Blog > Treatment Strategies > ACT for Anxiety Disorders: A Practical Guide for Clinicians
Acceptance and Commitment Therapy for Anxiety: A Clinician’s Guide to Building Psychological Flexibility
This article shows how to turn ACT principles into steady, values-driven change your clients can sustain—by building psychological flexibility across the six core processes and applying them in a phase-based session flow from intake through relapse prevention. You’ll see exactly how it sounds in the room via clinician scripts using a running vignette (Jamie) for each ACT process, with practical, brief, billable moves that keep clients moving toward what matters even when anxiety tags along.
Last Updated: August 29, 2025


What You'll Learn
- The ACT six-process model and how it targets anxiety without a “control agenda.”
- Micro-interventions that fit in 2 minutes (drop the rope, clipboard, choice point, struggle switch).
- Assessment with the ACT Matrix plus symptom/process measures.
- Turning values into graded, real-world committed actions (values-anchored exposure).
- How to troubleshoot: “acceptance = giving up,” sticky thoughts, and safety behaviors.
Contents
- Why Acceptance and Commitment Therapy for Anxiety—and Why Now?
- Case Vignette Using ACT for Anxiety Disorders
- Micro-Skills That Make Sessions Flow
- Troubleshooting Common Snags
- Integrating Documentation and Outcomes (ensuring that it’s billable and defensible)
- What Success Looks Like with ACT for Anxiety Disorders
- Conclusion: Making ACT Workable in the Real World—with ICANotes
Why Acceptance and Commitment Therapy for Anxiety—and Why Now?
Clients rarely come to therapy asking to “feel everything more fully.” They want anxiety to stop. ACT asserts that fighting anxiety often makes it stronger (view “The Struggle Switch” video for an illustration of this concept). By helping clients relate differently to internal experiences while guiding them to move towards what matters, ACT expands life even when symptoms ebb and flow. This article weaves the core processes into a clear, clinical flow you can use from intake through discharge, with one running vignette to show how the work looks in practice.
The Clinical Problem Reframed
Anxiety thrives on a control agenda: avoid, analyze, reassure, check. Those short-term relief strategies become “away moves” that shrink life. ACT normalizes this pattern without judgment and introduces a workable alternative: noticing what shows up inside, allowing room for it, and choosing “toward moves” guided by values. How do clinicians help clients create movement in the direction of toward moves? The core principle of ACT that assists with this is psychological flexibility.
Psychological Flexibility in one Picture
Think of psychological flexibility as a clinician’s “north star.” Psychological flexibility is the ability to adapt to changing situations and manage difficult thoughts and feelings effectively, rather than being controlled by them. When a session helps a client (1) contact the present moment, (2) make space for discomfort, (3) defuse from sticky thoughts, (4) stand in the observing self, (5) clarify values, and (6) take committed action, flexibility increases.
Case Vignette Using ACT for Anxiety Disorders
Jamie, 28, reports intense anxiety in social settings—racing heart, catastrophic self-talk (“I’m boring,” “They’re judging me”), and escalating avoidance. Jamie wants friends and professional growth but is “waiting until I’m less anxious” to try. We’ll return to Jamie as we map assessment and treatment.
Assessment That Sets Up Treatment
Map the Pattern, Not Just the Symptoms
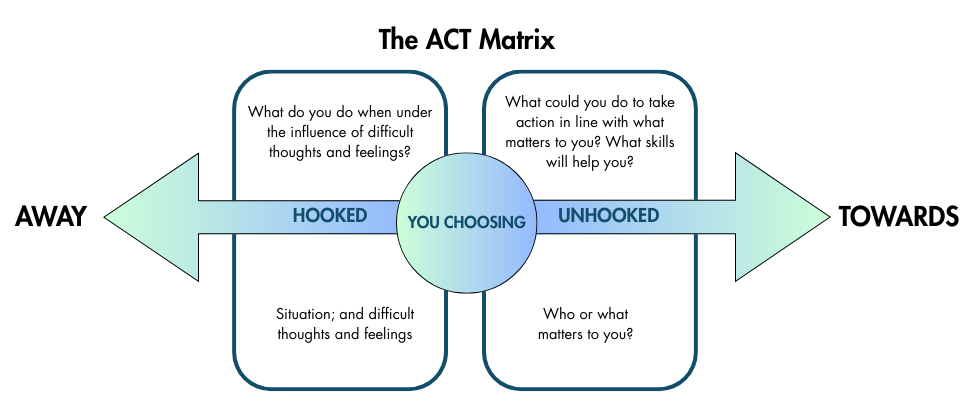
Early sessions focus on function over form: What does anxiety stop you from doing? What do you do next? What does that cost you? The ACT Matrix is ideal to explore at intake:
- Bottom-right (What matters): Connection, learning, reliability
- Bottom-left (Inner stuff): Tight chest, heat, “I’m awkward,” images of blushing
- Top-left (Away moves): Cancel plans, drink to cope, overprepare, scroll at home
- Top-right (Toward moves): Text a coworker, attend a meetup for 20 minutes, ask one curious question
Brief measures (e.g., GAD-7 for symptoms; a psychological flexibility scale for process) give baselines and help you and the client monitor progress. Document the matrix and initial scores and revisit both at key intervals.
A Phase-Based ACT for Anxiety Treatment Arc (with Jamie)
Phase 1: Orient and Steady (Present-Moment + Acceptance)
You normalize the control trap and introduce allowing as a workable alternative to suppression.
- Therapist: “Where is anxiety in your body right now?”
- Jamie: “Tight chest.”
- Therapist: “Let’s make room around that tightness—no fight, no fix—so you can keep choosing what matters.”
This is brief and experiential: 60–90 seconds of breath and sensation labeling sprinkled throughout the hour. The goal is not serenity; it is willingness while engaged.
Phase 2: Unhooking from Language (Defusion)
You help Jamie see thoughts as events, not mandates. Defusion teaches clients to observe thoughts as just thoughts and to mindfully observe them as they are without attachment to them.
- “I’m having the thought that I’m boring.”
- “I notice my mind predicting rejection.”
When a thought “sticks,” one option is to try a 30-second repetition or a playful voice to expose its sound-like-sound quality. Defusion isn’t necessarily debate. If Jamie insists “it’s true,” you explore how that may be so, and ask whether treating it as truth helps advance Jamie’s values right now.
Phase 3: Make Meaning Explicit (Values)
Anxiety is loud because something matters. Anxiety also has a tendency to pull people away from their values and valued-based living.
- Therapist: “If your social life were easier, what kind of person would you be?”
- Jamie: “Present and supportive.”
- Therapist: “Let’s let that steer our experiments.”
With the client, capture 2–3 top values as verbs (be present, be curious, be reliable), then translate them into actionable behaviors.
Phase 4: Let Values Drive Behavior (Committed Action)
In this phase, we build a ladder of steps sized to succeed with anxiety “in your pocket”:
- This week: Send one text invite by Thursday noon; attend a coffee for 10 minutes minimum.
- Willingness cue: “Tight chest can ride along while I ask one curious question.”
- After-action review: What moved you toward/away? What did you learn about what helps?
Behavioral activation and exposure practices are woven in here, while being values-anchored and process-oriented (Did I show up? Did I do my value-consistent behavior with willingness?).
Phase 5: Stabilize Perspective (Self-as-Context)
When anxiety surges, you invite Jamie to become mindful of the part that notices—“sky and weather.” Short exercises (“close your eyes; notice the noticer”) reduce over-identification with strong thoughts, urges, and emotions. Clients often report more room to breathe, literally and figuratively.
Phase 6: Consolidate and Prevent Relapse
Mapping typical choice points (e.g., 30 minutes before an event) and rehearsing a 3-step plan can be helpful: Name it → Make room → Move toward. You refresh the matrix, re-score measures, and celebrate gains in life participation, not just lowered distress or symptoms.

Tip
Defusion teaches clients to observe thoughts as just thoughts and to mindfully observe them as they are without attachment to them.
ACT for Anxiety Micro-Skills That Make Sessions Flow
- Name–Acknowledge–Allow–Choose: “Name what is here (‘tight chest’), acknowledge the urge to avoid, allow 2–3 breaths of space, choose a tiny toward move.”
- Drop the rope: If Jamie is wrestling with “I’ll say something dumb,” enact a tug-of-war and invite dropping the rope. The thought remains; struggling eases; choice returns.
- Clipboard metaphor: Invite the client to hold a pad in front of their face (fusion), then place it beside or beside them (defusion). The “problem” doesn’t vanish; the view enlarges and there is more space and focus for things in life that really matter to the client.
Troubleshooting Common Snags with ACT
- “Acceptance means giving up.” Reframe acceptance as the cost of admission to a valued life, not resignation. Demonstrate this with a 60-second “push the beach ball under water” experiment and ask which approach preserves energy for action.
- “Prove this will work.” Offer a behavioral bet: one tiny experiment, tracked in writing, judged by the client’s values rather than your persuasion.
- Safety behaviors creeping into exposures. Treat them as away moves; gently test doing 5% less safety while doing 5% more value (e.g., one question asked without rehearsing).
Integrating Documentation and Outcomes (ensuring that it’s billable and defensible)
Write notes that highlight function and change processes:
- Assessment: Anxiety pattern (physiology, cognitions, avoidance), matrix summary, baseline measures.
- Interventions: “Introduced present-moment awareness and acceptance; practiced defusion (‘I’m having the thought…’); clarified values (connection); planned one committed action.”
- Response: “Client enacted toward move; tolerated SUDS 6/10 with willingness; reported pride and energy afterward.”
- Plan: Next step on ladder; measures to recheck; risk updates if relevant.
If you use ICANotes, this language maps cleanly to progress note buttons and custom phrases, links directly to a values-based treatment plan, and pairs with outcome tracking (e.g., GAD-7 trendlines) to support medical necessity and prior authorization.
What Success Looks Like with ACT for Anxiety Disorders
Jamie still notices a quickened pulse at crowded events but now texts a peer, asks one curious question, and leaves by choice rather than panic. Anxiety hasn’t been “cured”; life has gotten bigger. That’s ACT’s aim, and its promise.
Cultural Humility and Accessibility
Values are client-defined, not clinician-prescribed. Honor culturally bound views of courage, family, spirituality, and help-seeking. Keep metaphors flexible (some clients prefer concrete demos; others resonate with narrative story). Pace willingness work carefully with trauma histories; consent and collaboration are non-negotiable.
Frequently Asked Questions
Conclusion: Making ACT Workable in the Real World—with ICANotes
ACT widens life even when anxiety stays noisy. The day-to-day challenge isn’t just what to do, it’s documenting how you did it, linking it to goals, and showing progress over time. That’s where ICANotes helps you turn ACT into a consistent, compliant workflow:
- ACT-aligned notes in minutes. Use (or create) custom buttons/phrases for acceptance practice, cognitive defusion, self-as-context, values clarification, and committed action, so progress notes reflect ACT language without typing from scratch. Randomized phrasing keeps documentation natural.
- Treatment plans that map to values. Tie goals like “Increase psychological flexibility for social participation” to specific ACT interventions and measurable objectives; link each session’s note to those goals—especially useful for Medicaid/Medicare and prior authorizations.
- Outcomes + process tracking. Enter scales (e.g., GAD-7/PHQ-9) and track trends alongside ACT process targets (toward/away moves, exposure steps completed). Graphs support medical necessity and show value-driven behavior change, not just symptom shifts.
- Client portal for ACT homework. Send intake packets, assessments, and ACT worksheets (e.g., Matrix, values sort, “Name the Story”) through the portal; collect them before session so therapy time stays focused on practice and planning.
- Session flow captured accurately. Optional ambient listening AI scribe helps draft session summaries; you edit to highlight the choice point addressed, willingness work attempted, the defusion method used, and the one tiny step committed for the week.
- Audit-ready details without friction. Simple clicks document MSE, risk checks, time spent, CPT, and medical-necessity statements (e.g., functional impairment + rationale for continued care), keeping your ACT work payer-friendly.
- Scheduling and adherence. Calendar integration and reminders reduce missed exposures/assignments; note templates prompt a quick “after-action review” to reinforce learning and refine the next step.
If you want your ACT treatment for anxiety disorders to be easier to run, faster to document, and simpler to defend, book an ICANotes demo—and let your software do the busywork while you focus on building psychological flexibility.
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
- Complete Notes in Minutes - Purpose-built for behavioral health charting
- Always Audit-Ready – Structured documentation that meets payer requirements
- Keep Your Schedule Full – Automated reminders reduce costly no-shows
- Engage Clients Seamlessly – Secure portal for forms, messages, and payments
- HIPAA-Compliant Telehealth built into your workflow
Complete Notes in Minutes – Purpose-built for behavioral health charting
Always Audit-Ready – Structured documentation that meets payer requirements
Keep Your Schedule Full – Automated reminders reduce costly no-shows
Engage Clients Seamlessly – Secure portal for forms, messages, and payments
HIPAA-Compliant Telehealth built into your workflow
Related Posts
Diane Bigler, LCSW, LSCSW, is a Licensed Clinical Social Worker in Missouri and Kansas with over 25 years of experience in the mental health field. She has held clinical positions as an outpatient and in-home therapist and clinical supervisor in diverse settings. Diane was an Adjunct Professor of Social Work for 10 years at The University of Kansas, School of Social Welfare and a Field Liaison and Field Instructor. She has also held administrative positions as a Program Director and Coordinator. Diane is a popular local and national trainer on a wide variety of mental health and workplace development topics for clinicians and corporations and has facilitated over 500 training courses in the last few years. Diane is most passionate about providing quality professional development to clinicians, employees, and leaders.








