Blog > Documentation > Writing Effective Psychiatric Progress Notes
How to Write Psychiatric Progress Notes Efficiently and Effectively
Creating high-quality psychiatric progress notes is essential for delivering safe, effective, and compliant mental health care. These notes serve as a legal record, a communication tool between providers, and a foundation for clinical decision-making. But for psychiatrists and other behavioral health professionals, documentation can become a time-consuming burden—especially when juggling packed caseloads.

Last Updated: May 14, 2025

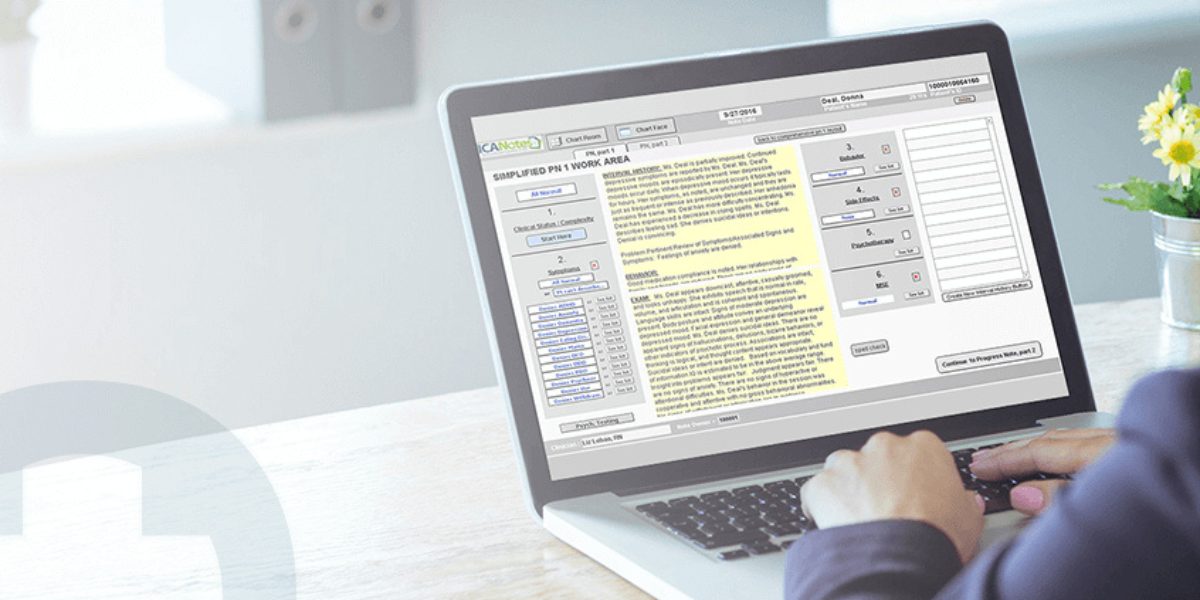
That’s where ICANotes comes in. As a behavioral health EHR designed specifically for psychiatrists, ICANotes simplifies the note-writing process with customizable templates, point-and-click menus, and clinically validated language. The result? You can produce thorough, defensible psychiatric notes in just minutes—with less typing, fewer errors, and better support for treatment and reimbursement.
Why Efficient Psychiatric Notes Matter
Efficient psychiatric notes help you:
-
Reduce time spent documenting
-
Improve the quality and consistency of your clinical records
-
Support better communication across providers
-
Strengthen claims for medical necessity
-
Protect your practice in audits or legal proceedings
With ICANotes, clinicians can generate rich narrative psychiatric progress notes in just minutes using a menu-driven system that aligns with best practices and documentation standards for psychiatry. You get structured prompts, clinically sound templates, and instant population of essential content—all with very little manual entry.
Video Demo: How to Write a Medication Management Progress Note in 2 Minutes
What to Include in a High-Quality Psychiatric Progress Note
To write effective psychiatric notes, it’s important to include all of the elements typically required for clinical care, insurance billing, and legal documentation. Below is a breakdown of the essential components of a comprehensive psychiatric progress note and how ICANotes helps streamline each one.
1. Current Situation / Reason for Visit
Describe how the patient’s symptoms have changed since the last visit. Has there been improvement, worsening, or no change? This section should reflect both the patient’s self-report and your clinical observations.
Detail the patient’s current status and why they are being seen today. This might include new symptoms, stressors, life events, or a follow-up on prior issues.
With ICANotes, structured prompts guide you through documenting the presenting problem, making it easy to update changes from prior sessions and highlight clinical priorities.
2. Relevant History
Include pertinent psychiatric, medical, family, and social history relevant to today’s session. This contextualizes the patient’s current functioning and guides treatment planning.
In ICANotes, prior history is easily viewable and can be pulled forward or referenced, reducing the need to retype clinical background repeatedly.
3. Verbal Content
Summarize the focus of the session from the patient’s perspective. What did they share? What concerns were discussed?
ICANotes lets you choose from structured options based on common therapeutic themes or customize narrative text to capture the unique details of each session, eliminating the need to start from scratch every time.
4. Therapeutic Interventions
Detail the specific therapeutic techniques you used during the session. This might include CBT strategies, psychoeducation, medication adjustments, or supportive listening.
ICANotes includes a comprehensive library of evidence-based interventions that can be easily inserted and customized, ensuring your psychiatry notes accurately reflect your clinical efforts.
5. Patient's Response to Interventions
Note how the patient responded to the therapeutic approaches used. Did they engage? Show insight? Resist the process?
You can quickly document engagement level and session dynamics with ICANotes' selectable phrases that reflect a range of client responses.
6. Mental Status Examination
Document your objective assessment of the patient's appearance, behavior, mood, affect, thought processes, insight, and other key mental health indicators. The MSE is a critical component in identifying psychiatric changes and informing diagnosis.
ICANotes features a structured Mental Status Exam builder, enabling you to create a complete and compliant MSE in under a minute, with checkboxes and dropdowns that auto-populate your note with clinically accurate language.
7. Medications
List all current psychiatric and medical medications, including dosage, frequency, and any adherence issues, side effects, or recent changes.
ICANotes allows you to track medications across encounters, adjust prescriptions, and document medication education or compliance in just a few clicks.
8. Diagnoses
Include the patient’s current DSM-5 or ICD diagnosis. Update it as necessary, especially if new symptoms emerge or conditions resolve.
ICANotes integrates searchable diagnostic codes and offers the ability to update diagnoses seamlessly, with justifications if needed.
9. Risk Assessment
Evaluate suicide risk, homicidal ideation, self-harm behaviors, or danger to others. Include the specific questions asked, risk factors identified, protective factors, and your clinical judgment about current risk level.
ICANotes provides a structured risk assessment module that helps ensure no critical safety question is missed and that documentation aligns with best practices and legal standards.
10. Instructions, Recommendations, and Plan
Outline the next steps in treatment, including follow-up appointments, referrals, medication changes, or homework assignments. Include measurable short-term goals and timelines when appropriate.
With ICANotes, you can document your treatment plan in alignment with insurance requirements and medical necessity standards. Progress toward goals can be easily tracked across sessions, and updates to the plan are quick to apply.
Download Our Guide to Writing Better, Faster Clinical Notes
Streamline your progress notes, avoid documentation pitfalls, and stay compliant with practical templates, note formats (SOAP, DAP, BIRP), and time-saving tips to write high-quality, defensible notes faster.
How ICANotes Makes Psychiatric Note Writing Fast, Accurate, and Compliant
Whether you're managing 10 clients or 100, ICANotes reduces your documentation time while improving the quality of your psychiatric progress notes. Here’s how:
✅ Menu-Driven Interface: Build rich, narrative notes without typing full sentences
✅ Pre-Configured Templates: Designed for psychiatry, including MSEs, med management, and therapy notes
✅ Compliant Documentation: Structured to meet payer, audit, and legal requirements
✅ Time-Saving Workflows: Notes can be completed in under 5 minutes
✅ Cloud-Based Access: Securely access and update notes from anywhere
Write Better Psychiatric Progress Notes in Less Time
Whether you're working in private practice or a larger clinic setting, ICANotes empowers you to spend less time on paperwork and more time on patient care. Our system helps psychiatrists and psychiatric nurse practitioners create high-quality, defensible, and efficient psychiatric progress notes—without the burnout.
Explore how ICANotes can transform your workflow by starting a free trial or by calling us at 443-357-0990.
Schedule a Live Demo
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals—built to streamline documentation, improve compliance, and enhance patient care.
Simplify clinical charting
Stay organized with appointment scheduling
Reduce no-shows with automated reminders
Improve client engagement with a secure patient portal
Provide flexible care with HIPAA-compliant telehealth
Dr. October Boyles is a distinguished healthcare professional with extensive expertise in behavioral health, clinical leadership, and evidence-based care delivery. With a Doctor of Nursing Practice (DNP) from Aspen University and advanced degrees in nursing, she brings a depth of clinical knowledge and a passion for improving mental health care services.