Blog > Billing & Insurance > Complete Guide to Mental Health & Behavioral Health Billing
Complete Guide to Mental Health & Behavioral Health Billing
If you're looking to optimize your mental health billing or streamline billing for behavioral health services, this guide is for you. Mental health billing is often complex and time-consuming, with coding errors, documentation issues, and insurance hurdles getting in the way of patient care. This guide breaks down everything clinicians need to simplify behavioral health billing, reduce claim denials, and get paid faster—so they can spend more time helping clients and less time chasing payments.

Fatima Davis
Last Updated: July 17, 2025


What You'll Learn
- The most common billing pitfalls in mental health practices—and how to avoid them
- How to properly use diagnosis and CPT codes to ensure faster reimbursements
- Step-by-step tips to verify insurance, submit clean claims, and reduce denials
- When and how to outsource behavioral health billing to save time and improve cash flow
Contents
- Types of Covered Mental Health Services
- The Role of Medical Record Documentation in Behavioral Health Billing
- Diagnosis Coding for Mental Health Billing
- Why Mental Health Billing Can Be Complicated
- Common Challenges When Billing for Mental Health Services
- Tips for Mental Health & Behavioral Health Billing Success
- Understanding CPT Codes and Maximizing Reimbursement
- How ICANotes Can Help You With Billing for Mental Health Services
Mental and behavioral health services are vital to emotional well-being, recovery, and overall quality of life. These services span a wide range of therapeutic interventions and clinical settings, from individual therapy and psychiatric evaluations to group counseling and medication management. Yet despite their importance, billing for behavioral health services is often one of the most challenging and time-consuming aspects of running a practice.
From coding errors and documentation gaps to authorization delays and claim denials, mental health billing can quickly become a barrier to care and operational efficiency. Navigating this complex landscape requires both administrative precision and a solid understanding of payer expectations. This guide is designed to demystify the process—so you can spend less time managing paperwork and more time focused on your clients.
Types of Covered Mental Health Services
When billing for mental health services, it’s essential to understand which types of care are typically reimbursable by insurance providers. Covered services vary by payer and plan but generally fall into several key categories recognized across behavioral health billing guidelines:
1. Psychiatric Evaluation and Diagnostic Services
Initial assessments to determine a diagnosis and treatment plan are usually covered. These include structured diagnostic interviews and evaluations performed by psychiatrists, psychologists, or licensed mental health professionals.
2. Psychotherapy
Individual, group, and family therapy sessions are among the most commonly billed mental health services. Coverage often depends on provider licensure, session length, and medical necessity. Common CPT codes include 90832, 90834, and 90837.
3. Medication Management
For clients receiving psychotropic medications, services provided by psychiatrists or psychiatric nurse practitioners for medication evaluation, prescription, and monitoring are typically reimbursable.
4. Crisis Intervention
Many insurance plans cover urgent mental health care such as suicide risk assessments, safety planning, and acute crisis stabilization—especially when performed in outpatient or emergency settings.
5. Telehealth Services
Telepsychiatry and virtual therapy became more broadly covered during the COVID-19 pandemic and continue to be billable under most plans when services meet licensing and HIPAA-compliant delivery standards.
6. Substance Use Disorder (SUD) Treatment
Detoxification, outpatient SUD counseling, and dual diagnosis treatment are often covered as part of behavioral health benefits, although authorization requirements and limitations may vary.
7. Behavioral Health Integration Services
Some payers reimburse for coordinated care models like the Collaborative Care Model (CoCM), where behavioral health services are integrated into primary care using a team-based approach.

Documentation Tip
For each of these covered services, accurate documentation that supports medical necessity, CPT/ICD code selection, and progress over time is essential for clean claims and timely reimbursement.
Free 2026 Billing Guide for Mental Health Providers
Clean claims. Correct coding. Fewer denials.
This comprehensive guide breaks down everything you need to bill accurately, reduce denials, and protect your revenue. Download your copy and get the tools you need to streamline billing and boost reimbursement.
The Role of Medical Record Documentation in Behavioral Health Billing
Accurate and thorough documentation is the backbone of successful behavioral health billing. Medical records not only support the clinical care you provide but also serve as the legal and financial justification for reimbursement.
Payers require detailed documentation to verify that billed services were medically necessary, appropriately coded, and delivered by a qualified provider. Incomplete or vague records are a leading cause of claim denials and payment delays in mental health billing.
Key elements your mental health documentation should include:
-
Diagnosis and clinical rationale: Clear justification for treatment based on the client’s presenting symptoms and functional impairments.
-
Progress notes linked to treatment goals: Each session note should reflect progress, or lack thereof, toward documented treatment objectives.
-
Service codes supported by content: Ensure the level of service billed (e.g., 90834 vs. 90837) is justified by the note’s time, complexity, and interventions provided.
-
Medical necessity language: Payers look for evidence that the service was essential for the client’s mental health condition and not primarily for convenience or personal development.
Inadequate documentation increases audit risk, delays payments, and can ultimately compromise compliance. For behavioral health practices, establishing consistent documentation workflows is key to sustainable billing operations.
Tip for Clinicians:
Use EHR clinical note templates designed for mental health to streamline documentation while ensuring you meet billing requirements. Smart prompts and structured note formats help reduce omissions and improve claim acceptance rates.
Diagnosis Coding for Billing Mental Health Services
Accurate diagnosis coding is a critical part of behavioral health billing. Insurers use diagnosis codes to determine whether a service is medically necessary and reimbursable. Using outdated, incomplete, or non-specific codes can lead to claim denials, payment delays, and compliance risks.
Behavioral health providers must use ICD-10-CM codes to document a client’s diagnosis. These codes should reflect the primary condition being treated and align with the treatment goals and services provided.
Best Practices for Diagnosis Coding:
-
Code to the highest level of specificity. Avoid generic codes when more detailed options are available. For example, use F33.1 – Major depressive disorder, recurrent, moderate instead of just F33.9 – Major depressive disorder, unspecified.
-
Support diagnoses with documentation. The diagnosis listed on the claim must match the one documented in your clinical notes. Include enough clinical detail to justify the diagnosis and treatment plan.
-
Keep up with annual updates. ICD-10 codes are updated every October. Regularly reviewing coding changes helps avoid rejections due to obsolete codes.
-
Avoid “rule-out” and suspected conditions. Payers generally don’t reimburse based on provisional or suspected diagnoses—only confirmed mental health conditions that meet criteria for treatment.
Common ICD-10 Codes in Mental Health Billing:
-
F32.0 – Major depressive disorder, single episode, mild
-
F41.1 – Generalized anxiety disorder
-
F43.10 – Post-traumatic stress disorder, unspecified
-
F90.0 – Attention-deficit hyperactivity disorder, inattentive type
-
F11.20 – Opioid dependence, uncomplicated

Why It Matters
Using the correct diagnosis code not only helps get claims paid but also protects your practice during audits and utilization reviews. In behavioral health billing, clinical accuracy and coding precision go hand in hand.
Why Mental Health Billing Can Be Complicated
Billing for mental health services presents unique challenges that differ significantly from medical billing. From varying session lengths and provider credentials to evolving payer policies and preauthorization requirements, behavioral health billing is often more complex and time-consuming.
Key Reasons Mental Health Billing is More Complicated:
1. Variable Coverage Across Payers
Insurance plans differ widely in how they cover mental health services. Some limit the number of sessions per year, require prior authorization, or exclude specific providers or diagnoses from coverage.
2. Strict Medical Necessity Requirements
Payers scrutinize mental health claims closely to ensure services are medically necessary. This requires detailed documentation and diagnosis coding to support the claim, a frequent source of denials when not done correctly.
3. Frequent Policy Changes
Mental health parity laws, telehealth expansions, and state-specific regulations change often. Staying compliant requires constant monitoring of policy updates across payers and jurisdictions.
4. Multiple Service Types and Codes
Therapists, psychiatrists, and other behavioral health providers may bill for different service types (e.g., psychotherapy, assessments, medication management), each with its own CPT codes and documentation standards. Mistakes in code selection or time-based billing can result in claim rejections.
5. Credentialing and Supervision Issues
Billing for services provided by interns, residents, or associate-level clinicians often involves additional supervision and credentialing documentation. Not all payers reimburse services provided under supervision, and billing incorrectly can trigger audits.

Bottom Line
Mental health billing requires specialized knowledge and tools to reduce denials, speed up reimbursement, and maintain compliance. Investing in behavioral health billing expertise, whether through staff training, specialized software, or outsourced services, can significantly reduce administrative burden and improve financial performance.
Common Challenges When Billing for Mental Health Services
Even experienced clinicians and billing teams can run into obstacles when managing billing for mental health services. From administrative bottlenecks to payer-specific rules, these challenges can slow down reimbursement, increase claim denials, and drain valuable time from patient care.
1. Inconsistent Coverage Across Insurers
Mental health parity laws have improved access, but insurance companies still vary widely in how they cover behavioral health services. Some require preauthorization for therapy, others limit session frequency, and many restrict coverage based on diagnosis or provider type.
2. High Denial Rates Due to Documentation Issues
One of the most common pain points in behavioral health billing is denied claims caused by insufficient documentation. Missing clinical details, lack of medical necessity language, or mismatched diagnosis and CPT codes can all trigger a rejection.
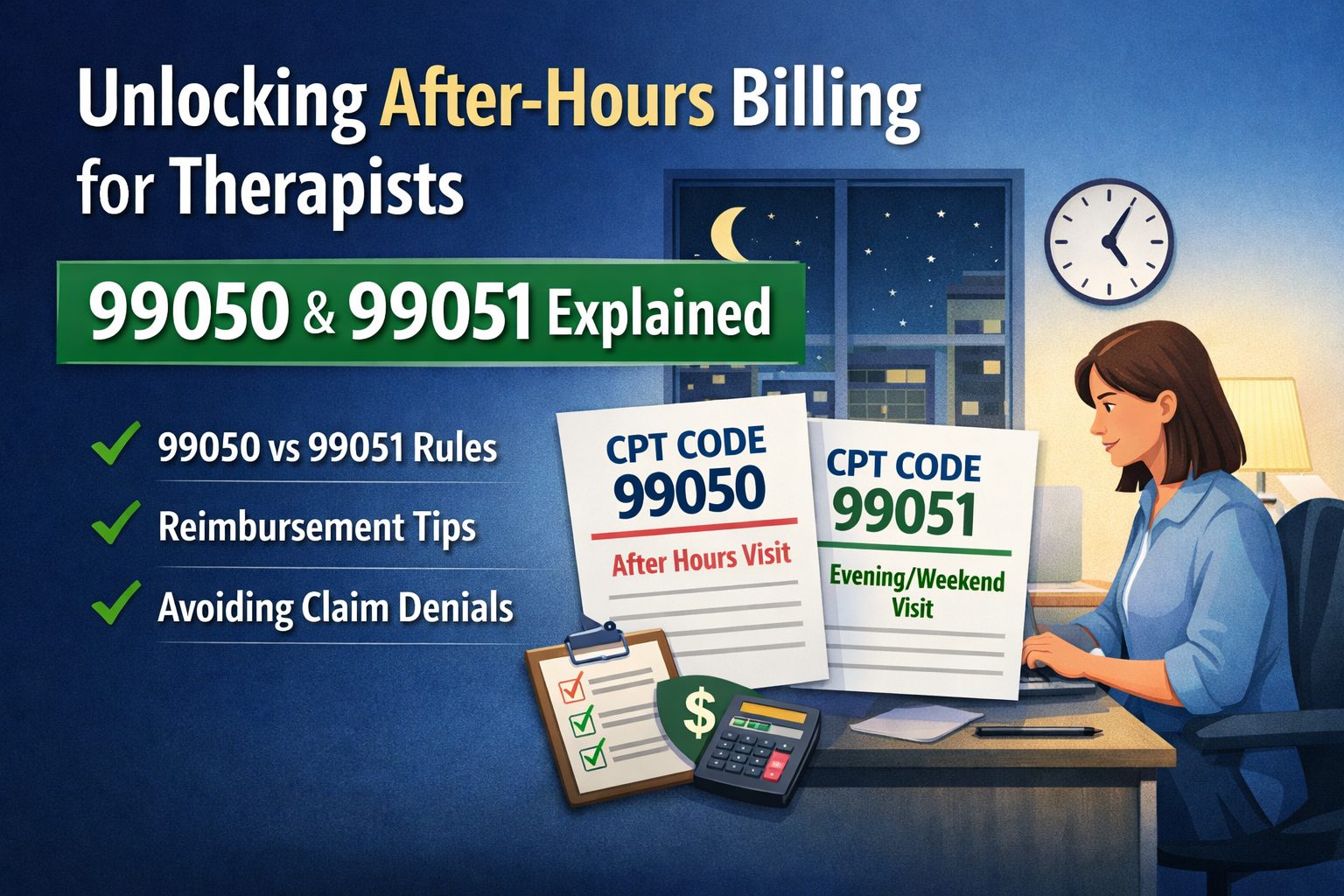
3. Time-Based CPT Code Complexity
Psychotherapy codes are time-based, and small discrepancies between billed time and documented time can result in claim denials. Providers must be meticulous about aligning session lengths with the appropriate CPT code (e.g., 90832 vs. 90834 vs. 90837).
4. Credentialing and Supervision Restrictions
Insurance payers often have strict credentialing requirements. Services provided by interns, associate-level clinicians, or uncredentialed staff may not be reimbursable—or must be billed under a supervising provider with proper documentation.
5. Delayed Payments and Follow-Ups
Without a robust billing system, it’s easy to lose track of outstanding claims. Manual processes, slow payer responses, and limited staff resources can all lead to cash flow delays and unpaid services.
6. Telehealth Billing Confusion
While telehealth is widely accepted, billing rules for virtual sessions still vary by payer. Providers must ensure they’re using the correct place of service codes, modifiers, and documentation to meet reimbursement criteria.
Tips for Mental Health & Behavioral Health Billing Success
Effective billing for mental health services requires more than just submitting claims—it demands accuracy, consistency, and a deep understanding of payer expectations. Use these practical tips to avoid common pitfalls and improve your behavioral health billing outcomes.
1. Verify Insurance Benefits Up Front
Before the first appointment, confirm the client’s mental health coverage, copays, session limits, deductible status, and preauthorization requirements. This prevents surprises and ensures you’re billing within the scope of the client’s benefits.
2. Use the Correct CPT and ICD-10 Codes
Choose service and diagnosis codes that reflect what actually occurred during the session. For example, if you provide a 60-minute individual therapy session, use CPT code 90837, and ensure your documentation supports both the time and clinical complexity.
3. Document Medical Necessity Clearly
Payers require that services be medically necessary for reimbursement. Your progress notes should include evidence of a mental health diagnosis, describe symptom impact on functioning, and show how your interventions address the treatment plan goals.
4. Track Authorization Requirements and Limits
Many payers require preauthorization for psychological testing, extended sessions, or intensive services. Use a calendar or EHR alerts to track authorization dates and visit limits to avoid claim rejections or missed revenue. If you are using a behavioral health EHR like ICANotes, the managed care authorization tracking feature can be configured to notify you when additional authorizations are needed.
5. Submit Claims Promptly and Accurately
Timely claim submission improves cash flow and reduces the risk of timely filing denials. Double-check for common errors such as incorrect NPI, provider credentials, place of service codes, and client demographic mismatches. If you are using an EHR or clearinghouse, those systems can pre-scrub your claims to minimize rejections.
6. Follow Up on Unpaid Claims
Don’t assume silence means approval. Set a routine to check claim statuses, resubmit denied claims with corrections, and appeal when needed. A solid follow-up process can significantly increase your reimbursement rate.
7. Use Software Designed for Behavioral Health
A behavioral health-specific EHR can simplify everything from note-taking to code selection, authorization tracking, and integrated billing. Systems built specifically for behavioral health reduce administrative burden and help ensure compliance with mental health billing regulations.

Pro Tip
Keep a cheat sheet of your most-used CPT and ICD-10 codes and payer-specific billing rules. Quick reference tools reduce errors and help your team work more efficiently.
Understanding CPT Codes and Maximizing Reimbursement
To bill accurately and get paid appropriately for mental health services, clinicians must have a clear grasp of Current Procedural Terminology (CPT) codes. These codes describe the services you provide, such as therapy sessions, diagnostic evaluations, and medication management, and directly determine how much you’re reimbursed.
Using the correct CPT code is about more than compliance. It’s essential for:
-
Receiving full reimbursement for your time and expertise
-
Avoiding underbilling or overbilling that could trigger denials or audits
-
Demonstrating medical necessity through appropriate code-documentation alignment
Common CPT Codes for Mental Health Services:
-
90791 – Psychiatric diagnostic evaluation
-
90832 – Psychotherapy, 30 minutes with patient
-
90834 – Psychotherapy, 45 minutes with patient
-
90837 – Psychotherapy, 60 minutes with patient
-
90846/90847 – Family or couples therapy (without/with the patient present)
-
99213/99214 – Evaluation and management (for medication management visits)
When choosing a code, match it carefully to the session’s length, content, and provider type. For example, a 60-minute session using advanced clinical techniques should typically be coded as 90837—provided the documentation justifies it. Underbilling by choosing 90834 instead could leave significant revenue on the table.
Understanding CPT codes is foundational to mental health billing success. With the right training and tools, you can reduce denials, ensure compliance, and optimize your financial outcomes—without spending extra hours on paperwork.

Reimbursement Tip
Want to make sure you’re getting paid what you deserve for the services you provide? Read our in-depth guide on how to maximize your reimbursement rate for proven strategies, including modifier usage, claim timing, and payer negotiation tactics.
Know When to Outsource Mental Health Billing Services
Managing billing in-house can be time-consuming and frustrating, especially for busy behavioral health practices navigating complex payer requirements, denied claims, and shifting regulations. Outsourcing your mental health billing to a trusted partner can help reduce administrative burden, improve claim turnaround times, and increase revenue.
ICANotes offers full-service behavioral health Revenue Cycle Management (RCM) to support your practice every step of the way — from eligibility verification to payment posting. Our dedicated RCM team brings deep expertise in behavioral health billing and works proactively to minimize denials, shorten reimbursement cycles, and maximize collections. Whether you're a solo practitioner or a growing group practice, outsourcing to ICANotes RCM allows you to stay focused on client care while we handle the complexities of your revenue cycle.
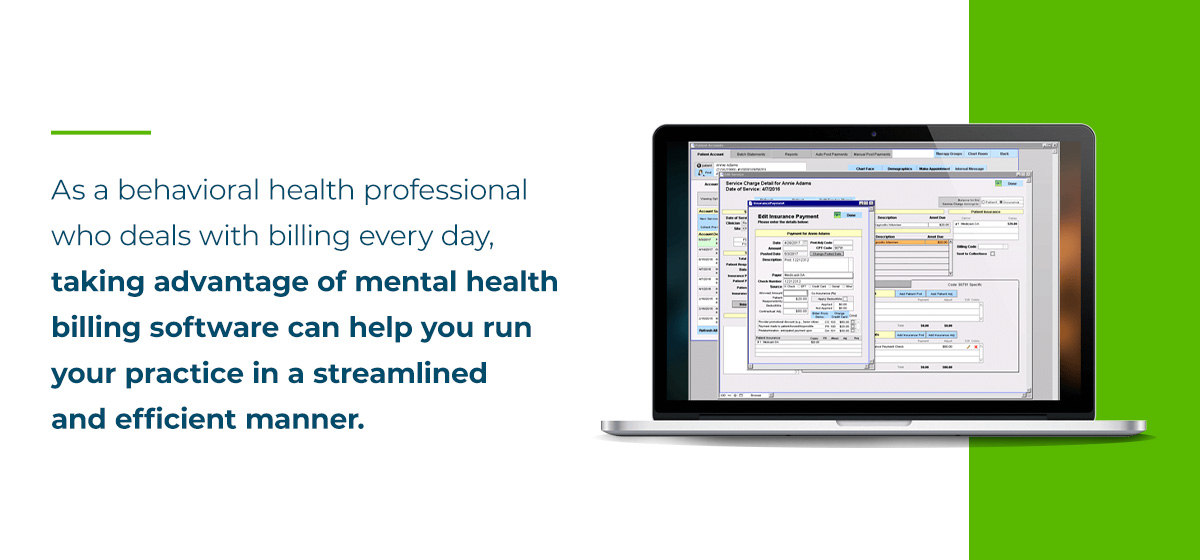
How ICANotes Can Help You with Billing for Mental Health Services
ICANotes provides two powerful options to streamline and strengthen your behavioral health billing process: an all-in-one EHR with integrated billing tools, and a full-service RCM solution.
If your practice handles billing in-house, the ICANotes platform includes robust billing features designed specifically for behavioral health. You can generate CMS-1500 and UB-04 claims directly from your clinical notes, manage payer rules, track authorizations, and stay on top of claim statuses through seamless integration with clearinghouses. Built-in appointment and eligibility tools help reduce billing errors at the front end, while customizable reports offer insight into reimbursements and financial performance.
Prefer to leave billing to the experts? ICANotes also offers outsourced billing services, giving you access to a team of behavioral health billing professionals who manage claims from submission through payment. We stay current with payer policies, follow up on rejections, and provide detailed reporting, so you have visibility without the hassle. Our RCM services are designed to increase revenue, reduce denials, and save valuable time — all with the support of a team that understands the unique needs of mental health providers. Call us at 443-347-0990 for more information or to schedule an RCM Consult.
Frequently Asked Questions
Schedule a Live Demo
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals—built to streamline documentation, improve compliance, and enhance patient care.
- Simplify clinical charting
- Stay organized with appointment scheduling
- Reduce no-shows with automated reminders
- Improve client engagement with a secure patient portal
- Provide flexible care with HIPAA-compliant telehealth
Simplify clinical charting
Stay organized with appointment scheduling
Reduce no-shows with automated reminders
Improve client engagement with a secure patient portal
Provide flexible care with HIPAA-compliant telehealth
Fatima C. Davis is the RCM Manager at ICANotes and a seasoned expert in behavioral health revenue cycle management. With over 20 years of experience, she specializes in optimizing collections, reducing denials, and ensuring compliance across diverse payer landscapes. Fatima has led RCM operations for large multi-agency systems and is passionate about helping behavioral health practices achieve financial sustainability.