Blog > Treatment Strategies > Anxiety and Substance Use
Anxiety and Substance Use: Breaking the Cycle
Anxiety and substance use frequently occur together, creating a complex and often self-perpetuating cycle that can be difficult to break. Individuals struggling with anxiety may turn to substances in search of relief, while substance use itself can heighten or even trigger anxiety symptoms. This bidirectional relationship between anxiety and addiction requires a thoughtful, integrated approach to assessment and treatment. In this article, behavioral health clinicians will learn how to recognize the interconnected nature of these conditions, navigate diagnostic challenges, and implement evidence-based strategies that support long-term recovery.

Last Updated: April 23, 2025


What You'll Learn
- How anxiety and substance use disorders develop and reinforce one another
- Common substances associated with self-medication for anxiety
- Ways substance use can lead to or worsen anxiety symptoms
- Challenges in diagnosing co-occurring anxiety and addiction
- Evidence-based therapies and pharmacological options for dual diagnoses
- Strategies to break the cycle and support long-term recovery
Bidirectional relationships exist in so many aspects of mental health and psychological treatment. Often, a person has an issue, and as they work to improve that issue, they inadvertently create another issue. By the time they present to therapy, the client could have a host of interconnected and unwanted concerns.
The relationship between anxiety and substance use is a prime example of these interconnected problems. In their lifetime, more than 28% of people will have an anxiety disorder, while more than 14% will have a substance use disorder. These are among the most common mental health conditions with one frequently leading to the other.
Mental health professionals should do themselves and their clients the service of assessing and treating these co-occurring disorders. Treating only one will never lead to the desired results in the long-term.
Understanding the Anxiety-Substance Use Connection
Bidirectional relationships can form in a number of different ways. In some cases, there is one condition that clearly precedes the other, but in other situations, they both seem to emerge at the same time, which makes proper diagnosis and treatment exceptionally challenging.
When Anxiety Leads to Substance Use
Imagine a teenager that is constantly worried about grades, friends, and sports. They were invited to a party on Friday night but feel too stressed out to go. In an effort to try and help the situation, the teen’s friend suggests having a few beers to “relax.”
The effects of alcohol calm the person by disrupting the typical levels of neurotransmitters in the brain and body. The drinking doesn’t end there, though. They drink again and again whenever they feel anxious or predict an anxious situation is on the horizon.
Over time, this pattern becomes a habit and alcohol use becomes a recurring negative coping skill called self-medication. Now, the teen only feels calm when they are drinking. This routine provides temporary relief while building a strong association between substance use and lower anxiety.
In this example, alcohol is the substance, but other people use other legal and illicit substances to induce relaxation like:
- Marijuana/ cannabis
- Benzodiazepines, like Xanax, Ativan, Valium
- Opioids, like hydrocodone, oxycodone, heroin
- Sleeping medications, like Ambien, Lunesta, Sonata
Whether it’s to feel calm mentally or physically, these substances are used widely to fight the feelings of stress and anxiety.
When Substance Use Leads to Anxiety
As mentioned, the relationship is bidirectional, so anxiety leads to substance use and substance use leads to anxiety. In this situation, people with a history of substance abuse can experience anxious feelings, either as a direct effect of the drug or as a withdrawal symptom.
The Drug’s Direct Effects
A group of medications work by stimulating, or speeding up, the central nervous system. Called stimulants, people use these substances to get more energy, stay alert, or to feel high. At higher doses, these drugs can create anxiety, fear, and paranoia.
Some substances that trigger anxiety include:
- Cocaine/ crack cocaine
- Amphetamine and methamphetamine
- Nicotine
- Caffeine
The Drug’s Withdrawal Effects
Substances that trigger addiction and tolerance may also create a response where the client will need the drug to feel well and function normally. When this dependence is in place, the person will experience uncomfortable withdrawal symptoms when the substance is not available.
With many substances, the withdrawal effects are the opposite of the intoxication effects. So depressant substances that calm someone down will create stress, nervousness, and restlessness during withdrawal. This result means that the anxious teen from the first example could feel calm when under the influence and then note a higher level of anxiety during withdrawal.
The Drug’s Situational and Social Effects
Alcohol and other drugs create a drastic impact on the client’s mental health, physical health, and overall well-being. The social effects of ongoing use start to accumulate and create new and worsening issues.
Secrecy, lying, and manipulation are common actions for someone in the depth of substance use. These responses center around decreasing stress and negativity in relationships, but in the long-term, they create more anxiety. As the person is constantly having to recall what they said, who they said it to, and what the other person’s response was, they can experience higher levels of worry.
They know that the entire lie they’ve been living can come crashing down at any moment. The anticipation of this can become overwhelming.
The Vicious Cycle
In all of these situations, substance use and anxiety feed off of each other in a cycle. As anxiety increases, higher doses or stronger substances are needed to neutralize the effects. When substance use grows, anxiety results from intoxication or withdrawal. In all cases, the social and situational anxieties expand.
If the person didn't have a diagnosable anxiety disorder at the beginning, enough cycles of this will result in one. If the person didn't have a diagnosable substance use disorder initially, enough repetitions of this vicious cycle will create one.
What makes this cycle even more challenging is that when the person makes a concerted effort to end it, the psychological and physical toll is intense enough to encourage the pattern to continue.
Diagnosing Co-Occurring Disorders
Whether the client has an anxiety disorder, a substance use disorder, or some combination of multiple conditions, they need comprehensive treatment designed to address all of their symptoms and conditions in a holistic way. Depending on laws and regulations in your state, you might be limited in your ability to treat mental health and substance use disorders. If this is the situation, be sure to consult with a collaborative treatment team.
Challenges in Diagnosis
The assessment and diagnosis process is complex for a number of reasons. Issues that can confuse and cloud the evaluation include:
- The substance or substance used
- The frequency, intensity, and duration of use
- Date of last substance use
- Existence of symptoms of one condition before symptoms of another
- The ability of the client to be an accurate historian
- Separating withdrawal/rebound symptoms from actual mental health symptoms
Completing an accurate evaluation may seem intimidating, but there is good news. Diagnoses never have to last forever. As time goes on, clinicians can adjust and revise their views.
The most effective assessment strategies involve really thoughtful, in-depth interviewing. Standardized assessments are valuable, but they may miss some of the nuance involved in the cause-and-effect, bidirectional relationship of addiction and recovery.
Treatment Approaches for Breaking the Cycle of Anxiety and Addiction
Once an acceptable diagnosis is made, the treatment can begin. As mentioned, the best treatments will involve a person’s whole self to address their physical health, mental health, and overall well-being.
Integrated Treatment for Anxiety and Substance Use
Integrated treatment isn’t only about talking about all of the symptoms. It is really centered around having a sound, complete plan to address each condition in a complementary way, while acknowledging that only targeting one set of symptoms can lead to another set of symptoms becoming more prominent.
Mental health professionals should always be aware of their areas of expertise, their limitations, and resources for collaboration. Having a set of mental health and substance use contacts can help to streamline care and build a network of trusted connections.
Psychotherapeutic Interventions for Addiction and Anxiety
Because the treatment approach will be integrative and comprehensive, clinicians need to consider the theoretical orientations that best meet their client's current status and future goals. Some behavioral approaches are evidenced-based solutions for a variety of mental health and substance use disorders, so rather than switching drastically between styles, practitioners can employ one foundational strategy to create the desired outcomes.
Treatment options offer clients a sense of control and resiliency over their conditions. They teach clients that anxiety and addiction, though very challenging at times, are comfortable and manageable situations. With relapse prevention strategies, focus on self-awareness, and methods to increase healthy social supports, clients will be in a better position to achieve periods of sustained recovery from anxiety and addiction.
Some of the best therapies for addiction and anxiety include:
- Cognitive-behavioral therapy (CBT) - CBT is a wonderful framework for so many conditions. Various anxiety disorders have CBT interventions specifically designed for their impact, but with its focus on thoughts, feelings, and behaviors, CBT is a great first line approach for anxiety and recovery.
- Dialectical behavior therapy (DBT) - DBT is separated into modules of mindfulness, distress tolerance, emotional regulation, and relationships skills. All of these areas are essential for a person hoping to overcome addiction and anxiety.
- Exposure therapy. Even though exposure therapy is technically a form of CBT, it deserves a special callout. Instead of using therapy to modify the person’s distorted thinking patterns, exposure therapy doubles down on behavioral changes and getting the person to experience the discomfort in safe and controlled ways.
When designing a comprehensive and integrative treatment plan, clinicians should select therapeutic frameworks that align with the client’s current needs and long-term goals. As symptoms change with periods of recovery, different treatment approaches and interventions may be more valuable. The end goal of therapy is usually the same, but the path to that destination may involve several twists and turns.
Pharmacological Options for Anxiety and Substance Abuse
Depending on the individual, their set of symptoms, and their long-term goals, medications could be as important to treatment as therapy. Being a part of a mental health agency or group private practice can give clinicians access to pharmacological evaluations completed by a psychiatrist or nurse practitioner, while those in private practice may need to rely on strong relationships built with outside prescribers.
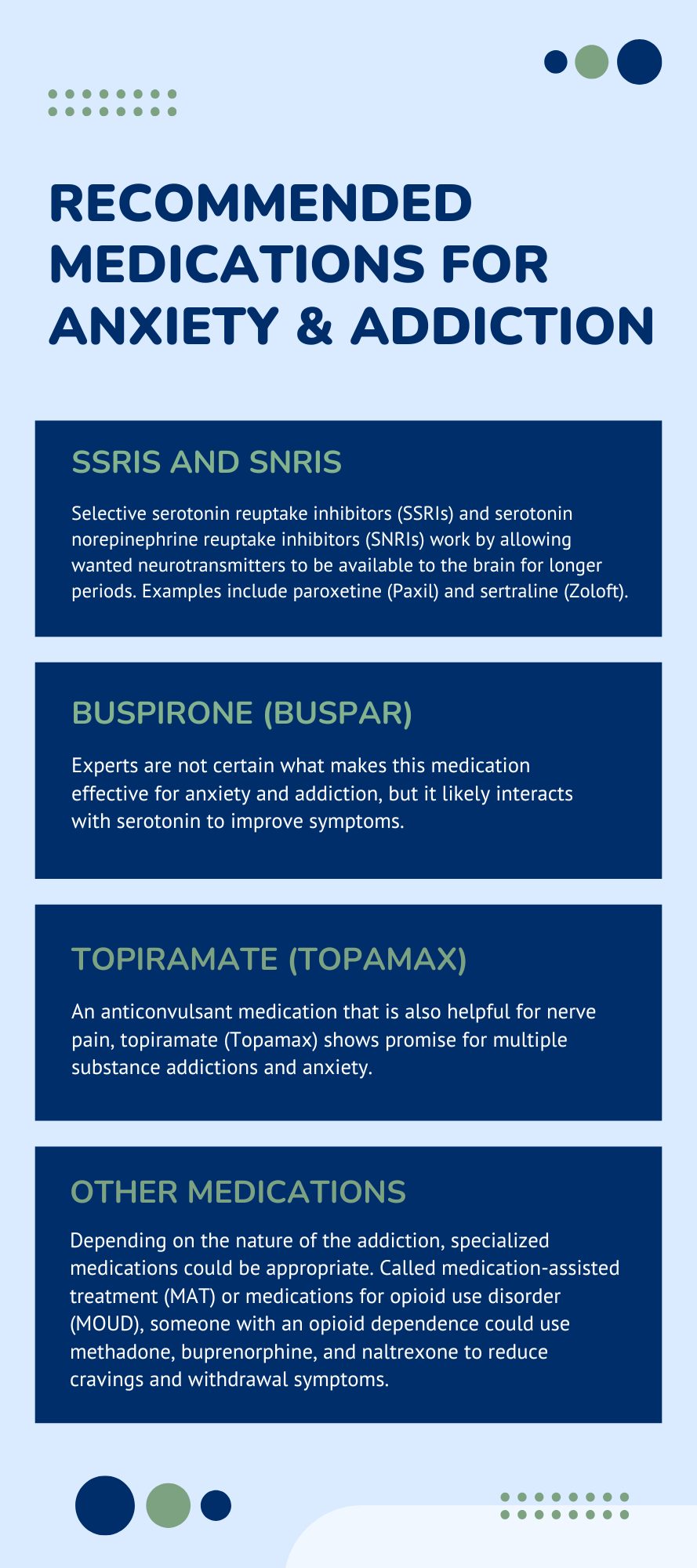
Generally, therapists should avoid making any assessments or claims about medications to their clients, but it is always appropriate to note when therapy alone may be insufficient to manage all symptoms. For a client experiencing symptoms of anxiety and addiction, recommended medications may include:
- SSRIs and SNRIs. Selective serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs) work by allowing wanted neurotransmitters to be available to the brain for longer periods. Examples include paroxetine (Paxil) and sertraline (Zoloft).
- Buspirone (BuSpar). Experts are not certain what makes this medication effective for anxiety and addiction, but it likely interacts with serotonin to improve symptoms.
- Topiramate (Topamax). An anticonvulsant medication that is also helpful for nerve pain, topiramate (Topamax) shows promise for multiple substance addictions and anxiety.
- Other medications. Depending on the nature of the addiction, specialized medications could be appropriate. Called medication-assisted treatment (MAT) or medications for opioid use disorder (MOUD), someone with an opioid dependence could use methadone, buprenorphine, and naltrexone to reduce cravings and withdrawal symptoms.
When considering medication management for anxiety and addiction, it is best to leave the suggestions or final decisions to the prescriber. They will consider many aspects of the client’s presentation to identify the medication that makes the most sense.
Holistic and Lifestyle-Based Approaches
For most clients, professional treatment options are necessary components to recovery, but people should never rely on these exclusively. By encouraging clients to add complementary treatments, they gain a range of benefits.
For example, support groups for recovery or anxiety can add a level of peer encouragement, community, and guidance that therapists may not offer. Alcoholics Anonymous, Narcotics Anonymous, and specific groups for people with anxiety can supplement professional appointments.
On an even more basic level, encouraging clients to care for their physical health can make a huge difference. When clients are eating well, getting enough quality sleep, and exercising, they put themselves in a better physical and mental state, which will boost the effects of other treatments.
Lastly, clients in early recovery may struggle to find a sense of meaning, purpose, and fulfillment. Exploring work, volunteer opportunities, and hobbies helps give life structure and direction.
Challenges Clinicians May Face in Treating Anxiety and Substance Use
When mental health conditions co-occur, the clinician will naturally encounter a series of challenges. From assessment throughout treatment, the path to sustained recovery is rarely a straight line. Therapists must remain flexible, yet consistent. They must lead the client towards new and uncomfortable coping skills while taking feedback and adjusting the plan.
Clinicians will likely face challenges like:
- Relapses. Relapses are a part of recovery for many, and when they present, how the therapist and client react will have a huge impact on future treatment. Relapses are a sign that treatment should be adjusted, but not abandoned or changed completely. Small tweaks usually create wanted results.
- Missed appointments. People with addiction and anxiety histories may struggle with consistent attendance. Therapists should set clear expectations and enforce the boundaries as needed.
- Medication issues. Adding medication to the treatment plan can bring great success, but it may take several trials to get the best fit. Clients and clinicians should stay optimistic and flexible with dosing and results.
- Early withdrawal. Some clients become overly confident early on in treatment and consider ending treatment prematurely. Although it is the job of the therapist to capitalize on this optimism, they need to set realistic expectations for the client and remind them that longer periods of treatment are associated with longer periods of recovery.
How ICANotes Supports Clinicians Treating Anxiety and Substance Use
Effectively treating co-occurring disorders like anxiety and substance use requires not only clinical expertise but also accurate, efficient, and compliant documentation. That’s where ICANotes comes in. Designed specifically for behavioral health and addiction treatment, ICANotes helps clinicians streamline documentation without sacrificing clinical depth or compliance. With structured templates for initial assessments, treatment plans, and progress notes, providers can clearly track the interplay between anxiety symptoms and substance use patterns over time. Each template includes fully configured menu-driven clinical content specific to mental health disorders and chemical dependency treatment.
ICANotes also enables:
-
Integrated treatment planning that links presenting symptoms to specific interventions and measurable goals
-
Risk factor tracking for behaviors such as self-medication, relapse triggers, and withdrawal concerns
-
Customizable templates for documenting therapy modalities like CBT, DBT, and motivational interviewing
- Electronic Rating Scales for evidence-based assessment and outcomes measurement
-
Collaboration tools that support coordinated care among mental health and addiction treatment teams
-
Efficient documentation workflows that reduce administrative burden and free up more time for direct client care
By using ICANotes, clinicians can enhance both the quality of their documentation and the effectiveness of their treatment, helping clients with anxiety and addiction achieve better outcomes with less friction.
Final Thoughts on Anxiety and Addiction
Treating anxiety and substance use isn’t just about breaking a cycle—it’s about building something stronger in its place. With a comprehensive approach that addresses the emotional, behavioral, and physical dimensions of recovery, clinicians can help clients reclaim a sense of control, stability, and hope. While the path may involve setbacks and recalibration, the destination—sustained recovery and improved quality of life—is absolutely attainable. With the right tools, like ICANotes, and a clear therapeutic plan, providers can guide clients toward meaningful, lasting change.
Get Your Free 30-Day Trial of ICANotes (no credit card required!)
Related Posts
Eric Patterson, MSCP, NCC, LPC, is a professional counselor who has been working for over a decade to help children, adolescents, and adults in western Pennsylvania reach their goals and improve their well-being.
Along the way, Eric worked as a collaborating investigator for the field trials of the DSM-5 and completed an agreement to provide mental health treatment to underserved communities with the National Health Service Corp.






