Blog > Documentation > How to Write a Biopsychosocial Assessment
How to Write a Biopsychosocial Assessment
This concise yet comprehensive guide demystifies the biopsychosocial assessment by breaking down how to seamlessly integrate biological, psychological, and social factors into your initial evaluation, equipping you with targeted questions and clear report-writing strategies. You’ll walk away with a structured outline, best‑practice tips, and ready‑to‑use tools that not only enhance clinical insight but also streamline documentation—making it a must-read for practitioners committed to holistic, efficient client care.

Last Updated: June 12, 2025

What You'll Learn
-
Practical steps to structure a comprehensive biopsychosocial assessment, integrating biological, psychological, and social dimensions.
-
Sample questions and prompts tailored to effectively capture detailed client histories.
-
Common pitfalls to avoid, helping ensure accuracy and completeness in your assessment reports.
-
Time-saving tips and structured templates to streamline documentation, enhance clinical insights, and support effective treatment planning.
Contents
Understanding the Biopsychosocial Model of Mental Health
What is Included in a Biopsychosocial Assessment?
How to Write a Biopsychosocial Assessment as a Mental Health Professional
Tips to Remember When Writing a Biopsychosocial Assessment
Using Technology to Reduce Your Documentation Burden
Why Use ICANotes for Your Biopsychosocial Assessments?
Biopsychosocial assessments help health professionals assess what biological, psychological and social factors could be impacting their client's health. This comprehensive assessment creates a foundation for understanding the factors contributing to your patient's well-being and enables clinicians to develop an effective treatment plan.
Mental health professionals typically conduct a biopsychosocial assessment as part of the initial assessment with clients. We've created this guide to help you learn how to use biopsychosocial assessment questions and write a report.
Understanding the Biopsychosocial Model of Mental Health
Biopsychosocial assessments are based on the biopsychosocial model proposed by Dr. George Engel. According to Engel's model, a person's body and mind are not separate entities. In other words, a person's biological, social and psychological states all intertwine and impact their well-being.
For example, if a patient experiences a physical illness while lacking social support, they may become depressed or anxious. Similarly, if a person has depression, they might withdraw from their friends and family and neglect self-care, impacting their physical and social wellness.
Is a Biopsychosocial Assessment Necessary?
The biopsychosocial assessment is often necessary when psychological factors alone do not explain the presence of a mental health condition. Psychological factors do not consider the many social and biological factors that can impact one's mental state.
Mental health professionals recognize the need to view clients holistically and consider how various aspects of a person's life might contribute to a mental health issue, impair functioning or maintain a disorder.
Streamline your Intakes with this powerful form!
Download our Fillable Biopsychosocial Intake Form
Whether you're onboarding new clients or updating charts, this form helps you gather everything you need in one place.
What is Included in a Biopsychosocial Assessment?
Biological Factors
Psychological Factors
Social Factors
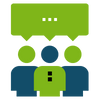
As you can tell by its name, the biopsychosocial model includes three components: biological, psychological and social factors. You'll want to focus on these aspects as you gather data for your assessment via patient questionnaires and face-to-face interviews. To show you what to cover, here are descriptions of each component:
1. Biological Factors
Biological factors refer to aspects of an individual's physical makeup, such as genes, physiology, hormones, neurotransmitters, chemistry, brain structures and organ system functioning. Many mental conditions are caused by a combination of biological, psychological, genetic and environmental factors.
Since genes can play a part in a person's mental health and increase the risk of developing certain disorders, counselors should consider a client's family history during their initial meeting.
You might take the following information about your client into account:
- Genes
- Age
- Immune Response
- Infections
- Environmental toxins
- Physical traumas
- Diet
- Appetite
- Hormones
- Sleep/exercise habits
Biological questions help you understand a client's medical issues and history, which can impact other areas of their life. Consider asking your client to fill out a questionnaire about their personal medical and mental health history, their family's medical and mental health history, their substance use history, and their current sleep, diet and exercise habits.
You might ask questions such as:
- Who is your current primary care physician?
- Are you on medications? If so, what are they?
- Are you allergic to any medications?
- Do you have a personal or family history of substance abuse or mental health disorders?
- Are you experiencing any medical problems that are impacting your life?
- What medical or surgical issues have you had in the past?
2. Psychological Factors
Psychological factors refer to a person's thought processes and how they influence mental states and behavior. Psychological factors can impact a person's physical well-being and vice versa.
For example, one study found that at least 36% of patients with chronic pain experienced depressive symptoms. Chronic pain and depression are correlated — as the pain worsens, so does the risk, duration and severity of depression. According to the American Psychological Association, more than 55% of adults who live with chronic pain also have symptoms of anxiety and depression.
To understand your clients better, consider psychological factors and related information, such as:
- Personality
- Psychological traumas
- Stress
- Coping skills
- Suicidal ideation
- Reaction to illness
The psychological component of the biopsychosocial assessment offers a more accurate look at a patient's thoughts, behaviors and feelings. To identify psychological factors that may be influencing your client's health, you can give them a questionnaire containing a current symptom checklist and a checklist of emotional and behavioral issues.
You might also ask the following questions:
- What brings you in today?
- How long have you been experiencing this problem?
- How would you describe yourself?
- What are your strengths and weaknesses?
- Have you had counseling in the past?
- Have you had suicidal or homicidal thoughts?
- What do you feel is your greatest need right now?
- What do you hope to gain from therapy?
3. Social Factors
Social factors include relationships, culture, money, family, work and housing. Research shows that social determinants, such as education and socioeconomic status, can significantly impact mental health. For example, higher income levels often correlate with positive mental health due to access to effective health care, sufficient food security and safe housing. Alternatively, income volatility, debt and perceived job security can have a substantial impact on mental health.
To learn about a client's social circumstances and how these factors influence their mental and physical health, you might focus on the following:
- Family relationships
- Social support
- Marital status
- Cultural influences
- Food security
- Income level
- Discrimination
- Living situation
- Military service
- Spiritual or religious background
- Hobbies and recreational activities
- Sexual history
- Financial status
- Legal history
- Educational background
- Employment status and work history
- Access to affordable healthcare
Ask questions that help you understand your client's past and current relationships, work-related stressors, finances and involvement in their community. You might ask:
- Are you involved with any community organizations?Who is in your family?
- Who do you live with, and who do you see most often?
- Are there any problems in your family now, or were there issues in the past?
- How much support do you expect from family members?
- Do you have close friends?
- Are there any issues with your friendships?
- Who can you rely on for support?
- Have you ever been arrested?
- Were you ever sentenced for a crime?
- What kind of work do you currently do?
- What have you done in the past?
- How much work-related stress is in your life?
- Have you ever served in the military?
How to Write a Biopsychosocial Assessment as a Mental Health Professional
After you've gathered data about your client, you can write a biopsychosocial assessment report. Your report will help you understand your client as a whole individual to devise an effective treatment plan. You can also share your assessment with colleagues or physicians to coordinate care.
Here's a biopsychosocial assessment outline to help you get started.
Basic Information
Begin your report with basic information about your client. This should include:
- Identifying information: Include identifying information such as your client's name, gender, date of birth and marital status.
- Referral: Provide the name of the person or agency who referred the client to you. Include the type of assistance they sought.
- Presenting problem: Describe the reason the client came to you. Include the client's definition of their problem, how long they've been experiencing the issue and what they expect to gain from your services. Also, describe what the client has done in the past to try to resolve the issue.
- Source of data: List everything you used to gather data for your reports, such as questionnaires, interviews, observations, test results and records from the referring agency. Describe your client's involvement in compiling the information.
- General description of the client: Briefly describe your client's appearance, mood and level of cooperation during the interview. List any problems the client has with memory, thinking or speech. Note any signs of anxiety, depression or other mental health issues.
Client's History and Current Functioning
Examine the client's history and current functioning and include relevant details. Address the following areas when writing your report:
- Family history: Describe the client's family members, including details about the client's childhood relationships and who they grew up with. List family members' history of substance abuse, legal problems or psychiatric disorders.
- Educational background: Write about your client's educational experience, challenges they may have faced and current goals.
- Employment status and history: Include your client's current employment status and occupation, an overview of their work history and any special skills or training they have.
- Religious or spiritual beliefs and practices: Mention if your client identifies with a religion or spiritual beliefs. Include any involvement they may have with a religious community.
- Military service and history: Mention if your client was or wasn't in the military. If they served in the military, describe their role, the dates they served, any highly stressful experiences they had and the type of discharge they received.
- Current and past medical background: Describe your client's current general health and functioning. Mention any history of disease, accidents and medication. Consider their family's medical history.
- Mental health history: Describe your client's mental health history, including current or previous experiences of abuse, violence, trauma or neglect.
- History of substance abuse: If your client has a substance abuse background, list all current and past experiences with drugs or alcohol. Include any medical treatment or rehabilitation they received.
- Social and recreational activities: Describe your client's social network, including significant relationships. Mention if your client is involved in the community or has hobbies.
- Basic life functioning: Add your client's current functioning level and if they can meet their basic life needs, such as obtaining housing and food. Write if they require assistance.
- Present legal concerns or past issues: Include any legal concerns your client has or dealt with in the past, including marital issues or domestic violence.
- Client's strengths and resources: Evaluate how your client copes with issues. Mention their strengths and limitations.
- Other environmental or psychosocial assessment factors: Describe other factors that may influence your client's mental health, such as discrimination or sexuality issues.

Your Assessment and Recommendations
After you provide an overview of your client's current and past psychological, biological and social states, it's time to include your professional assessment. You might offer the following information:
- Brief summary: In about three to five sentences, summarize what you've already written in your report, including your client's primary problem and any associated factors. Describe your client's level of urgency regarding the problem. Mention any secondary issues or concerns your client shared.
- Client's appearance: Describe how your client appeared during the interview, including signs of anxiety or depression and any memory or speech issues. If you also conducted a mental status exam during your initial meeting with a client, include it in this section.
- Your observations: Provide your observations of the client and their current state. Discuss your assessment of the client's motivation to use your service and modify behaviors.
- Diagnosis: Include your diagnosis and any diagnoses your client claimed they'd been given in the past by other therapists.
- Goals and recommendations: Identify long-term and short-term goals. Describe the type of treatment you think is best for your client and any suggestions for services and resources. Include how long you think your client should receive treatment.
Tips to Remember When Writing a Biopsychosocial Assessment
As you write your biopsychosocial assessment report, it's important to consider who will use your assessment to provide care. Here are tips to help communicate your assessment with colleagues and other care providers:
1. Differentiate Between Objective Facts and Subjective Impressions
Make sure to frame information in a way that separates facts from your impressions. Objective facts include things the client actually said, whereas subjective impressions include how the client appeared to you. Be sure to clarify who said, thought or did something in your report.
For example, to have an objective fact, you might write, "The client said he felt sad when he lost his mother." To state a subjective impression, you might write, "The client seemed sad when he talked about his mother." You'll want to be as objective and unbiased as possible.
2. Create a Balance of Information
Be sure to include a balance of information to ensure your evaluation is accurate and effective. Note the client's strengths, challenges, facts and impressions.
3. Present Information Based on Priority
Decide which problems are most important and need urgent attention. Spend more time writing about these issues in your report. You'll also want to present the primary issues first.
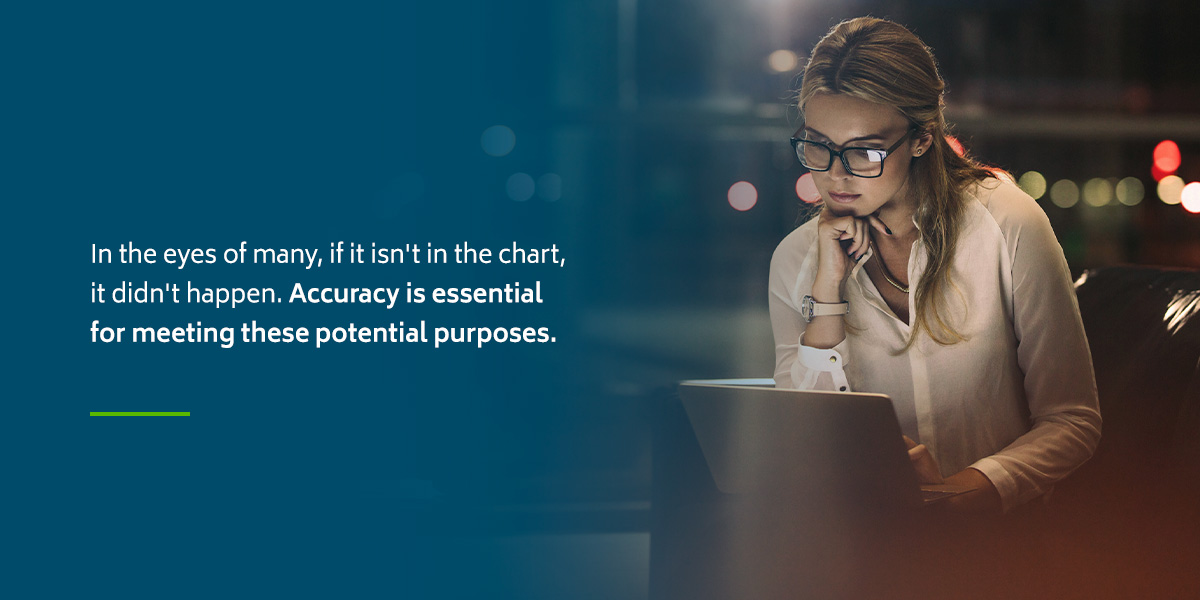
4. Consider Accuracy
Other physicians or therapists may read your report, so it's crucial to be as accurate as possible. Ensure you accurately convey what the client or other sources said or did, and remove or rewrite errors or misleading information.
5. Remove Irrelevant Details
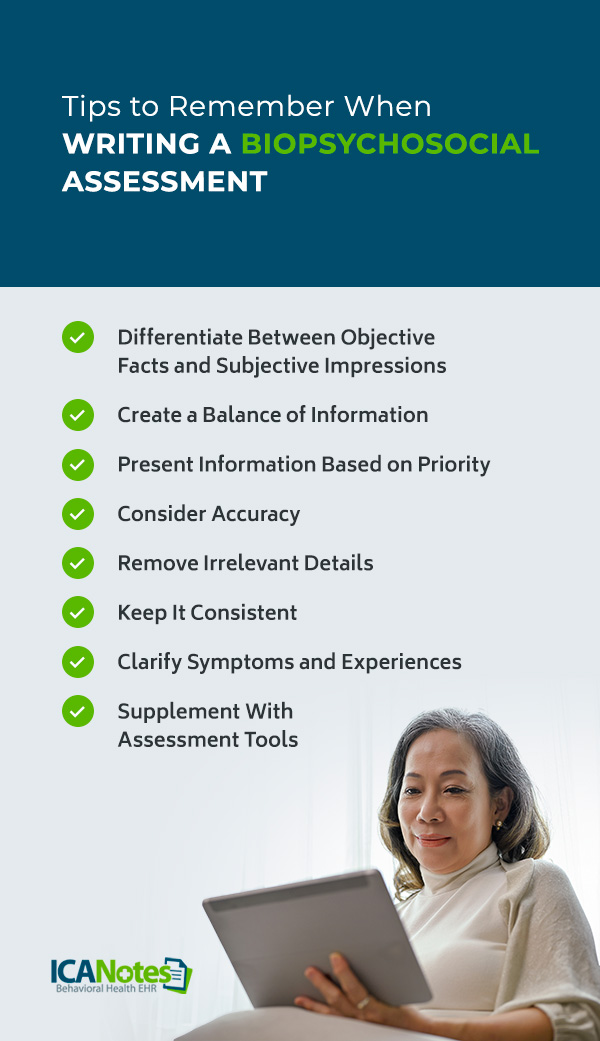
You do not need to include everything the client said, thought, felt or did in your report. Instead, aim to include only relevant information.
It's also possible that your biopsychosocial assessment may not yield relevant information in all three factors. For instance, you may find that a patient's depression is associated with their living situation — a social factor — but cannot identify a biological factor that may contribute to their depression.
You do not need to include everything the client said, thought, felt or did in your report. Instead, aim to include only relevant information.
It's also possible that your biopsychosocial assessment may not yield relevant information in all three factors. For instance, you may find that a patient's depression is associated with their living situation — a social factor — but cannot identify a biological factor that may contribute to their depression.
6. Keep It Consistent
All documentation should be organized in a logical manner that's easy to comprehend. For example, if your evaluation includes a diagnosis of major depressive disorder, your report should include detailed mentions of the client's loss of interest in pleasurable activities, sleep disturbances or appetite changes.
7. Clarify Symptoms and Experiences
While you do not have to ask every question outlined in a biopsychosocial assessment, you can ask relevant follow-up questions.
For example, if a client responds to the question "How much work-related stress is in your life?" with "I am extremely overwhelmed with work-related stress," you can ask follow-up questions about the intensity, frequency and onset of their experiences.
8. Supplement with Assessment Tools
You can use the following assessment tools and templates to make your evaluation more efficient and support your official diagnosis:
- Patient Health Questionnaire (PHQ-9)
- Kessler Psychological Distress Scale (K10)
- Patient Stress Questionnaire
- My Mood Monitor
- Mood Disorder Questionnaire (MDQ)
- Generalized Anxiety Disorder seven-item (GAD-7) scale
- Hamilton Anxiety Rating Scale (HAM-A)
- Life Events Checklist for DSM-5 (LEC-5)
Using Technology to Reduce Your Documentation Burden
Writing a biopsychosocial assessment is just part of your documentation workload as a behavioral health professional. In addition to evaluations, you likely have progress notes, psychotherapy notes, treatment plans, medical records, privacy notices, and consent forms to complete, organize and keep secure. Although these documents enable you to treat clients and provide the best care possible, they can also be time-consuming if you don't use document management tools.
If you need assistance managing documentation in your practice, ICANotes electronic health record (EHR) software for behavioral health can reduce the amount of time you spend writing, organizing and searching for critical documents. ICANotes was designed by a clinical psychiatrist for behavioral health professionals and is a comprehensive EHR system. With ICANotes, you can:
- Scan forms or questionnaires to keep digital files.
- Quickly and securely access clients' records from your phone, tablet or laptop.
- Keep all records, forms and notes organized and compliant with privacy laws.
- Take advantage of customizable templates and automatic data population to reduce documentation time.
- Ensure accurate, legible notes to enable better care coordination and faster reimbursement.
- Keep clients engaged and satisfied with the convenient patient portal.
Overall, ICANotes can help you run an efficient practice and allow you to focus more time on your clients.
Why Use ICANotes for Your Biopsychosocial Assessments?
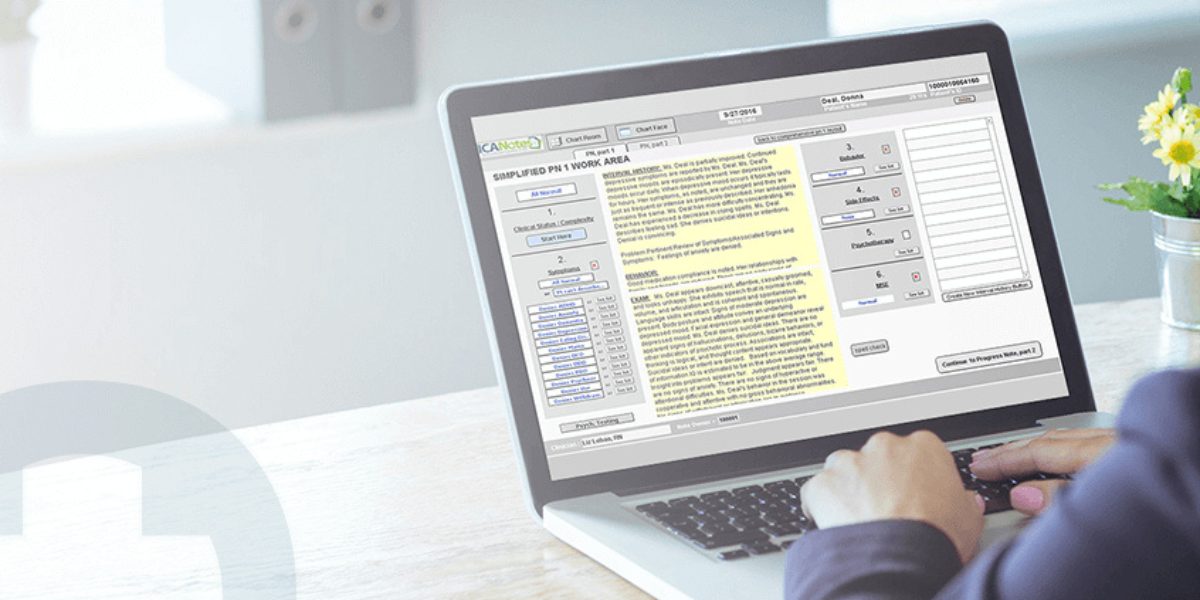
ICANotes simplifies biopsychosocial assessments by allowing clients to securely complete their intake information through a mobile-friendly electronic history module—accessible from any device. This client-entered data seamlessly integrates directly into the clinician's biopsychosocial assessment document, significantly reducing redundant data entry and streamlining your review and documentation processes.
With ICANotes’ intuitive, menu-driven interface and pre-configured templates, you can quickly generate comprehensive, narrative-rich biopsychosocial assessments. Additionally, built-in electronic rating scales (like PHQ-9, GAD-7, ASI, and more) help you capture standardized data directly within your clinical workflow, enhancing both accuracy and regulatory compliance.
By leveraging ICANotes, clinicians spend less time on documentation and more time providing quality care. Register for a fully functional 30 day trial (no credit card required!) or book a demo to learn more.
Schedule a Live Demo
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals—built to streamline documentation, improve compliance, and enhance patient care.
Simplify clinical charting
Stay organized with appointment scheduling
Reduce no-shows with automated reminders
Improve client engagement with a secure patient portal
Provide flexible care with HIPAA-compliant telehealth
Frequently Asked Questions
Dr. October Boyles is a behavioral health expert and clinical leader with extensive expertise in nursing, compliance, and healthcare operations. With a Doctor of Nursing Practice (DNP) from Aspen University and advanced degrees in nursing, she specializes in evidence-based practices, EHR optimization, and improving outcomes in behavioral health settings. Dr. Boyles is passionate about empowering clinicians with the tools and strategies needed to deliver high-quality, patient-centered care.