Blog > Documentation > Why Narrative Behavioral Health Progress Notes Matter
Why Narrative Behavioral Health Progress Notes Matter: How ICANotes Makes Charting Effortless and Accurate
In a digital world filled with checkbox templates and time-consuming clinical documentation, narrative behavioral health progress notes remain essential for quality care and compliance. This blog explores how ICANotes helps mental health professionals like psychiatrists and therapists create rich, accurate, and audit-ready session notes in less time using its intuitive, menu-based system.

Last Updated: May 12, 2025

Why Behavioral Health Progress Notes Still Matter in a Digital World
In a time when therapists and psychiatrists are juggling packed caseloads, compliance pressures, and increasing clinical documentation demands, behavioral health progress notes often become just another checkbox. But notes are a cornerstone of quality care. The narrative format — detailed, descriptive, and human — remains one of the best ways to capture the richness of a session. And with the right electronic health record (EHR), writing these mental health progress notes doesn’t have to be time-consuming.
ICANotes was designed from the ground up with behavioral health in mind. Unlike generic or checkbox-heavy systems, it offers an intelligent, menu-based interface that generates high-quality narrative therapist notes and psychiatric notes with ease and speed. Here’s why that matters — and how ICANotes makes it possible.
The Challenge — Session Notes That Are Either Too Sparse or Too Time-Consuming
Mental health counselors and psychiatrists often face a frustrating trade-off: spend valuable time crafting detailed, personalized notes, or resort to generic templates that barely reflect the nuances of a therapeutic session. This challenge becomes even more pressing in high-volume practices, where clinicians may see eight or more clients a day.
Poor documentation can have serious consequences:
- Clinical Gaps: Vague or incomplete progress notes can leave out key details that impact treatment planning.
- Audit Risk: Non-compliant session notes can jeopardize reimbursement and put your practice at legal risk.
- Team Communication: In group practices, sparse therapy documentation makes handoffs or collaboration more difficult.
- Burnout: The pressure to document extensively after hours contributes to clinician fatigue and job dissatisfaction.
In contrast, comprehensive narrative behavioral health progress notes preserve the patient’s story in context. But writing them by hand after each session can eat up hours every week. This is where many EHRs fall short. While platforms like TherapyNotes and SimplePractice offer structured note templates and dropdown menus, these tools often result in repetitive, robotic language and force clinicians into unnatural clinical documentation patterns.
Clinicians need something better — a system that supports personalized and comprehensive narrative documentation without slowing them down.
Download Our Guide to Writing Better, Faster Clinical Notes
Streamline your progress notes, avoid documentation pitfalls, and stay compliant with practical templates, note formats (SOAP, DAP, BIRP), and time-saving tips to write high-quality, defensible notes faster.
The ICANotes Solution — Smart, Narrative Therapy Documentation
ICANotes solves the clinical documentation dilemma by combining speed and clinical depth. At the heart of its system is a proprietary menu-driven clinical content engine that helps therapists and psychiatrists build thorough progress notes through intelligent selection rather than excessive typing.
Click-to-Compose Narrative Behavioral Health Progress Notes
ICANotes lets you build complete, natural-sounding mental health progress notes by clicking through structured menus of relevant phrases—each selection automatically generates a dynamic sentence tailored to the session, so you can document thoroughly without typing.
For example:
"The patient reported experiencing increased anxiety in social settings, particularly in the workplace, accompanied by physiological symptoms such as rapid heartbeat and sweating."
This sentence may require three clicks in ICANotes, but takes over 20 seconds to type manually. Multiply that by 10 notes a day, and you save hours every week.
Structured for Compliance, Styled for Humans
ICANotes easily formats progress notes according to popular clinical structures like SOAP, DAP, BIRP, and PIE. These formats are embedded within the note-building process, so clinicians don’t have to worry about structure, only substance. This helps ensure documentation is:
- Audit-ready
- Reimbursement-compliant
- Easily reviewable by colleagues or supervisors
Unlike checkbox-only systems, ICANotes progress notes are written in paragraph form. This makes them easier to read, easier to explain to clients (when appropriate), and more reflective of the provider's clinical reasoning.
Fully Customizable Phrases
ICANotes offers over 75,000 clinical phrases out of the box — and you can also add your own. This is especially useful for specialized practices (e.g., trauma-informed therapy, substance use recovery, child psychiatry) that use unique terminology or processes.
Seamless Integration With Other Practice Functions
Each behavioral health progress note is automatically tied to a scheduled session, and can be linked to billing codes, clinical forms, and treatment plans. This reduces duplicate data entry and ensures alignment between documentation and billing.
ICANotes vs. Other EHRs — The Narrative Advantage
Let’s examine how ICANotes compares to other popular systems used in behavioral health like TherapyNotes and SimplePractice:
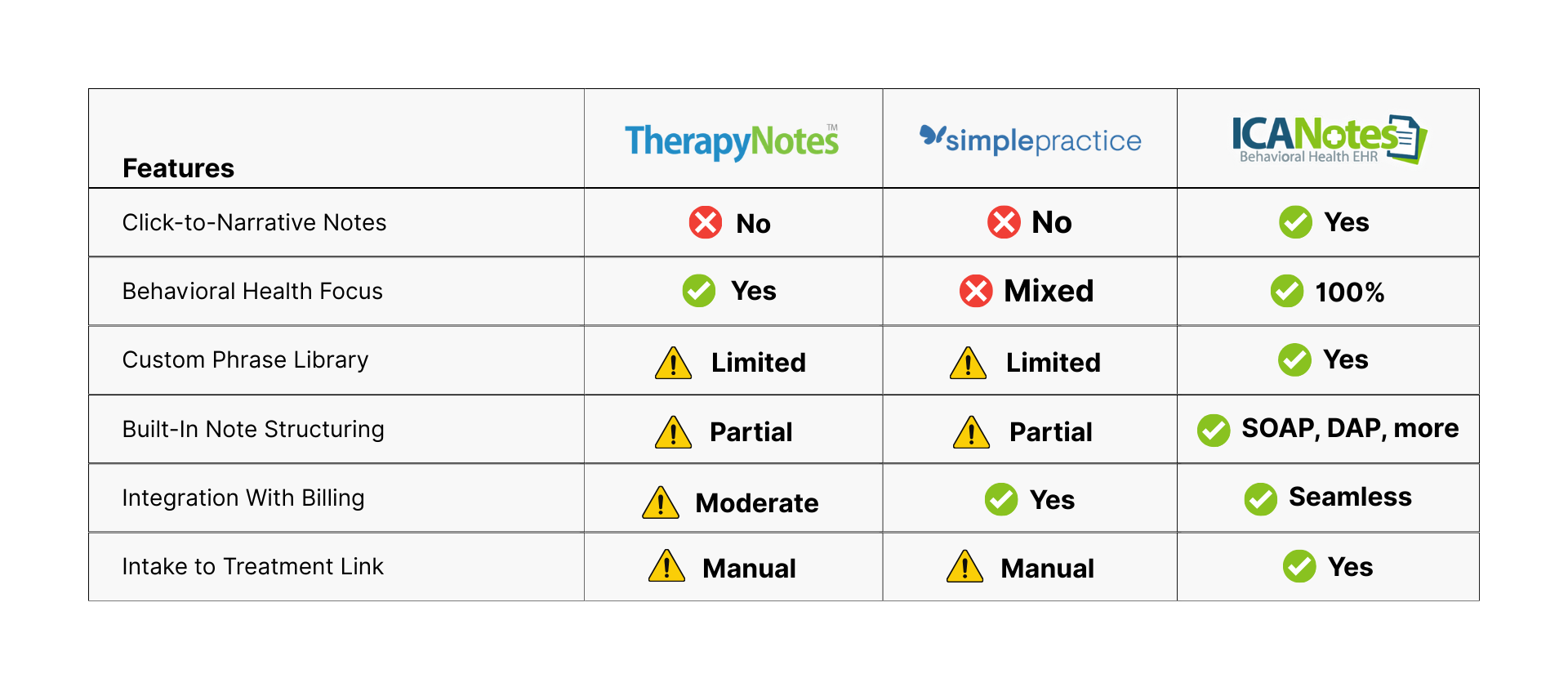
Most EHRs were either designed for general medical use or only lightly customized for behavioral health. ICANotes was created by mental health clinicians, and its documentation tools reflect a deep understanding of the therapeutic process.
For example, TherapyNotes offers basic templates but requires a lot of free-text customization. SimplePractice’s form builder is great for intake, but less useful for behavioral health progress notes. In contrast, ICANotes brings clinical depth without requiring extensive configuration.
Behavioral Health Progress Notes That Tell the Whole Story (in Half the Time)
Narrative notes remain the gold standard for therapy and psychiatric documentation. They communicate nuance, support high-quality care, and protect your practice. But traditionally, they’ve come at a cost: time.
ICANotes changes the game by letting you document richly, quickly, and in a format that supports both your clinical thinking and your operational workflows. Whether you're a solo practitioner or part of a large group practice, ICANotes helps you:
- Spend less time on documentation
- Improve note quality
- Stay compliant
- Reduce burnout
If you're tired of rigid checkboxes or spending nights catching up on notes, it might be time to try a smarter solution.
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
- Complete Notes in Minutes - Purpose-built for behavioral health charting
- Always Audit-Ready – Structured documentation that meets payer requirements
- Keep Your Schedule Full – Automated reminders reduce costly no-shows
- Engage Clients Seamlessly – Secure portal for forms, messages, and payments
- HIPAA-Compliant Telehealth built into your workflow
Complete Notes in Minutes – Purpose-built for behavioral health charting
Always Audit-Ready – Structured documentation that meets payer requirements
Keep Your Schedule Full – Automated reminders reduce costly no-shows
Engage Clients Seamlessly – Secure portal for forms, messages, and payments
HIPAA-Compliant Telehealth built into your workflow
Related Posts
Dr. October Boyles is a distinguished healthcare professional with extensive expertise in behavioral health, clinical leadership, and evidence-based care delivery. With a Doctor of Nursing Practice (DNP) from Aspen University and advanced degrees in nursing, she brings a depth of clinical knowledge and a passion for improving mental health care services.