Blog > Documentation > Therapist Notes: Complete Guide to Documentation Types & Best Practices
Therapist Notes: Complete Guide to Documentation Types & Best Practices
This definitive guide to therapist notes addresses one of the biggest challenges mental health professionals face: creating efficient, compliant, and clinically useful documentation. Whether you’re struggling with time-consuming paperwork, unsure about the differences between note formats, or concerned about HIPAA compliance, this article provides practical solutions. We explore the major documentation types — SOAP, DAP, BIRP, progress notes, and psychotherapy notes — with real-world examples that show exactly how to implement each format. You’ll also discover strategies to reduce documentation time, avoid common mistakes, and ensure your notes meet legal and ethical standards. This guide equips you with the knowledge and tools to implement efficient documentation workflows.

Donald Morrison, MSW, LCSW
Last Updated: September 4, 2025


What You'll Learn
- Documentation Formats: Master the structure and appropriate use of SOAP, DAP, BIRP, progress notes, and psychotherapy notes with real examples
- HIPAA Compliance: Understand the specific requirements for protecting therapist notes and the critical differences between progress notes and psychotherapy notes
- Legal Protections: Learn how proper documentation safeguards your practice during audits, legal proceedings, and insurance reviews
- Real-World Examples: See fully-written sample notes demonstrating best practices for different clinical scenarios
- Ethical Considerations: Navigate complex issues around record requests, documentation retention, and information disclosure
Contents
- Types of Therapy Notes
- Progress Notes for Therapists
- Psychotherapy Notes vs Progress Notes
- HIPAA Compliance for Therapy Notes
- Common Therapy Documentation Mistakes
- Efficiency Strategies for Writing Therapist Notes
- Real-World Examples of Therapist Notes
- Legal and Ethical Considerations
- Final Thoughts on Therapist Notes
Introduction to Therapist Notes
Effective therapist notes are essential for providing quality care and maintaining accurate records. Whether you’re a seasoned clinician or new to the field, the documentation process can be both challenging and time-consuming. Many mental health professionals struggle with creating therapist notes that are both efficient and thorough.
Documentation serves multiple critical purposes: it tracks client progress, ensures continuity of care, meets legal and ethical requirements, supports insurance reimbursement, and protects you in case of audits or legal issues. Learning how to write comprehensive therapist notes can improve your clinical practice and ensure legal compliance.
In this guide, we’ll explore the different types of therapy notes, provide real-world examples, discuss HIPAA compliance requirements, address common documentation mistakes, and share efficiency strategies to help you create better clinical documentation while spending less time on paperwork.
Download Our Guide to Writing Better, Faster Clinical Notes
Streamline your progress notes, avoid documentation pitfalls, and stay compliant with practical templates, note formats (SOAP, DAP, BIRP), and time-saving tips to write high-quality, defensible notes faster.
Types of Therapy Notes
Understanding the various types of therapy notes and when to use each format is fundamental to effective clinical documentation. Each format has specific advantages depending on your practice setting, client population, and documentation needs.
SOAP Notes for Therapists
SOAP notes for therapists provide a structured format that includes Subjective, Objective, Assessment, and Plan sections. This widely-used format helps organize clinical information in a logical sequence.
- S - Subjective
This section documents the client’s self-reported experiences, symptoms, and concerns. Include direct quotes when possible and note any changes since the previous session.
- O - Objective
Record observable data and facts without interpretation. This includes your observations of the client’s appearance, behavior, mood, affect, and any assessment results or measurements.
- A - Assessment
Document your clinical impressions, diagnosis considerations, and professional analysis of the client’s presentation. Connect your observations to diagnostic criteria and treatment goals.
- P - Plan
Detail the treatment plan, including interventions used, homework assigned, referrals made, and plans for the next session. Include any adjustments to the treatment approach.
When creating SOAP notes for therapists, it’s important to include relevant client statements in the Subjective section while keeping the Objective section focused on observable facts. Many electronic health record systems include templates for SOAP notes for therapists to streamline the documentation process.
DAP Notes Mental Health
The DAP note format for mental health documentation follows a Data, Assessment, and Plan structure that many clinicians find intuitive. This format is often preferred for its simplicity and efficiency.
- D - Data
Combine both subjective and objective information in this section. Include what the client reports and what you observe during the session. When writing DAP notes mental health professionals should focus on observable behaviors in the Data section.
- A - Assessment
Document your clinical reasoning, interpretation of the data, and progress toward treatment goals. The assessment section of DAP notes mental health documentation should include your clinical impressions and reasoning.
- P - Plan
Outline the next steps in treatment, including interventions, homework, referrals, and the focus for future sessions.
DAP notes are particularly useful for clinicians who prefer a more streamlined approach than SOAP notes while still maintaining a clear structure. They work well in settings where detailed separation of subjective and objective data isn’t necessary.
BIRP Notes Format and Example
BIRP notes focus on Behavior, Intervention, Response, and Plan, making them particularly useful for tracking specific interventions and client responses.
- B - Behavior
Document the client’s behaviors, including verbal statements, emotional expressions, and actions during the session.
- I - Intervention
Record the specific therapeutic techniques, approaches, and interventions you used during the session.
- R - Response
Note how the client responded to your interventions, including any changes in behavior, insight gained, or resistance encountered.
- P - Plan
Detail the plan for future sessions, including treatment goals, homework assignments, and any adjustments to the treatment approach.
Below you’ll find a BIRP notes example that demonstrates proper documentation of Behavior, Intervention, Response, and Plan. This BIRP notes example shows how to document client behaviors objectively while maintaining clinical relevance. Reviewing a well-written BIRP notes example can help you improve your own documentation practices.

BIRP Notes Example
Behavior: Client arrived 5 minutes late, appearing anxious with rapid speech and fidgeting. Reported feeling "overwhelmed" by work demands and described conflict with supervisor. Stated, "I can't sleep because my mind won't shut off."
Intervention: Used guided breathing exercise to reduce immediate anxiety. Implemented cognitive restructuring to identify and challenge catastrophic thinking patterns about work performance. Explored boundary-setting strategies for workplace interactions.
Response: Client's breathing slowed and fidgeting decreased following relaxation exercise. Initially resistant to challenging negative thoughts ("But my boss really does hate me"), but gradually identified evidence that contradicted this belief. Expressed interest in practicing boundary-setting techniques.
Plan: Continue cognitive restructuring work focusing on workplace scenarios. Assign thought record homework to track anxious thoughts. Provide sleep hygiene handout. Next appointment scheduled for 10/12/2023.
Progress Notes for Therapists
Progress notes for therapists document client progress toward treatment goals and are essential for insurance reimbursement and continuity of care. Well-written progress notes for therapists document client progress toward treatment goals while justifying the need for continued treatment.
Effective progress notes should:
- Connect session content to treatment plan goals
- Document interventions used and their effectiveness
- Note changes in symptoms, functioning, or risk factors
- Include plans for future sessions
Insurance companies often require detailed progress notes for therapists to justify continued treatment. Creating concise yet comprehensive progress notes for therapists is a skill that develops with practice.
Many clinicians use a combination of formats (like SOAP or DAP) within their progress notes to ensure they capture all necessary elements while maintaining efficiency.
Psychotherapy Notes vs Progress Notes
Understanding the distinction between psychotherapy notes vs progress notes is crucial for HIPAA compliance and proper record-keeping. The key difference in psychotherapy notes vs progress notes lies in their legal status and level of protection.
Progress Notes:
- Part of the official medical record
- May be requested by clients, insurance companies, or legal entities
- Document services provided, assessment, diagnosis, treatment plan, and client progress
- Must be maintained according to legal and ethical standards
Psychotherapy Notes:
- Private notes of the therapist
- Contain the therapist’s impressions, hypotheses, and analysis
- Receive special protection under HIPAA
- Not typically disclosed to clients or third parties
- Often include details the therapist is processing but that aren’t necessary for treatment
While progress notes are part of the medical record, psychotherapy notes vs progress notes shows that the former receives special protection under HIPAA. Keeping these separate helps maintain appropriate boundaries and protections.
Understanding the difference between psychotherapy notes and progress notes helps clarify what belongs in the official record versus what remains private. The table below highlights the key distinctions.
| Category | Progress Notes | Psychotherapy Notes |
|---|---|---|
| Purpose | Document services provided, client progress, and link to treatment plan. | Capture therapist’s personal reflections, impressions, and analysis. |
| Status | Part of the official medical record. | Kept separate from the medical record. |
| Access | May be requested by clients, insurers, or legal entities. | Protected under HIPAA; not typically shared with clients or third parties. |
| Content | Includes symptoms, interventions, assessment, and treatment progress. | May include ideas, hypotheses, or details the therapist is processing privately. |
HIPAA Compliance for Therapy Notes
Creating HIPAA compliant therapy notes requires understanding both technical and administrative safeguards. Proper documentation practices are essential for protecting client confidentiality and avoiding costly violations.
Protected Health Information in Notes
When creating therapy notes, be mindful of what constitutes Protected Health Information (PHI):
- Client identifiers (name, contact information, date of birth)
- Diagnosis and treatment information
- Session dates and billing information
- Any information that could identify the client
HIPAA compliant therapy notes should contain only the minimum necessary information required for treatment, payment, and healthcare operations. Avoid including extraneous details that aren’t clinically relevant.
Digital Storage Requirements
Electronic systems can help ensure your practice maintains HIPAA compliant therapy notes. Key requirements include:
- Encryption: All electronic notes must be encrypted both in storage and during transmission
- Access Controls: Implement user authentication and role-based access
- Audit Trails: Maintain logs of who accessed records and when
- Backup Systems: Regular, secure backups to prevent data loss
- Business Associate Agreements: Required for any third-party services handling PHI
Documentation Retention Policies
HIPAA compliant therapy notes must be retained according to state laws and professional guidelines, typically 7-10 years for adult clients and longer for minors. Develop clear policies for:
- Minimum retention periods based on your state’s requirements
- Secure destruction methods when retention periods expire
- Documentation of destruction processes
- Special considerations for minor clients
Regular audits of your documentation can help verify you’re maintaining HIPAA compliant therapy notes and identify any areas needing improvement.
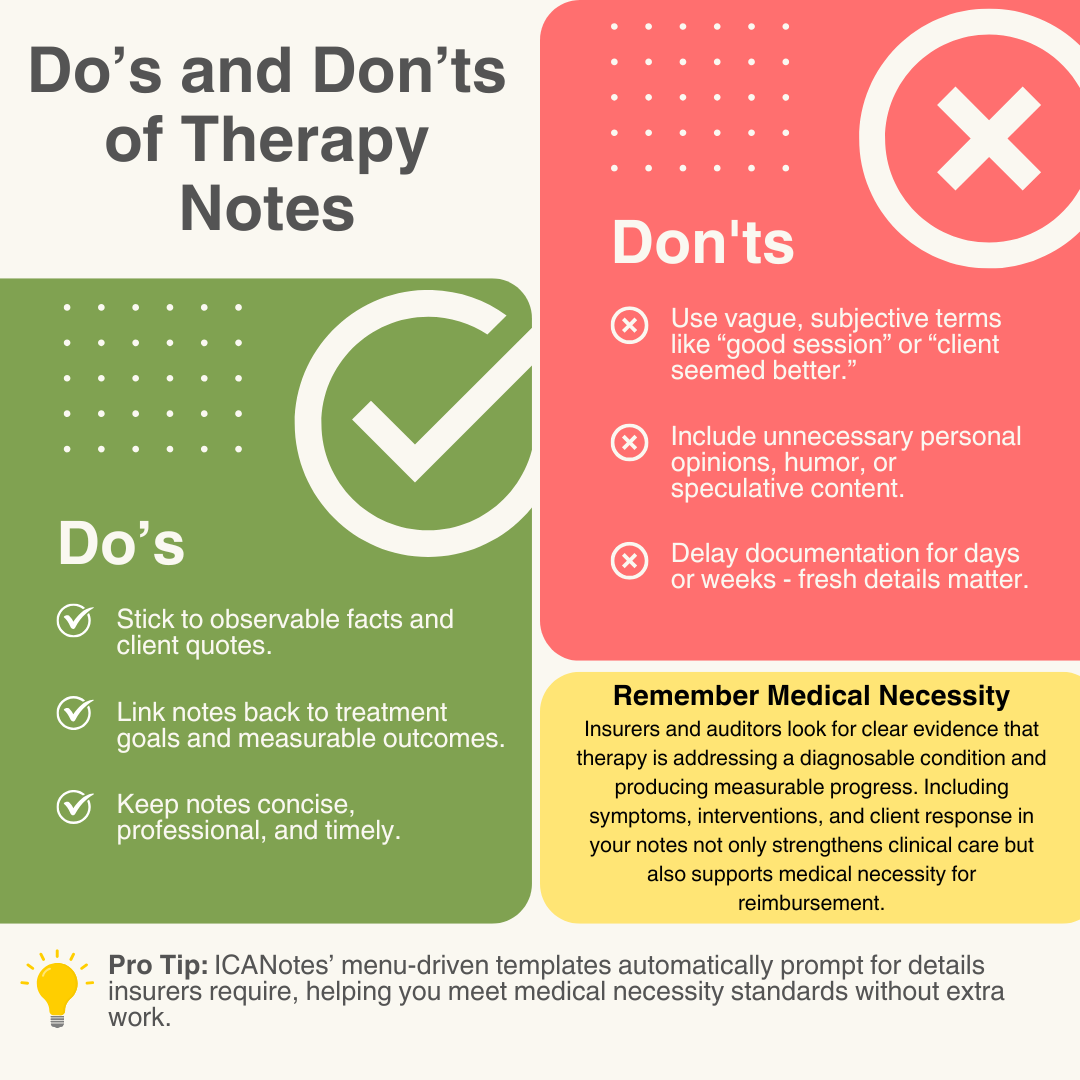
Common Therapy Documentation Mistakes
Even experienced clinicians make documentation errors. Being aware of these common pitfalls can help you avoid them.
| Mistake | Problem (what this looks like) | Solution (what to do instead) |
|---|---|---|
| Vague or Subjective Language | Using terms like “good session,” “client seemed better,” or “therapy going well” without specific details. | Document observable behaviors, specific statements, and measurable changes. Instead of “client seemed anxious,” write: “Client displayed rapid speech, fidgeting, and reported racing thoughts.” |
| Missing Connection to Treatment Plan | Failing to connect session content to established treatment goals. | For each session, explicitly reference how discussion and interventions relate to specific treatment goals. For example: “Continued exposure exercises for social anxiety (Goal 2); client reported 30% reduction in anxiety compared to previous exposure.” |
| Inconsistent Documentation | Varying detail levels, formats, or terminology across sessions. | Use consistent templates and formats. Establish personal documentation standards and stick to them. Using therapy note templates can significantly reduce documentation time while ensuring thoroughness. |
| Delayed Documentation | Waiting days or weeks to complete notes, leading to forgotten details. | Complete notes immediately after sessions when possible. If not, use brief voice memos or bullet points to capture key information for later expansion. |
| Inappropriate Content | Including non-essential judgmental statements or speculative content. | Focus on facts and clinical observations. If including interpretations, clearly label them as such and connect them to clinical reasoning. |
Efficiency Strategies for Writing Therapist Notes
Documentation doesn’t have to consume hours of your day. Use these practical strategies to keep notes accurate, compliant, and efficient — without over-documenting.
1. Use Templates
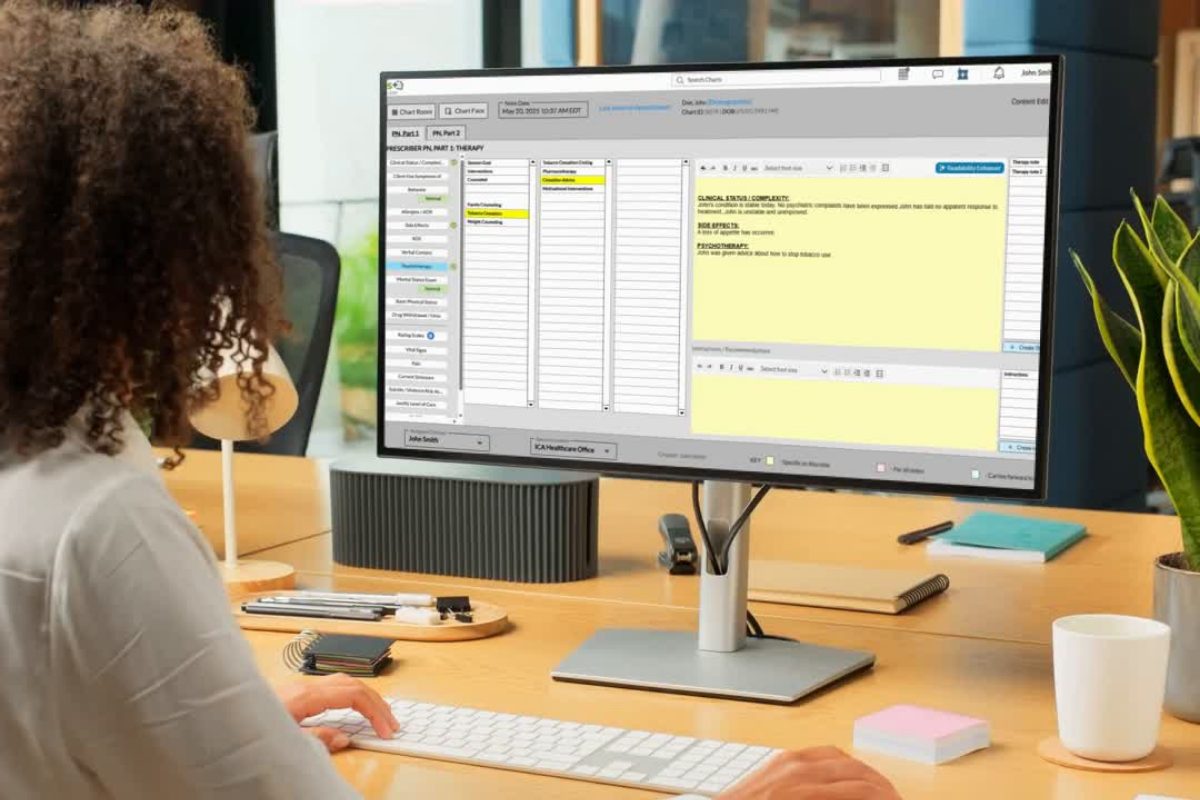
Many electronic health record systems provide customizable therapy note templates. Create or customize templates for different session types (intake, regular session, termination) and note formats (SOAP, DAP, BIRP). Effective therapy note templates include sections for symptoms, interventions, and treatment planning. A behavioral health specific EHR like ICANotes provides pre-configured menu-driven templates that guide therapists through each step of documentation, ensure consistent use of clinical language, and save significant time while still meeting compliance and payer requirements.
2. Implement Concurrent Documentation
When appropriate, complete portions of your notes during the session. This works well for:
- Reviewing previous homework
- Documenting assessment results - include brief scale scores, dates, and deltas (e.g., "PHQ-9 = 8, down from 12 on 8/01")
- Recording agreed-upon goals or homework
Always maintain clinical presence and explain to clients why you’re taking notes.
3. Focus on Clinical Relevance
Not everything discussed in a session needs to be documented. Focus on:
- Information relevant to diagnosis and treatment
- Progress toward treatment goals - reference goal IDs and note how interventions target those goals (Example: "Exposure practice for social anxiety (Goal 2); client reports ~30% reduction from last session")
- Risk factors and safety concerns
- Significant life events affecting treatment
- Interventions used and client response
4. Schedule Documentation Time
Block specific times in your schedule dedicated to completing notes. Adding 5-10 minute buffers between sessions can prevent documentation from spilling into personal time and ensures notes are completed promptly.
Real-World Examples of Therapist Notes
Seeing actual therapist note examples can make the differences between formats more concrete. Below are sample SOAP and DAP notes that illustrate how clinicians document client concerns, observations, clinical impressions, and treatment plans in structured, professional ways. These examples highlight the level of detail and organization that supports both clinical care and compliance.

SOAP Note Example
SOAP notes follow a medical-model structure, breaking down information into four categories — Subjective, Objective, Assessment, and Plan — for a detailed and systematic record of each session.
Subjective:
“Client reports feeling ‘overwhelmed and anxious’ about upcoming job interview. States sleep has been disrupted, averaging 4-5 hours per night. Reports increase in negative self-talk: ‘I’ll never get this job’ and ‘I always mess up interviews.’”
Objective:
Client arrived 5 minutes early, appropriately dressed, maintained good eye contact. Observed physical symptoms of anxiety including fidgeting, rapid speech. Completed GAD-7 with score of 12 (moderate anxiety).
Assessment:
Client experiencing situational anxiety related to upcoming job interview. Negative thought patterns and sleep disruption exacerbating anxiety symptoms. Client demonstrates insight into anxiety triggers and willingness to implement coping strategies.
Plan:
- Introduced and practiced deep breathing technique (4-7-8 method)
- Assigned thought record worksheet to identify and challenge negative thoughts
- Discussed sleep hygiene techniques
- Will continue CBT approach focusing on cognitive restructuring
- Next appointment scheduled for 10/5/2023

DAP Note Example
DAP notes provide a streamlined alternative, focusing on Data, Assessment, and Plan to capture session content efficiently while still supporting clinical reasoning and continuity of care.
Data:
Client arrived on time for session, reporting increased conflict with teenage son over past week. Described three arguments regarding homework completion and curfew. Client appeared frustrated, speaking rapidly with increased volume when discussing recent incidents. Stated, “I don’t know how to get through to him anymore.” Reports using “I” statements as practiced but feels son is “not listening.”
Assessment:
Client is implementing communication strategies but struggling with consistency and emotional regulation during conflicts. Progress toward parenting goals is slower than expected, but client remains motivated. Family dynamics appear to be shifting as son seeks more independence, requiring adjustment to parenting approach.
Plan:
- Role-played difficult conversations with focus on emotional regulation
- Reviewed and refined consequences system for homework and curfew violations
- Assigned daily 10-minute positive interaction with son
- Provided handout on adolescent development
- Next session scheduled for 10/19/2023
Whether using SOAP or DAP notes, consistent templates make it easier to capture the right details without missing critical information. A behavioral health–specific EHR like ICANotes streamlines this process with pre-configured, menu-driven templates that save time and support compliance.
Legal and Ethical Considerations
Beyond HIPAA compliance, therapist notes must adhere to various legal and ethical standards.
Subpoenas and Court Orders
Therapy records may be subpoenaed in legal proceedings. Understanding the difference between a subpoena and a court order is crucial:
- A subpoena is a request for information
- A court order is a directive from a judge
When receiving a subpoena:
- Verify its validity
- Determine what specific records are being requested
- Consider consulting with an attorney
- Obtain client consent when possible
- Provide only the minimum necessary information
State-Specific Requirements
Therapy documentation requirements vary by state and professional licensing board. Stay informed about:
- Specific content requirements
- Signature and date requirements
- Electronic record regulations
- Supervision documentation for pre-licensed professionals
Informed Consent for Documentation
Clients should understand your documentation practices as part of informed consent:
- What information you record
- How records are stored and for how long
- Who may have access to records
- Circumstances under which records may be disclosed
- Their rights regarding accessing their records
Frequently Asked Questions: Therapist Notes
Final Thoughts on Therapist Notes
Creating effective therapist notes is both an art and a science. By understanding the different documentation formats, following mental health documentation best practices, and implementing efficiency strategies, you can create notes that serve multiple purposes: clinical care, legal protection, and insurance reimbursement.
Remember that documentation is not just a bureaucratic requirement but an essential clinical tool that supports quality care. Well-crafted notes help you track client progress, plan effective interventions, and ensure continuity of care.
As you develop your documentation skills, regularly review and refine your approach. Consider periodic self-audits of your notes to identify areas for improvement. Following mental health documentation best practices protects both clients and clinicians.
With practice and the right systems in place, you can create thorough, compliant documentation while minimizing the time spent on paperwork — allowing you to focus more energy on what matters most: providing quality care to your clients.
ICANotes Simplifies Therapy Note Documentation
No matter which type of therapy note you use —SOAP, DAP, BIRP, or progress notes — ICANotes makes documentation faster, easier, and more compliant. Designed specifically for behavioral health, ICANotes offers a structured, menu-driven interface that allows clinicians to create detailed, personalized notes in just a few clicks. Notes are automatically time-stamped, formatted for audit-readiness, and integrated with the rest of the clinical record. Whether you're charting progress, recording interventions, or documenting clinical observations, ICANotes ensures your notes are thorough, professional, and support medical necessity, without the burden of excessive typing. → Learn more about our documentation solutions
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
- Complete Notes in Minutes - Purpose-built for behavioral health charting
- Always Audit-Ready – Structured documentation that meets payer requirements
- Keep Your Schedule Full – Automated reminders reduce costly no-shows
- Engage Clients Seamlessly – Secure portal for forms, messages, and payments
- HIPAA-Compliant Telehealth built into your workflow
Complete Notes in Minutes – Purpose-built for behavioral health charting
Always Audit-Ready – Structured documentation that meets payer requirements
Keep Your Schedule Full – Automated reminders reduce costly no-shows
Engage Clients Seamlessly – Secure portal for forms, messages, and payments
HIPAA-Compliant Telehealth built into your workflow
Related Posts
About the Author
Donald Morrison graduated from UNC Charlotte in 2004. He has since worked as a school-based therapist, inpatient social work supervisor and outpatient clinician. Donald currently works in private practice, and he is also an adjunct faculty member at the UNC Charlotte School of Social Work. In addition, Donald serves as a clinical supervisor to LCSW associates, and he regularly presents at area mental health conferences and seminars.