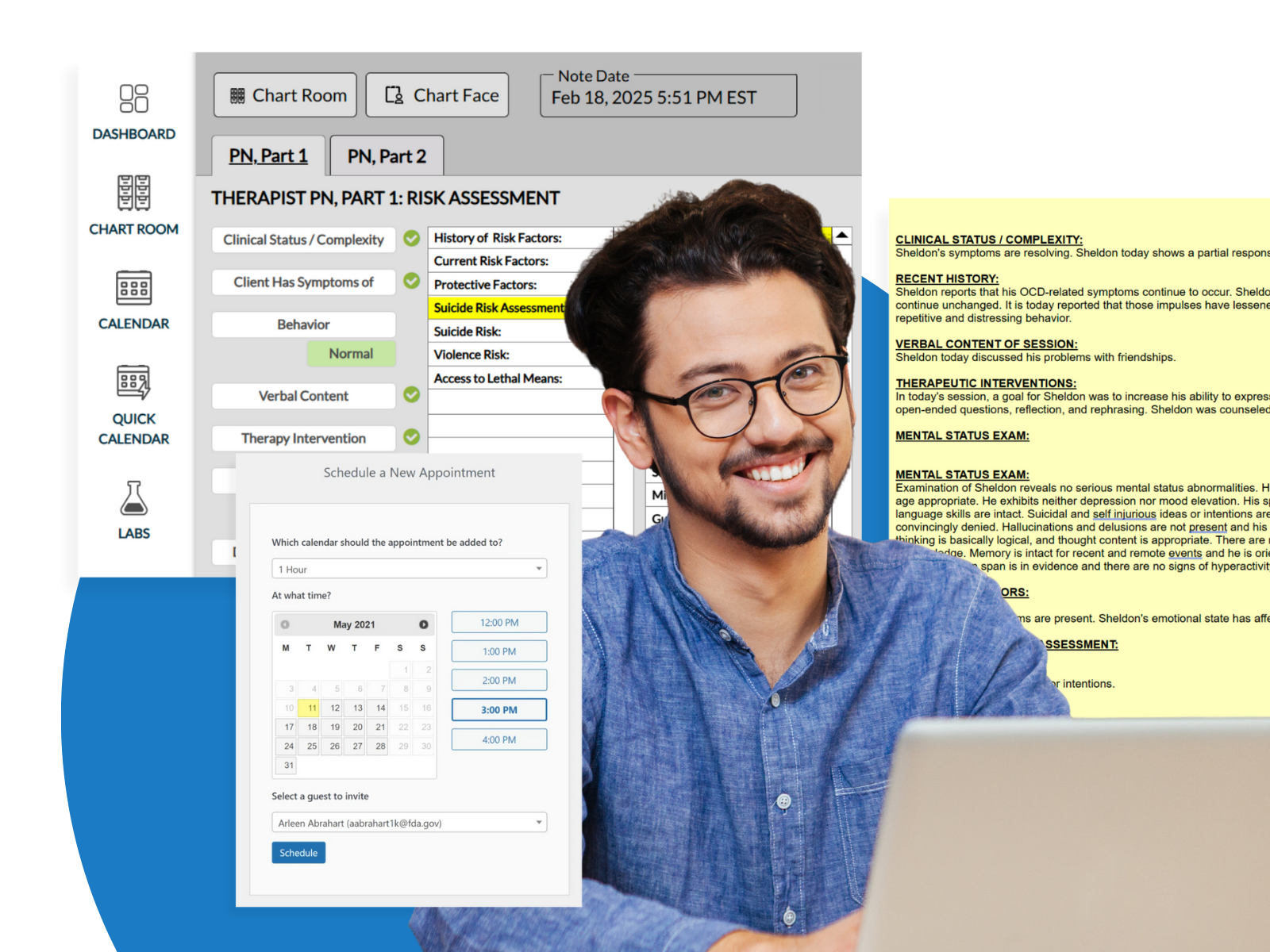
Strong mental health documentation is the foundation of effective, compliant, and defensible care. Yet for many clinicians, keeping up with detailed requirements, while still focusing on clients, can feel overwhelming. That’s where ICANotes makes the difference.
ICANotes is designed specifically for behavioral health professionals, with features that support every step of the documentation process. From intake to discharge, ICANotes provides structured menu-driven templates, built-in rating scales, and smart tools that help you maintain the “golden thread” and demonstrate medical necessity with ease. Our intuitive, menu-driven note builder saves time while ensuring your records meet mental health documentation guidelines and payer requirements — so you can focus less on paperwork and more on your clients.
Whether you’re a solo practitioner or part of a larger practice, ICANotes helps you streamline documentation, reduce errors, and stay audit-ready. Start your free trial today and see how ICANotes can transform the way you document, bill, and deliver care.
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
- Complete Notes in Minutes - Purpose-built for behavioral health charting
- Always Audit-Ready – Structured documentation that meets payer requirements
- Keep Your Schedule Full – Automated reminders reduce costly no-shows
- Engage Clients Seamlessly – Secure portal for forms, messages, and payments
- HIPAA-Compliant Telehealth built into your workflow
Complete Notes in Minutes – Purpose-built for behavioral health charting
Always Audit-Ready – Structured documentation that meets payer requirements
Keep Your Schedule Full – Automated reminders reduce costly no-shows
Engage Clients Seamlessly – Secure portal for forms, messages, and payments
HIPAA-Compliant Telehealth built into your workflow
Related Posts
About the Author
Dr. October Boyles is a behavioral health expert and clinical leader with extensive expertise in nursing, compliance, and healthcare operations. With a Doctor of Nursing Practice (DNP) and advanced degrees in nursing, she specializes in evidence-based practices, EHR optimization, and improving outcomes in behavioral health settings. Dr. Boyles is passionate about empowering clinicians with the tools and strategies needed to deliver high-quality, patient-centered care.