Blog > Billing & Insurance > Best Clearinghouse for Medical Billing (Behavioral Health)
How to Choose a Mental Health Clearinghouse (That Actually Fits)

Last Updated: August 22, 2025


What You'll Learn
-
What a clearinghouse actually does for mental health billing (837 out, 835 back).
-
How to evaluate and score vendors to find the best clearinghouse for medical billing.
-
The must-have features for a mental health clearinghouse (behavioral-health edits, payer connectivity, 835 reassociation).
-
Questions to ask before you sign, plus common reject/deny pitfalls and how to prevent them.
Contents
- What Does a Clearinghouse Do in Behavioral Health?
- How to Determine if Your Practice Needs a Clearinghouse
- How to Pick the Best Clearinghouse for Medical Billing (for Mental Health)
- Mental Health Clearinghouse Must Haves
- Questions to Ask Before You Sign
- Why an Integrated EHR + Clearinghouse Beats a Standalone Vendor
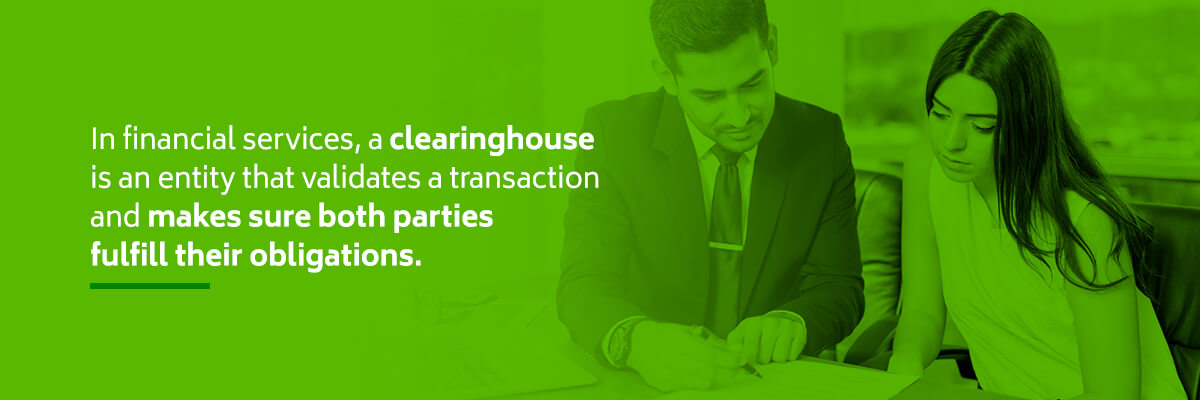
What Does a Clearinghouse Do in Behavioral Health?
Although you can submit claims to your payers directly, working with a medical clearinghouse has multiple advantages. The primary benefit of using a clearinghouse is receiving payments faster. Ideally, the clearinghouse your practice chooses will work with the insurance companies you bill most often to streamline the claim submission and payment process.
In simple terms, a clearinghouse is the traffic controller between your EHR and payers. You generate an 837 electronic claim; the clearinghouse “scrubs” it for errors and forwards it to the payer. When the payer responds with an 835 (remittance advice/payment), your system matches it back to the claim for posting and reconciliation. Clean 837s + reliable 835 reassociation = fewer delays, fewer write-offs, and better cash flow.
How to Determine if Your Practice Needs a Clearinghouse
Not every provider needs to work with a clearinghouse. If you don't work with payers or only have a small number of patients, you might not need to partner with a clearinghouse. If you don't currently work with one and are wondering if doing so will benefit your practice, there are a few questions you can ask:
- How many insurance companies do you work with? If your practice accepts multiple insurance plans, working with a clearinghouse can simplify your claims submission process and increase compatibility.
- Do you have a high volume of claims? If most of your patients use insurance or if you have a lot of patients, a clearinghouse can make your submission process more efficient. If you have a smaller claim volume, it might not make economic sense to use a clearinghouse.
- Do you bill electronically? Clearinghouses work with electronic billing and record-keeping programs for a streamlined process.
- Are claim errors an issue at your practice? Mistakes happen. If they seem to happen frequently at your practice, particularly with claims, a clearinghouse can help to prevent errors that lead to claim denials and rejections. Minimizing errors also means your team can spend less time on hold with payers.
- How long do you typically wait for reimbursement? If you usually wait weeks for insurance reimbursement, the waiting period can affect your bottom line and make it difficult for your practice to pay bills. If you're tired of long waits or can't afford to wait a long time for a payer to reimburse you, a clearinghouse might be the way to go.
How to Pick the Best Clearinghouse for Medical Billing (for Mental Health)
Commercial “best” lists rarely account for the realities of behavioral health. Use these criteria to separate marketing from must-haves:
-
Behavioral-health scrubbing rules
Edits tuned for psychotherapy codes and common modifiers; support for secondary claims/COB and place-of-service logic. -
Payer connectivity you actually need
Confirm your top 10–15 payers (Medicaid, Medicare, commercial, regional MCOs). Fewer “secondary hops” means faster, cleaner routing. -
ERA/EFT & 835 reassociation quality
Look for clean pairing of 835s to original claims and tools to resolve exceptions quickly (no “orphaned” payments). -
Uptime, redundancy, and incident response
Ask how claims flow during major network disruptions and how fast they fail over. Request real incident write-ups and SLAs. -
Support & escalation paths
Hours, channels (phone/email/chat), response targets, and whether you get a dedicated rep during onboarding. -
Accreditation & security
Preference for programs now administered by DirectTrust (formerly EHNAC). This signals mature privacy/security and transaction controls. -
Pricing clarity
Understand per-claim fees, eligibility checks, enrollment costs, and overage tiers. Avoid surprises on secondary claims and attachments. -
EHR compatibility & workflow fit
Single sign-on, status dashboards, resubmission loops, task queues, and how eligibility (270/271) and claim status (276/277) surface inside your EHR.
Scorecard: Compare Clearinghouses by What Matters
Use this comparison matrix to evaluate the clearinghouse vendors you are considering for your practice.
| Criterion | Why it matters | Weight | Vendor A | Vendor B | Vendor C |
|---|---|---|---|---|---|
| Behavioral-health edits/scrubbing | Prevents specialty-specific rejects; supports psychotherapy modifiers. | 30 | |||
| Payer connectivity (your top plans) | Fewer hops/secondary clearinghouses; faster cash. | 20 | |||
| ERA/EFT & 835 reassociation | Accurate posting & reconciliation; fewer write-offs. | 15 | |||
| Uptime & incident response | Keeps claims moving during outages. | 15 | |||
| Support SLAs | Fast answers on rejects; clear escalation. | 10 | |||
| Accreditation (DirectTrust/EHNAC) | Signals security, privacy, process maturity. | 10 |
Mental Health Clearinghouse Must Haves
A true mental health clearinghouse should deliver the essentials below to prevent specialty-specific rejections and speed clean reimbursement.
-
Behavioral-health edit sets that catch diagnosis/procedure mismatches and psych-specific modifier issues before payer submission.
-
Eligibility (270/271) and claim status (276/277) surfaced right in your EHR so staff don’t context-switch.
-
Secondary/COB workflows that retain primary EOB logic and avoid duplicate denials.
-
Robust 835 posting—clean reassociation, easy exception handling, and reports that match your bank deposits.
-
Transparent payer lists for your state/region plus national payers you bill the most.
-
Security & accreditation appropriate for PHI and transaction volume.
Questions to Ask Before You Sign
Ask the questions below to verify you’re choosing the best clearinghouse for medical billing—one that matches your payer mix, workflow, uptime needs, and total cost.
-
Which of our top 10 payers are direct connections vs. routed through another clearinghouse?
-
Average time from 837 submission to payer acceptance? Average time from payer payment to 835 availability?
-
What’s your incident response during industry-wide disruptions? (Ask for actual post-mortems and uptime history.)
-
Do you provide a 30-day proof-of-concept with real claims? What’s the onboarding timeline for ERA/EFT enrollments?
-
How are fees structured (per-claim, eligibility, enrollments, secondaries, attachments)? Any minimums?
-
What are your support SLAs and escalation paths?
Clearinghouse Rejections vs. Payer Denials (and How a Clearinghouse Helps)
Understanding the difference, summarized below, helps you fix errors earlier (rejections) and appeal smarter (denials) so fewer claims stall in your revenue cycle.
-
Rejections happen before the payer gets the claim, usually fixable data or format issues caught during scrubbing.
-
Denials come after the payer reviews a claim—often coverage, auth, or policy reasons.
For a deeper dive into differences, causes, and prevention, read our related article, Clearinghouse Rejection vs. Payer Denial.
ICANotes + Clearinghouses: How Integration Speeds Cash Flow
ICANotes offers a fully integrated clearinghouse option for customers that prefer not to evaluate and contract with a clearinghouse directly. This means that you can submit clean 837s, track status, and auto-post 835s without leaving the EHR. The advantage of this option is that you work with only one vendor and receive your training and support from ICANotes instead of the clearinghouse.
If you already work with a clearinghouse or prefer to contract with a clearinghouse separately, ICANotes supports third party integrations with many popular medical billing clearinghouses: Waystar, Availity, Trizetto, eTactics, Claim.MD, and OfficeAlly.
Frequently Asked Questions
Why an Integrated EHR + Clearinghouse Beats a Standalone Vendor
After you’ve compared features to find the best clearinghouse for medical billing, the biggest lever on outcomes is how tightly that clearinghouse connects to your documentation, scheduling, and billing workflows inside your EHR.
With an integrated ICANotes stack, mental health practices gain:
-
One source of truth from intake to payment - fewer logins, fewer handoffs, faster follow-through.
-
Cleaner claims from the start - structured behavioral-health charting and coding tools reduce scrubbing errors before 837 submission.
-
Real-time eligibility & status in workflow - 270/271 and claim updates surface where staff already work, not in a separate portal.
-
Reliable 835 auto-posting & reconciliation - fewer “orphaned” payments and clearer audit trails.
-
Denial prevention & work queues - rejections/denials route to task lists with reason codes and next steps.
-
End-to-end visibility - scheduling, documentation, claims, and payments roll into unified KPI reporting.
-
Stronger resilience & support - one vendor to escalate across EHR, clearinghouse, and RCM processes.
ICANotes at a Glance
-
Charting built for behavioral health: guided templates that capture the data payers expect.
-
Practice management + billing: scheduling, claims, statements, ERA/EFT, and integrated clearinghouse connections.
-
Optional Revenue Cycle Management (RCM): enrollment support, submissions, follow-up, and appeals when you need extra hands.
Bottom Line: choosing a capable mental health clearinghouse matters, but pairing it with an integrated EHR and RCM workflow is what turns fewer errors into faster cash and a calmer front office.
Schedule a Live Demo
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals—built to streamline documentation, improve compliance, and enhance patient care.
- Simplify clinical charting
- Stay organized with appointment scheduling
- Reduce no-shows with automated reminders
- Improve client engagement with a secure patient portal
- Provide flexible care with HIPAA-compliant telehealth
Simplify clinical charting
Stay organized with appointment scheduling
Reduce no-shows with automated reminders
Improve client engagement with a secure patient portal
Provide flexible care with HIPAA-compliant telehealth
Related Posts
Fatima C. Davis is the RCM Manager at ICANotes and a seasoned expert in behavioral health revenue cycle management. With over 20 years of experience, she specializes in optimizing collections, reducing denials, and ensuring compliance across diverse payer landscapes. Fatima has led RCM operations for large multi-agency systems and is passionate about helping behavioral health practices achieve financial sustainability.