Blog > Documentation > How to Write a Group Therapy Note: Templates, Tips & Examples
How to Write a Group Therapy Note
Group therapy notes are essential for documenting client progress, ensuring continuity of care, and supporting insurance reimbursement. Whether you're just beginning to facilitate group therapy or you're refining your note-writing process, mastering the group therapy note is critical. In this guide, you'll learn how to write effective group therapy notes that align with best practices in behavioral health and meet the requirements of payers and clinical standards.

Last Updated: August 26, 2025

What is a Group Therapy Note?
A group therapy note is a specialized progress note that records the details of a group therapy session, including client participation and progress toward treatment goals. Each session generates individual notes to prove medical necessity and may be required by insurers for reimbursement. Typically, a group therapy note begins with a group summary, discusses the topic, documents interventions, and concludes with observations on each client's participation.
Differences Between Group Therapy Notes and Individual Notes
Group therapy notes and individual therapy notes have a few differences. Group therapy notes focus on the dynamics among group members, including their interactions and mutual influences. Individual therapy notes center on one-on-one progress between the therapist and the client.
Record keeping for group therapy sessions requires extra attention to confidentiality. Although HIPAA and the American Psychological Association only provide detailed guidelines for privacy and confidentiality rules for individual therapy notes, you can apply those same best practices to group therapy with a few additions, such as:
- Creating a separate record for each group member
- Using initials for other group members when documenting interactions, and including only essential identifying information.
- Writing general notes about group interactions and interventions to include in each participant's progress note.
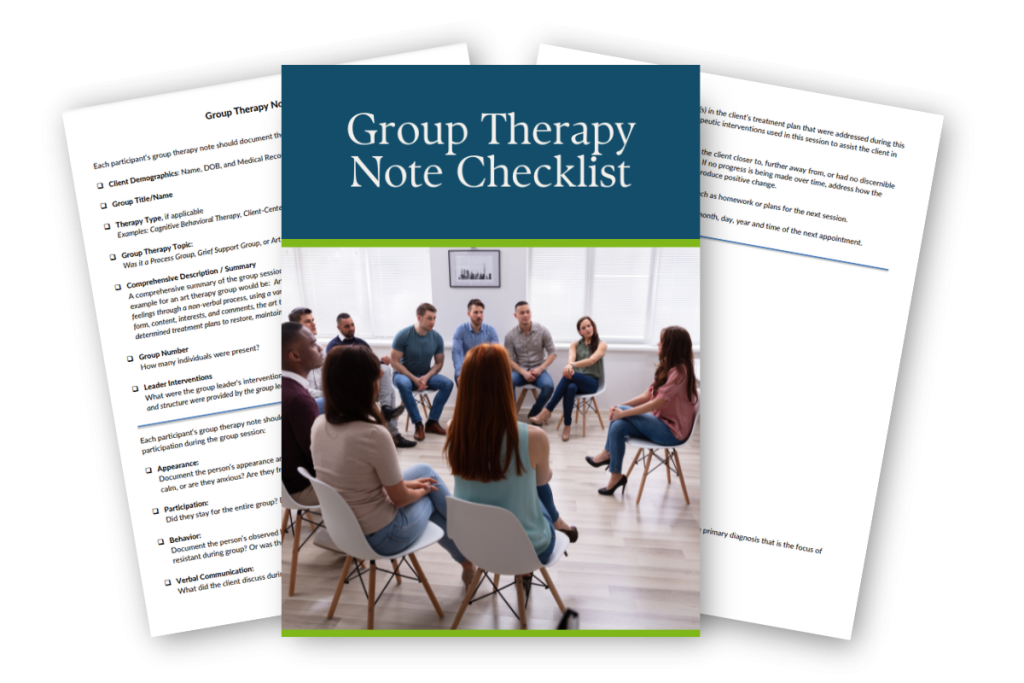
Free Download: Group Therapy Note Checklist
Grab our free Group Therapy Note Checklist—a comprehensive, printable tool to ensure every session is well-documented, clinically sound, and insurance-ready.
The Elements of a Group Therapy Note
Overall, group therapy notes are not much different than the progress notes you write for individual client sessions. For example, you can use the SOAP (an acronym for Subjective, Objective, Assessment, and Plan) note format for individual group therapy notes, just as you would for regular progress notes. The difference is you'll include a brief group summary at the top of each note and incorporate details about the session throughout the document.
Regardless of the note-writing format you use, be sure to describe the client's participation in the group, how they reacted to the session, and how the meeting addressed their treatment goals.
To help you get started, here are 12 essential elements to include in individualized group therapy notes.
1. Group Summary
Each note for individual clients should begin with a group synopsis. You might include the following details:
- Group name
- Discussion topic
- Session date and times
- Schedule and format
- Counselor's name
- Number of group members in attendance
- Interventions used in the group session
You can use the same group summary for each client. If you do so, make sure it does not include individual client names. You might create an attendance list and file it in a separate folder.
2. Identifying Information
Ensure each note includes accurate identifying information such as:
- Client's full name
- Client's identification number
- Client's date of birth
- Your organization's name
Depending on your practice, you may need to include a few other details, such as the client's gender or contact information.
3. Mood and Appearance
Note the client's demeanor, mood, and general appearance using a mental status exam checklist for clarity.
4. Behavior
Describe each group member’s participation, willingness to share insights, and response to other group members in the therapy session.
5. Issues and Events
List any new issues or conflicts that arise with other group members and interventions used to address them. For example, if a client becomes angry and argues with another group member, describe how you intervened and helped them identify the source of their anger.
6. Patient-Group Interactions and Reactions
Detail how each client interacts with the group and vice versa, noting whether they are active, passive, included, or isolated. In each group member's note, discuss how they engaged with the group and the contributions they made. Do they assume the role of the group leader or are they more timid? Is the group receptive and welcoming to the individual or do they have difficulties integrating and accepting them into the discussion?
7. Patient-Group Influences
Explain how clients influence group dynamics and how the group impacts each client’s attitudes or decisions. Every individual member will play a different role in how the group functions as a whole. Detail how each of your clients contributed or influenced the group. For instance, did they have a significant effect on the direction of the conversations or topic? Did they have a heavy influence on the tone of the overall interaction?
As you should describe how each client influenced the group, you should also explain how the group influenced each client. Describe the nature of how the group did this and the effect it had. Did the group's support positively influence the client and make them feel encouraged about the possibility of change? Did the group's agreement or disagreement on a particular topic affect the client or make them feel excluded? Was the group able to change the client's mind about a specific issue?
8. Goals and Objectives
Relate session content to the client’s treatment goals and objectives, ensuring progress is documented for each group therapy session. For instance, imagine a client's goal is to stop abusing alcohol. They have several objectives in their treatment plan to help them achieve this, such as identifying triggers that lead to their alcohol use. Include this specific objective if the group therapy session focuses on identifying substance use triggers.
9. Therapeutic Interventions
List specific therapeutic interventions and techniques, such as exercises or group discussions, used to address treatment plans. For example, you might write that you taught the group a breathing exercise to help members reach their goal of feeling less anxious.
10. Response or Progress
Update on the client’s response to the session, whether they moved closer to their treatment goals, or if further strategies are needed. Include if the session moved the client away from their objectives or made no impact. For example, you might add that a client listened to the group's feedback but did not seem interested in applying their suggestions. If the client does not eventually make progress, you may want to include how you will change your strategy.
11. Plan and Additional Information
Outline plans for future sessions and note assigned homework, anticipated absences, or new strategies learned.
12. Signature and Date
Each note should conclude with the therapist's signature, credentials, and the time and date of the session and next appointment. If needed, get your supervisor's signature as well.
How to Write Better Group Notes
Like individual progress notes, group notes should be accurate, detailed, and easy to read. Well-written notes reduce the likelihood that your insurance claims will get denied. They also help you monitor a client's overall progress and develop effective treatment plans. Here are a few tips to help you write quality group therapy notes.
Use Objective Language
Be sure to write your group notes using an objective tone. Keep descriptions neutral and focused on observable facts, steering clear of biased language about group members. Avoid wording a reader could interpret as judgmental.
Keep Notes Confidential
Comply with HIPAA by omitting names or identifying information of other group members wherever possible.
Be Clear and Concise
If multiple professionals are running your group, your notes will be the main element in continually driving progress. Others will need to understand the specifics of past meetings, allowing them to pick up and continue therapy seamlessly. Ensure you have clearly stated your analysis of the current session and that the discussed plan for progress is easy to understand.
Use Methods and Interventions
Describe any methods, techniques, or interventions you used in the group therapy session and align your note documentation with treatment goals. These could be things like open-ended questions, exercises, meditations, affirmations, or other strategies you use to help your client or group achieve a goal. For example, based on the topic of the group discussion, you might help your clients come up with a plan that each person can apply to their personal circumstances and include these details in your notes.
While you may develop these methods and interventions on your own, you can also encourage your clients to help create unique interventions they think might help them accomplish their personal and common goals outside the therapy room.
Regardless of what types of methods or interventions you use, your notes should always align with HIPAA guidelines to protect your clients and your practice.
Maintain Efficiency When Writing Group Notes
Write notes promptly after each session, using templates for clarity, organization, and faster documentation.
When completing your notes, consider your usual process and determine if there are any areas for improvement. If you usually don't write notes until hours after your session, you'll likely forget many important details. If you need some time to decompress after each session before you tackle your group therapy notes, try not to wait too long before getting them started. You may feel less frustrated because the appointment will be fresh in your mind.
Another key to efficiency when writing group therapy notes is to know what critical information you need to include before you even start writing. If you're inclined to give a long, descriptive account of each session, you will likely spend hours on your notes, particularly if you have many clients. Using templates can help you keep your notes organized, clear, and concise, especially when they're tailored to your client's presenting condition, such as substance use disorder, or the treatment plan you're using. Remember, more detail doesn't mean more accuracy, and longer notes will only usually make it more difficult for you to sift through them later when you're reviewing. Stick to the most essential details and topic of the session as much as possible.
Group Therapy Note Example
When writing your group notes, it's always helpful to use a therapy note template to keep them organized, concise, and relevant to the session topic. One of the most commonly used templates in therapy is the SOAP method, which includes:
- Subjective: Quotes or complaints directly from the client, referencing other group members only by initials. Use a few sentences to describe the most pressing concern or issue they brought up during the discussion. Discuss their complaints, symptoms, or life events in their own words.
- Objective: Factual observations from the therapy session, omitting judgment or opinion. This may include the client's demeanor, appearance, or body language. Use this section almost as if you were conducting a physical examination of your client.
- Assessment: Synthesized analysis of the client’s progress toward goals in context of group dynamics. You can include screening results, goals, interventions, and objectives you addressed in group therapy for this individual.
- Plan: Outlines future steps, assigned exercises, and adjustments to the treatment plan for the next group session.
Sample Group Therapy Note (SOAP Format)
Client Name: J.S.
Group Name: Anxiety Management Group
Date: August 22, 2025
Therapist: Taylor Lee, LCSW
Start/End Time: 2:00 PM – 3:00 PM
S – Subjective
Client reported experiencing increased anxiety over the past week, particularly in social settings. Stated, "I feel like everyone is judging me when I speak." Expressed nervousness about an upcoming work presentation. Client shared feeling comforted hearing others in the group express similar fears.
O – Objective
Client arrived on time, appropriately dressed, and maintained good eye contact throughout the session. Participated actively in discussion and completed a brief mindfulness breathing exercise without hesitation. Demonstrated improved posture and decreased fidgeting compared to prior sessions.
A – Assessment
Client continues to demonstrate symptoms consistent with social anxiety but is progressing toward treatment goals. Engagement level has increased, and client appears to be developing insight into thought patterns that trigger anxiety. Peer validation and normalization appear to be helpful motivators.
P – Plan
Client will practice the 4-7-8 breathing technique daily and reflect on its impact in the next session. Will also journal about a recent anxiety-provoking event and bring the entry to the group next week. Continue participation in weekly group sessions. Monitor for continued progress and potential individual support needs.
Access Our Sample Notes Library
Get instant access to our full library of sample behavioral health notes, including Initial Evaluations, Progress Notes, Treatment Plans, and Discharge Summaries. We have note samples for psychiatry, therapy, case management, PRP, substance abuse, group therapy, couples therapy, and more!
Benefits of Writing Good Group Therapy Notes
Now that you've seen a group therapy note example and know how to take more effective, clear notes, let's review some of the top benefits of improving your note-writing process:
- Keep you organized: Using a template and knowing exactly what information you need to record before you begin writing your notes can prevent you from spending hours searching for the right documents later on.
- Refresh your memory: As a therapist, you may have dozens of clients that you see weekly, especially during group sessions. Writing organized notes makes it easy to review each client's current progress before starting your group session you can jump right back where you left off.
- Reduce repetition and wasted time: Without following a format for your notes, it can be easy to repeat yourself and spend more time restating the same details you've already written. Writing more efficient notes means reducing documentation time overall by focusing only on key information.
- Make billing easier: Keeping your notes accurate, legible, and detailed enough to comply with insurance companies' requirements may make it easier and faster for you to get paid.
- Streamline your workflow: Having a solid note-writing process can help you spend more time with your patients and less time worrying about when you'll be able to fit in documentation time. Writing your notes more quickly and efficiently may allow you to focus more on other critical tasks in your practice.
Frequently Asked Questions: Group Therapy Notes
Write Streamlined Group Therapy Notes with ICANotes EHR Software
Group therapy sessions are a powerful tool for helping clients connect, reflect, and heal—but documenting each participant’s progress shouldn’t feel overwhelming. ICANotes makes the group note-writing process faster and more accurate with built-in tools designed for behavioral health clinicians.
You can easily schedule recurring group appointments using a shared roster, automatically track attendance, and generate a single session note that flows into each participant’s chart. ICANotes allows you to quickly add individualized content for each group member, ensuring documentation is both efficient and clinically meaningful.
With ICANotes, you’ll spend less time writing therapy notes and more time supporting your clients. Register for a free 30-day trial account now — no credit card required!
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
- Complete Notes in Minutes - Purpose-built for behavioral health charting
- Always Audit-Ready – Structured documentation that meets payer requirements
- Keep Your Schedule Full – Automated reminders reduce costly no-shows
- Engage Clients Seamlessly – Secure portal for forms, messages, and payments
- HIPAA-Compliant Telehealth built into your workflow
Complete Notes in Minutes – Purpose-built for behavioral health charting
Always Audit-Ready – Structured documentation that meets payer requirements
Keep Your Schedule Full – Automated reminders reduce costly no-shows
Engage Clients Seamlessly – Secure portal for forms, messages, and payments
HIPAA-Compliant Telehealth built into your workflow
Related Posts
Dr. October Boyles is a behavioral health expert and clinical leader with extensive expertise in nursing, compliance, and healthcare operations. With a Doctor of Nursing Practice (DNP) and advanced degrees in nursing, she specializes in evidence-based practices, EHR optimization, and improving outcomes in behavioral health settings. Dr. Boyles is passionate about empowering clinicians with the tools and strategies needed to deliver high-quality, patient-centered care.