Blog > Documentation > Tips for Writing Better Mental Health SOAP Notes
Tips for Writing Better Mental Health SOAP Notes
SOAP notes are a widely used framework for organizing clinical documentation in mental health. This blog breaks down each section—Subjective, Objective, Assessment, and Plan—so you can write notes that are clear, compliant, and clinically useful. Whether you're new to SOAP notes or looking to sharpen your skills, you'll find practical tips and examples to improve your documentation process.

Last Updated: May 16, 2025


What You'll Learn
- A clear breakdown of each SOAP note section and what to include
- Practical tips for writing concise, effective mental health notes
- Common documentation mistakes and how to avoid them
- Real-world SOAP note examples for psychiatry, individual, and group therapy sessions
The mental health SOAP notes you write as a behavioral health professional describe the quality of care your patients receive. Having notes that are comprehensive yet concise, and informative yet easy for other professionals to use is a skill that often takes years to master.
Using a pre-determined framework for your patient notes can help you improve the quality of your documentation.
One of the more popular methods for creating mental health documentation is to write SOAP notes. The four-pronged approach of SOAP notes was developed using the principles of the problem-oriented medical record (POMR) pioneered by physician Lawrence Weed.
In its early days, the SOAP method was used only by medical professionals. Today, it's recognized as an effective communication tool among healthcare providers of all disciplines to document a patient's treatment.
Download our
SOAP Notes Guide
Enhance your clinical documentation skills with a comprehensive guide to writing clear, effective, and compliant SOAP notes for mental health care.
What are SOAP Notes?
SOAP Notes are a type of note framework that includes four critical elements that correspond to each letter in the acronym — Subjective, Objective, Assessment, and Plan.
These four stages offer an ideal standard for providing information necessary for all types of medical and behavioral health professionals to interact successfully with the notes.
How to Write a Mental Health SOAP Note
To write a SOAP note for mental health, include a section on each of the four elements: Subjective, Objective, Assessment, Plan.
Let's examine each category in detail and drill down on what you need to include in a SOAP note.
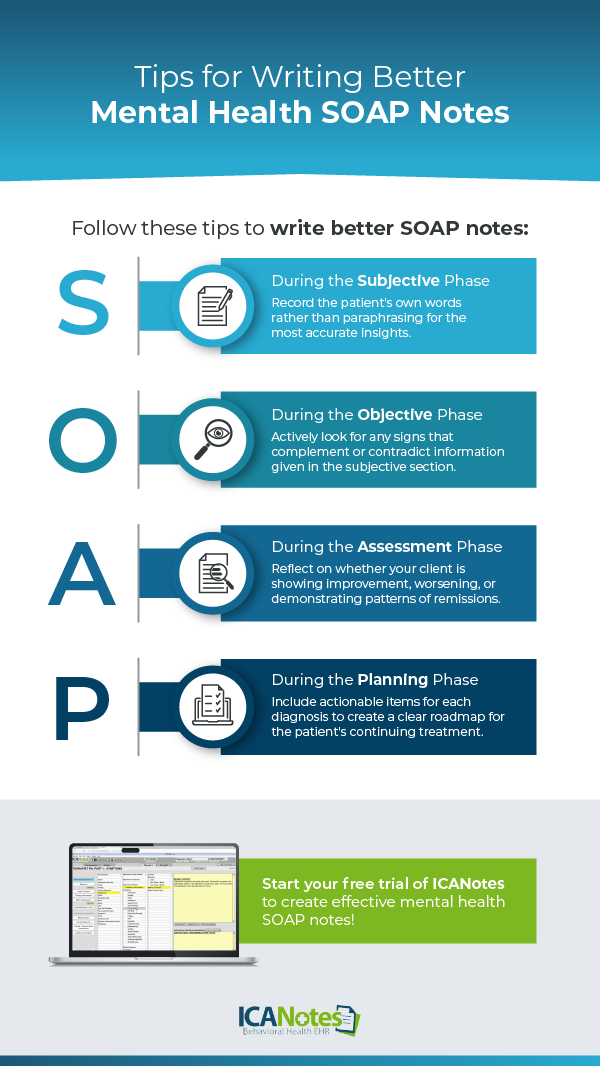
The SOAP Notes Acronym: Subjective, Objective, Assessment, Plan
1. Subjective
The first step is to gather all the information that the client has to share about their own symptoms. The patient will tell you about their experience with the symptoms and condition, as well as what they perceive to be their needs and goals for treatment.
It's crucial to record the patient's own words rather than paraphrasing them so you cultivate the most accurate insight into their condition.
The Subjective category is also an appropriate place to list any comments made by the patient, their family members, or their caretakers.
This category is the basis for the rest of your notes as well as your treatment plan, so getting the most quality information possible is paramount.
The OLD CHARTS acronym provides a smart way to cover a patient's condition systematically:
- Onset: Determine when each symptom first started.
- Location: Find out the primary location of pain or discomfort.
- Duration: Learn how long the patient has dealt with their symptoms.
- CHaracter: Examine the types of pain — aching, stabbing, etc.
- Alleviating or Aggravating Factors: What actions or interactions reduce or increase the severity of the patient's symptoms?
- Radiation: Find out if the pain radiates to other locations in the body.
- Temporal Pattern: Do the symptoms appear in a pattern like in the evenings or after meals?
- Symptoms Associated: Are there any secondary symptoms that accompany the patient's main complaint?
With the client's symptoms fully documented, you can move to the next portion of the note.
2. Objective
The patient's experience is central to effective treatment, but making observations from an impartial point of view helps round out what the patient told you.
The objective portion of a mental health SOAP note relates to how the body functions and evaluates neurological functioning with the Mental Status Exam.
What observations can you make about the individual? Write them down as factually as possible.
The Objective phase is concerned only with raw data, not conclusions or diagnoses on your part. Record any measurable data during the client's session, including applicable test scores.
Documenting the Objective phase brings up the issue of separating symptoms from signs. Symptoms are the patient's own experience of their condition, whereas signs are objective observations related to symptoms.
If a client reports having symptoms of anxiety, such as panic attacks, signs of that anxiety might include visible trembling or clenching of muscles as well as hypertension determined by a physical test.
You have a limited window for examination, so it's important to actively look for any signs that complement or contradict information given in the subjective section of the notes.
3. Assessment
Both the Subjective and Objective elements previously recorded come into effect in the Assessment phase. You will document your impressions and make interpretations based on the information you've gathered.
For an initial visit, the Assessment portion of your notes may or may not include a diagnosis based on the type and severity of symptoms reported and signs observed.
For common conditions such as depression, the Assessment is fairly straightforward and can often lead to a diagnosis in the first visit or two.
For rarer and more complex conditions or those that appear co-morbidly, you may need more time to gather information on the Subjective and Objective levels before arriving at a diagnosis.
For follow-up visits, the Assessment portion of mental health SOAP notes covers an evaluation of how the client is progressing toward established treatment goals. The Assessment will inform your current treatment course as well as future plans, depending on whether the patient is responding to treatment as expected.
It's essential to reflect on whether your client is showing improvement, maintaining improvements already made, worsening, or demonstrating patterns of remissions.
Like the other sections of the mental health SOAP note, your Assessment should only contain as much information as is necessary. Some Assessments will be significantly longer than others, based on the complexity of the patient's condition.
Sometimes this section of your notes will contain only a few snippets of information like, "Patient is sleeping better, no change in the incidence of panic attacks."
In other situations, there are more pieces to evaluate and your Assessment portion of notes should extend to include all the appropriate information.
Share this image with the following code:
<p><strong> www.ICANotes.com </strong><br /><br /><a href='https://www.icanotes.com/2018/04/25/tips-for-writing-better-mental-health-soap-notes'><img src='https://www.icanotes.com/wp-content/uploads/2018/04/Tips-for-Writing-Better-Mental-Health-SOAP-Notes-01.png' alt='Tips-for-Writing-Better-Mental-Health-SOAP-Notes-01' width='600' /></a></p>
4. Plan
This is where the previous three sections all come together to help you determine the course of future treatment. The Plan section of your mental health SOAP notes should contain information on:
- The treatment administered in today's session and your rationale for administering it
- The client's immediate response to the treatment
- When the patient is scheduled to return
- Any instructions you gave the client
- Goals and outcome measures for new problems or problems being re-assessed
Your Plan notes should include actionable items for each diagnosis.
If your client is experiencing multiple conditions, such as post-traumatic stress disorder (PTSD) in combination with a substance use disorder, your notes should include separate plans for each condition.
The goal of this section is to address all the specific deficits listed in the Assessment. When done efficiently, the Plan sets a clear roadmap for the patient's continuing treatment and provides a window of insight for other clinicians to continue that treatment if need be.
The Plan should be consulted on each new visit, and adjusted regularly based on the findings in the Assessment section.
Writing Mental Health SOAP Notes in ICANotes
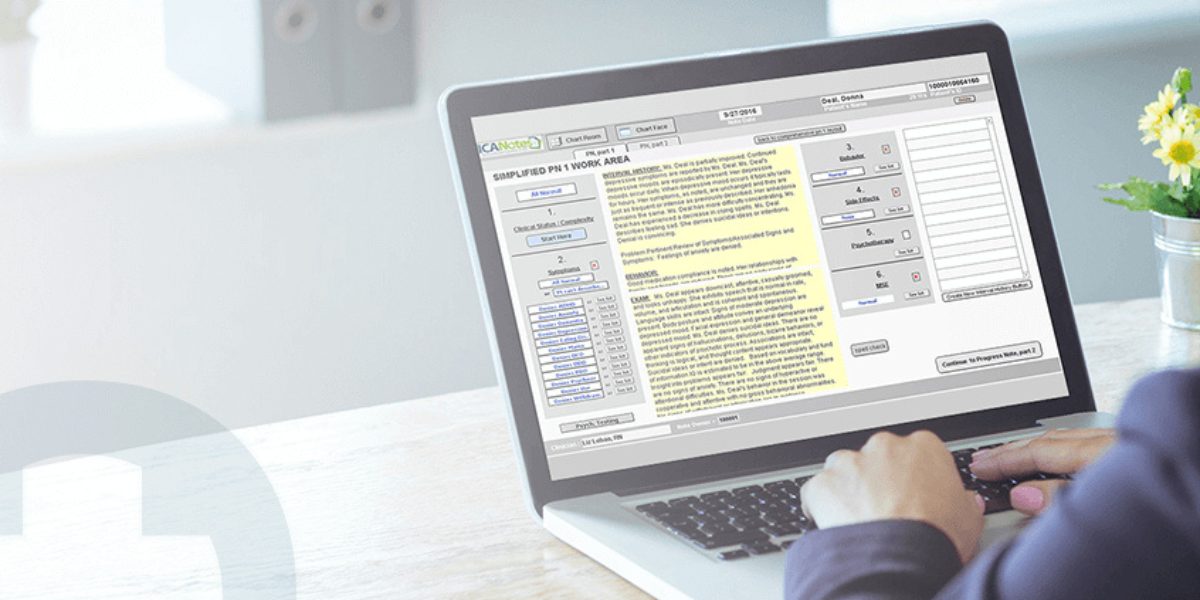
ICANotes is a behavioral health EHR that provides everything you need to create mental health SOAP notes with ease and accuracy. With our menu-driven templates, you can create a clinically significant psychotherapy note in just three minutes with hardly any typing.
Our system is highly intuitive and easy to use. It allows you to create your own templates in addition to using our clinically geared variety.
Check out a sample mental health SOAP note that was created using ICANotes, then schedule a demo to see our powerful system for yourself.
Why SOAP Notes are an Important Tool
SOAP is the most common format used by medical and behavioral health professionals, and for good reason. Since its development in the 1960s, the SOAP framework has been useful enough for health professionals of all stripes to implement it.
Of the many benefits SOAP provides, here are three of the most prominent.
1. Connectivity
Adoption of EHR systems is on the rise, with 89.6 percent of primary care providers and 61.3 percent of psychiatric practices using some form of electronic record. EHRs make integrated care possible by allowing medical and behavioral health professionals to access each other's notes on patients.
Using the SOAP framework enables practitioners of all specialties to communicate in a streamlined fashion, providing better care for each patient.
2. Accuracy
When healthcare providers are not using the same framework for notes, it's easy for critical information to get lost in translation when the next provider accesses the information. SOAP notes emphasize clarity and concision, which helps get every provider on the same page with minimal confusion.
The clear structure of SOAP notes also increases the accuracy of your notes in general. Rather than trying to remember everything that happens in an appointment and jotting it down stream-of-consciousness style, SOAP notes give you a way to structure your appointments to get the right information at the right time, making it easier to recall and accurately input all the necessary notes.
3. Efficacy
SOAP notes help support your end goal of providing the most effective care and treatment for your clients. The focus on Assessment and Plan keeps progress at the forefront of your sessions and offers a history of efficacy you can evaluate to see what's working and what isn't.
SOAP notes also create a paper trail of documentation that may be useful in the case of a malpractice suit. More commonly, mental health SOAP notes are required for insurance reimbursements in the case of a third-party audit. Switching to this note-taking technique is better for both your patients and your practice.
Mental Health SOAP Note Examples
View SOAP note examples:
The SOAP framework can be incorporated into any notes taken in a behavioral health care setting. To help you envision the ways you can integrate mental health SOAP notes into your practice, here are three situations in which the SOAP approach can clarify and simplify your documentation.
1. Psychiatry
You're treating a patient at an outpatient psychiatric clinic. We'll call her Mrs. D. You diagnosed her with Alzheimer's, dementia, and depression three months ago, and it's time for another follow-up appointment. To write her notes in the SOAP framework, you would follow these steps.
- Gather subjective information from the patient on her depression symptoms.
- Review lab test results to gather information on signs of the condition and compliance with the medication regimen.
- Review notes from the last visit to determine how Mrs. D is progressing with her treatment and evaluate whether her symptoms are getting better or worse.
- Based on her progression or lack thereof, you can decide whether to adjust her medication or make another alteration to her treatment plan.
In this case, Mrs. D is displaying signs of a worsening condition. The Subjective investigation reveals that her depressive symptoms have not abated, and she has been having outbursts of anger. Her daughter also reports that she has had trouble sleeping.
On the Objective end, you notice that her speech is loud and garbled, she has trouble naming objects, and she expresses inappropriate episodes of rage. She also cannot perform simple arithmetic calculations and is disoriented when it comes to date and location.
Your Assessment finds that she is not making progress on the current course of treatment, and you find that it may be appropriate to change her Plan going forward.
2. Individual Therapy
As medications and lab tests are not regular components of individual therapy, SOAP notes are even simpler to document.
In this case, we'll imagine treating a patient called Ms. P, who suffers from general anxiety, borderline personality disorder, and major depressive disorder.
Following the steps from the example above, Ms. P's SOAP notes might look like a longer version of this:
- Subjective: The patient states, "I feel better today. I think my depression is improving. The therapy is helping."
- Objective: Compliance with medication is good. Relationships are reduced. Work performance is marginal. The patient has maintained sobriety. Her weight is stable, and her food and fluid intake are normal. She has reported sleep problems with difficulty falling asleep and staying asleep.
- Assessment: Ms. P appears calm, attentive, and relaxed. There are no signs of bizarre behaviors, delusions, hallucinations, or other indicators of psychosis. The patient is fully oriented. The judgment appears fair, insight into problems appears normal, and the patient did not display signs of anxiety.
- Plan: The patient will replace negative and self-defeating talk with the verbalization of realistic and positive cognitive messages.
This patient's SOAP notes give a clear picture of the kind of progress she has made. In this case, the client is responding fairly well to treatment, and alteration of the Plan is not necessary.
3. Group Therapy
Creating group therapy notes is necessarily more complex than documenting individual sessions. You have multiple patients with multiple conditions that you have to keep track of, making it even more crucial to be succinct and precise in your notes. Each individual should have their own notes from each group therapy session, using the SOAP format.
Each individualized group therapy note should also include the group type, the agenda for that session, the group members present, and the interventions facilitated by the group leader.
Creating individualized SOAP notes for group therapy can be somewhat time-consuming, but is essential for monitoring progress over time.
Write Better SOAP Notes with ICANotes
The main drawback to mental health SOAP notes is that they can often be tedious to create. EHRs geared toward medical professionals just don't cut it for behavioral health specialists, and don't offer the features clinicians need to create effective mental health SOAP notes.
With ICANotes, you'll spend less time creating better documentation. Curious to see how it works? Register for a live demo of our platform, or claim a free trial to use the system for yourself.
Higher-quality mental health SOAP notes don't have to require harder work on your part. ICANotes is proud to provide professionals with a behavioral health EHR that understands your documentation needs.
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
Simplify clinical charting
Stay organized with appointment scheduling
Reduce no-shows with automated reminders
Improve client engagement with a secure patient portal
Provide flexible care with HIPAA-compliant telehealth
Frequently Asked Questions
Dr. October Boyles is a behavioral health expert and clinical leader with extensive expertise in nursing, compliance, and healthcare operations. With a Doctor of Nursing Practice (DNP) from Aspen University and advanced degrees in nursing, she specializes in evidence-based practices, EHR optimization, and improving outcomes in behavioral health settings. Dr. Boyles is passionate about empowering clinicians with the tools and strategies needed to deliver high-quality, patient-centered care.