Blog > Documentation > Golden Thread Documentation for Mental Health Clinicians
The Golden Thread in Mental Health Documentation: How to Keep Your Clinical Story Seamless and Defensible
Maintaining consistent, high-quality clinical documentation can feel like walking a tightrope between compliance and care. The golden thread helps clinicians stay balanced by connecting every stage of a client’s journey — from intake to discharge — through clear, cohesive documentation. In this guide, you’ll learn what the golden thread in mental health means, why it’s essential for defensible notes, and how ICANotes helps you maintain that thread effortlessly across every assessment, treatment plan, and progress note.
Sharon Miller, LCSW-R, CCM, CDP
Last Updated: October 20, 2025

What You'll Learn
- What the golden thread means in therapy documentation and how it links assessment, treatment, and progress notes.
- Why golden thread documentation is crucial for medical necessity, audits, and clinical outcomes.
- How to create client-centered goals and measurable objectives that strengthen your documentation story.
- Common pitfalls to avoid when writing notes that risk breaking the golden thread.
- Ways ICANotes supports golden thread compliance with built-in templates, AI-powered note drafting, and structured workflows.
What Is the Golden Thread in Mental Health?
The golden thread in mental health refers to the consistent clinical connection between your assessment, treatment plan, and progress notes.
Think of it as the narrative thread that links:
- Assessment: What brings the client to therapy and how you define the problem.
- Treatment Plan: What goals and interventions you’ve collaboratively set to address that problem.
- Progress Notes: How the client responds and progresses toward those goals over time.
When these three components align, your documentation clearly demonstrates why the client needs treatment, how treatment is provided, and what progress has been made — the foundation of clinical defensibility and quality care.
Why Golden Thread Documentation Matters
Failing to maintain the golden thread can have major consequences, both clinical and legal. Sharon Miller, LCSW-R, who presented the webinar Never Miss the Mark: How to Ensure Your Documentation Is A+ 100% of the Time, emphasizes that documentation serves many purposes:
- Supports reimbursement: Insurance payers audit for medical necessity and consistency across the record.
- Protects you legally: In a subpoena or review, well-connected notes show your professional diligence.
- Improves clinical outcomes: When treatment builds logically from assessment, care is more effective.
- Strengthens continuity of care: Other providers can easily follow your client’s therapeutic story.
- Reinforces professionalism: Accurate documentation reflects competence and ethical integrity.
Or as Miller puts it: “If it isn’t documented, it didn’t happen.”
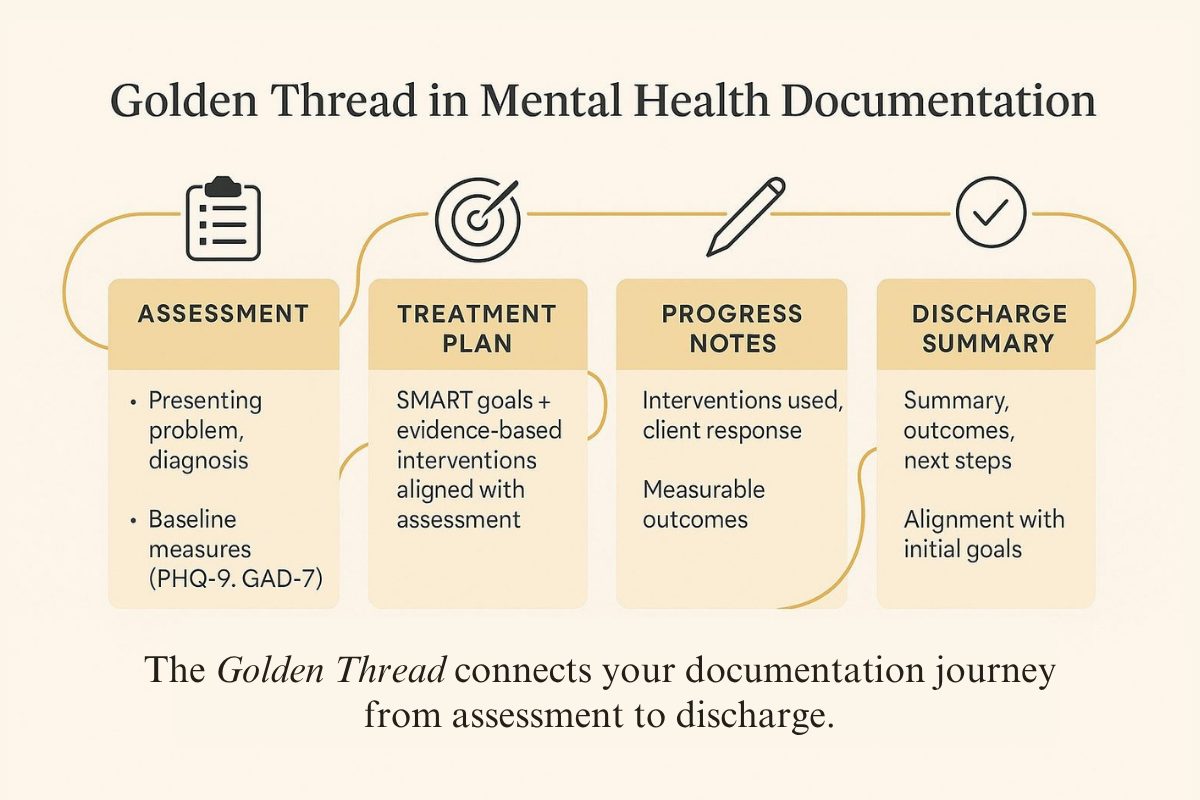
How to Apply the Golden Thread in Therapy Documentation
To maintain a seamless golden thread throughout your clinical notes, every phase of documentation should reflect and reinforce the previous one.
1. Start Strong with a Thorough Assessment
Your assessment is the foundation of the golden thread. It should include:
- The client’s chief complaint or presenting problem.
- Symptoms and diagnosis (including DSM-5 or ICD codes with justification).
- Cultural and psychosocial context that shapes the client’s experience.
- Baseline measures using validated scales like the PHQ-9 or GAD-7.
- Motivational interviewing insights that uncover readiness for change and personal goals.
Your assessment tells the beginning of the story. Every future note should trace back to what you discover here.

Example Assessment:
Client: 36-year-old woman presenting with persistent worry, fatigue, and restlessness interfering with work performance.
Chief Complaint: “I can’t stop overthinking everything. My anxiety makes it hard to concentrate.”
Diagnosis: Generalized Anxiety Disorder (F41.1).
Supporting Evidence: Reports daily anxiety for >6 months, difficulty sleeping, and muscle tension. PHQ-9 = 10 (moderate), GAD-7 = 14 (moderate).
Cultural Considerations: First-generation immigrant balancing family expectations and workplace stress.
Client Goals (Motivational Interviewing): “I want to learn how to calm my mind so I can focus at work and enjoy time with my kids.”
2. Develop a Treatment Plan that Reflects the Assessment
A strong treatment plan transforms the assessment data into actionable goals. Each goal should:
- Be specific, measurable, achievable, relevant, and time-bound (SMART).
- Have corresponding evidence-based interventions (e.g., CBT, DBT, ACT).
- Reflect the client’s own words and aspirations, ensuring person-centered care.
- Include short-term objectives that can be measured and adjusted over time.

Example Treatment Plan:
Goal: Reduce frequency and intensity of panic attacks from daily to once per week within 8 weeks.
Objective: Client will identify and practice three coping strategies (deep breathing, grounding, and thought reframing) to manage anxiety symptoms.
Intervention: Cognitive Behavioral Therapy (CBT) focusing on cognitive restructuring and relaxation training.
Measurement: Self-report and GAD-7 reassessment every four weeks.
3. Use Progress Notes to Connect Every Session Back to the Plan
Your progress notes are where the golden thread becomes visible. Each note should:
- Reference the treatment goal or objective being addressed.
- Describe interventions used and the client’s response.
- Include observable, measurable outcomes (“Client reduced self-reported anxiety from 8/10 to 5/10”).
- Document changes in mental status, safety concerns, and follow-up plans.
Avoid copy-pasting previous notes. Every session has unique nuances that demonstrate your client’s growth and your clinical responsiveness. ICANotes helps by automatically linking progress note content back to the treatment plan, ensuring seamless continuity.

Example Progress Note:
Date: 3/10/2025
Goal Addressed: Reduce daily anxiety and improve concentration at work.
Intervention: CBT session focused on identifying automatic negative thoughts related to performance anxiety. Guided cognitive reframing exercise.
Client Response: Client engaged actively, able to identify three self-critical thought patterns and reframe two with therapist support.
Progress: Reports fewer anxiety spikes during meetings (down from 7/10 to 5/10). Sleep improved from 5 to 7 hours per night.
Plan: Continue weekly CBT sessions. Assign journaling to track thought patterns before next visit.
4. End with a Discharge Summary that Tells the Full Story
When treatment concludes, your discharge note should complete the thread by:
- Restating the presenting problem and initial diagnosis.
- Summarizing goals achieved and interventions used.
- Documenting measurable progress or reasons for discontinuation.
- Providing aftercare recommendations and next steps.
This summary shows how the client’s journey began, what was done, and how the outcomes align with the original plan — proving treatment effectiveness and clinical accountability.

Example Discharge Summary:
Client: Completed 16 sessions of CBT for Generalized Anxiety Disorder.
Initial Presentation: Reported daily anxiety, poor sleep, and difficulty concentrating.
Treatment Summary: Engaged in cognitive restructuring, mindfulness, and grounding exercises.
Goals Achieved: Reduced GAD-7 from 14 to 5. Reports sleeping 7–8 hours nightly and improved work focus.
Remaining Challenges: Occasional mild worry in high-stress situations.
Discharge Plan: Continue mindfulness practice and follow up with primary care for medication evaluation if symptoms recur.
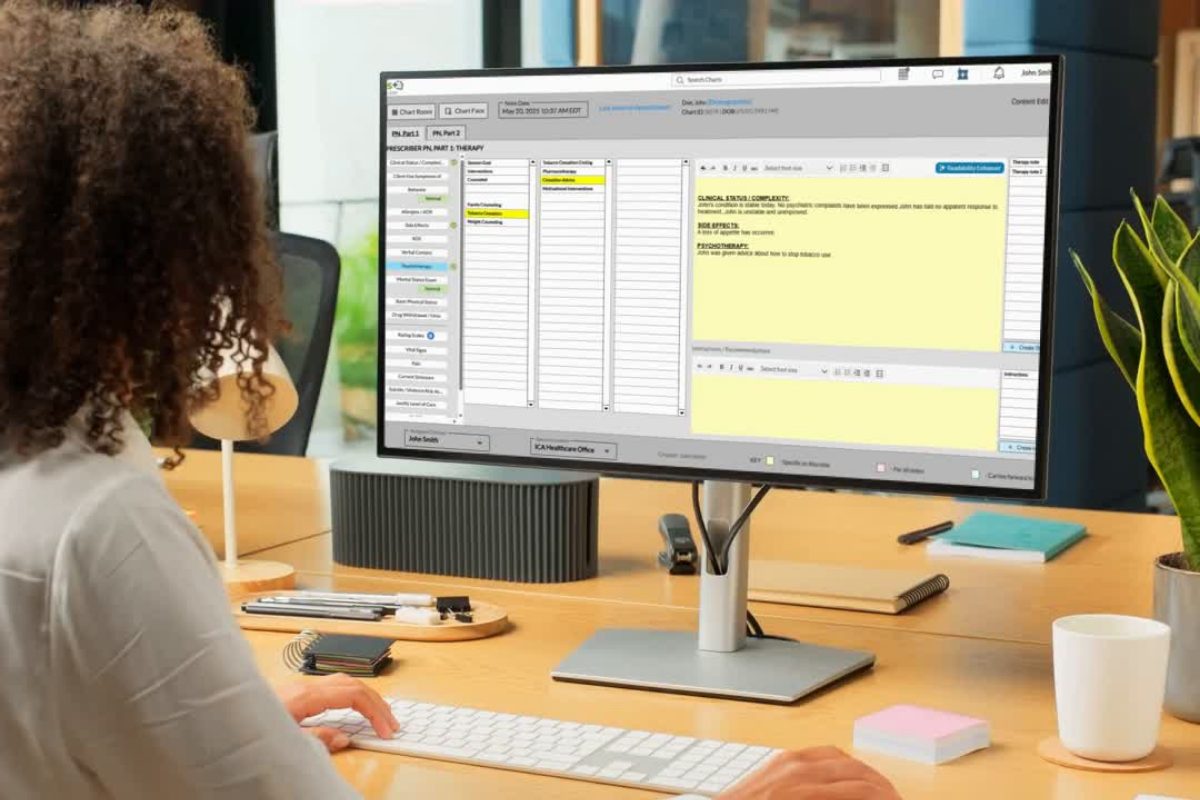
The Role of ICANotes in Supporting Golden Thread Documentation
Maintaining the golden thread can be challenging when juggling full caseloads and compliance standards. ICANotes was designed to make that process effortless.
Here’s how ICANotes helps clinicians create defensible, cohesive, and efficient documentation:
- Built-In Golden Thread Logic: Every assessment, goal, and note is automatically connected for continuity.
- Evidence-Based Templates: Structured prompts guide you to include all medically necessary elements.
- AI Readability Enhancer: Clarifies note language and ensures documentation is client-centered and professional.
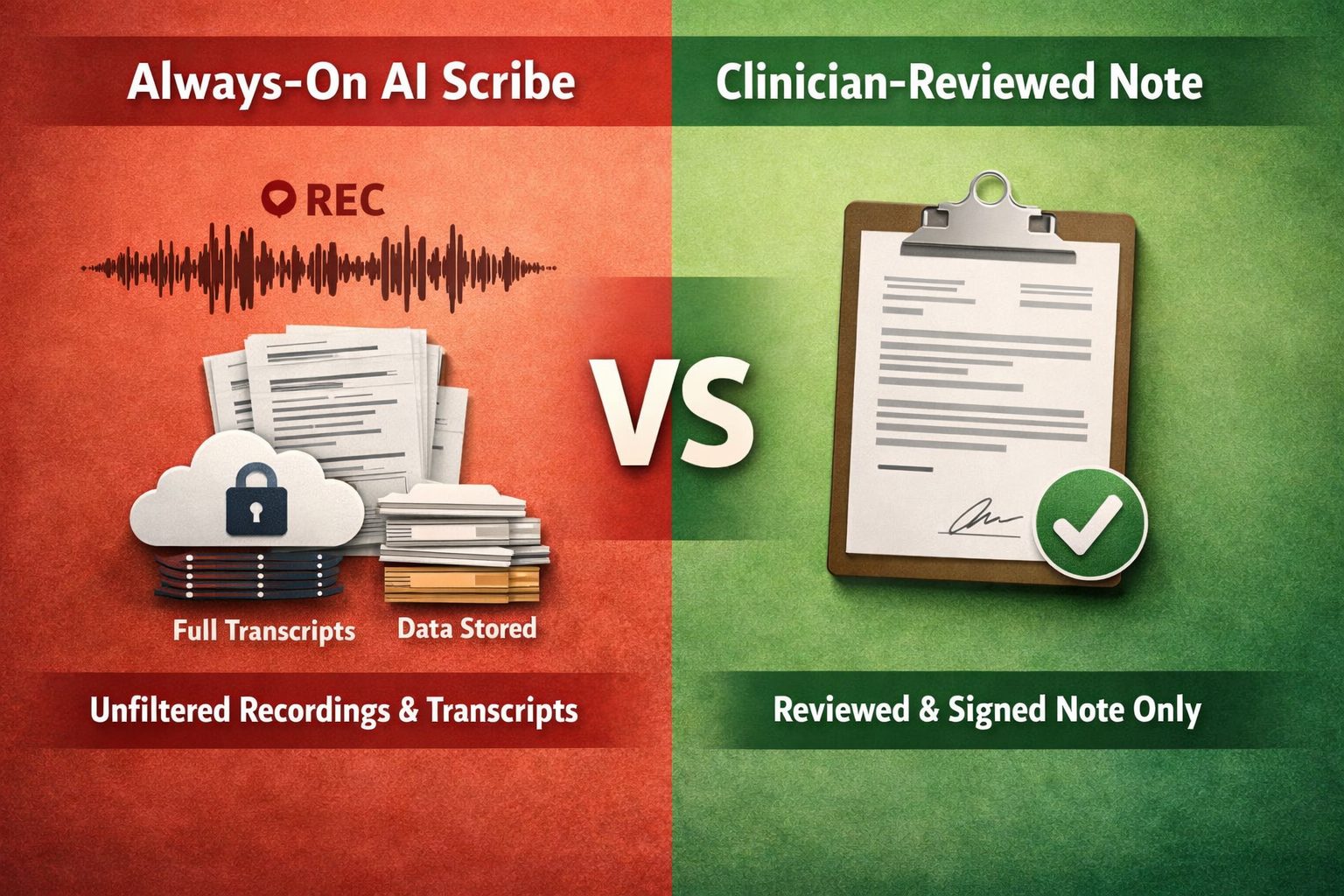
- AI Scribe: Captures session dialogue in real time and drafts clinically accurate progress notes.
- Audit-Ready Formatting: Notes meet payer and compliance standards without extra effort.
- Concurrent Documentation Tools: Reduce the need for copy-pasting and help you complete notes before your next session.
By using ICANotes, clinicians can focus on the therapeutic relationship while ensuring every piece of documentation supports the golden thread, from intake to discharge.
Download Our Guide to Writing Better, Faster Clinical Notes
Streamline your progress notes, avoid documentation pitfalls, and stay compliant with practical templates, note formats (SOAP, DAP, BIRP), and time-saving tips to write high-quality, defensible notes faster.
Key Takeaways for Clinicians
- The golden thread ties your documentation together, proving medical necessity and supporting better outcomes.
- Always connect assessment → treatment plan → progress notes → discharge.
- Keep notes client-centered, measurable, and legally defensible.
- Avoid copy-pasting; tailor each session’s narrative to the client’s progress.
- Use tools like ICANotes to streamline and strengthen your documentation process.
FAQs: Golden Thread Documentation
Final Thoughts
The golden thread isn’t just a compliance requirement, it’s a clinical compass. It ensures your documentation reflects a coherent story of healing and change. With ICANotes, you can maintain that thread effortlessly while elevating the quality, clarity, and compliance of your notes.
Ready to Strengthen Your Golden Thread?
Experience how ICANotes makes documentation seamless, defensible, and stress-free. Start your free trial today!
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
- Complete Notes in Minutes - Purpose-built for behavioral health charting
- Always Audit-Ready – Structured documentation that meets payer requirements
- Keep Your Schedule Full – Automated reminders reduce costly no-shows
- Engage Clients Seamlessly – Secure portal for forms, messages, and payments
- HIPAA-Compliant Telehealth built into your workflow
Complete Notes in Minutes – Purpose-built for behavioral health charting
Always Audit-Ready – Structured documentation that meets payer requirements
Keep Your Schedule Full – Automated reminders reduce costly no-shows
Engage Clients Seamlessly – Secure portal for forms, messages, and payments
HIPAA-Compliant Telehealth built into your workflow
Related Posts
About the Author
Sharon Miller is a licensed clinical social worker and healthcare operations leader with more than 16 years of experience in behavioral health, care management, and telehealth service delivery. She has directed large-scale mental health programs in hospital and digital health settings, developed EHR documentation standards, and trained clinicians in evidence-based practices including CBT, DBT, and motivational interviewing.
As Vice President of Clinical Operations at UCM Digital Health, Sharon led the integration of mental health services into digital care, creating psychosocial assessment, treatment plan, and discharge summary templates that advanced clinical documentation quality. Her work has consistently focused on improving outcomes, compliance, and continuity of care through well-designed workflows and clinician education—principles at the heart of the golden thread concept.
Sharon holds a Master of Social Work from Columbia University, a Master’s in Psychology from New York University, and is a Certified Case Manager and Certified Dementia Planner.