Blog > Documentation >Handwritten Behavioral Health Notes Cost You Time
Why Electronic Therapy Notes Are Better Than Handwritten Ones
While handwritten notes have long been associated with therapy sessions, clinging to pen and paper may be costing you more than you realize. From lost time and reduced efficiency to added documentation stress, manual note-taking can create unnecessary burdens for today’s behavioral health professionals. This post explores the hidden drawbacks of handwritten notes and explains how switching to electronic therapy notes can streamline your workflow, improve compliance, and give you more time to focus on clients. If you're still jotting notes by hand, it's time to consider a smarter, faster approach.

Last Updated: September 11, 2025


What You'll Learn
-
Why handwritten therapy notes can slow you down and increase administrative burden
-
How delayed documentation affects clinical accuracy and insurance reimbursement
-
The risks associated with storing and managing paper records in a digital world
-
The benefits of switching to electronic therapy notes for improved efficiency, security, and client care
Can Therapy Notes be Handwritten?
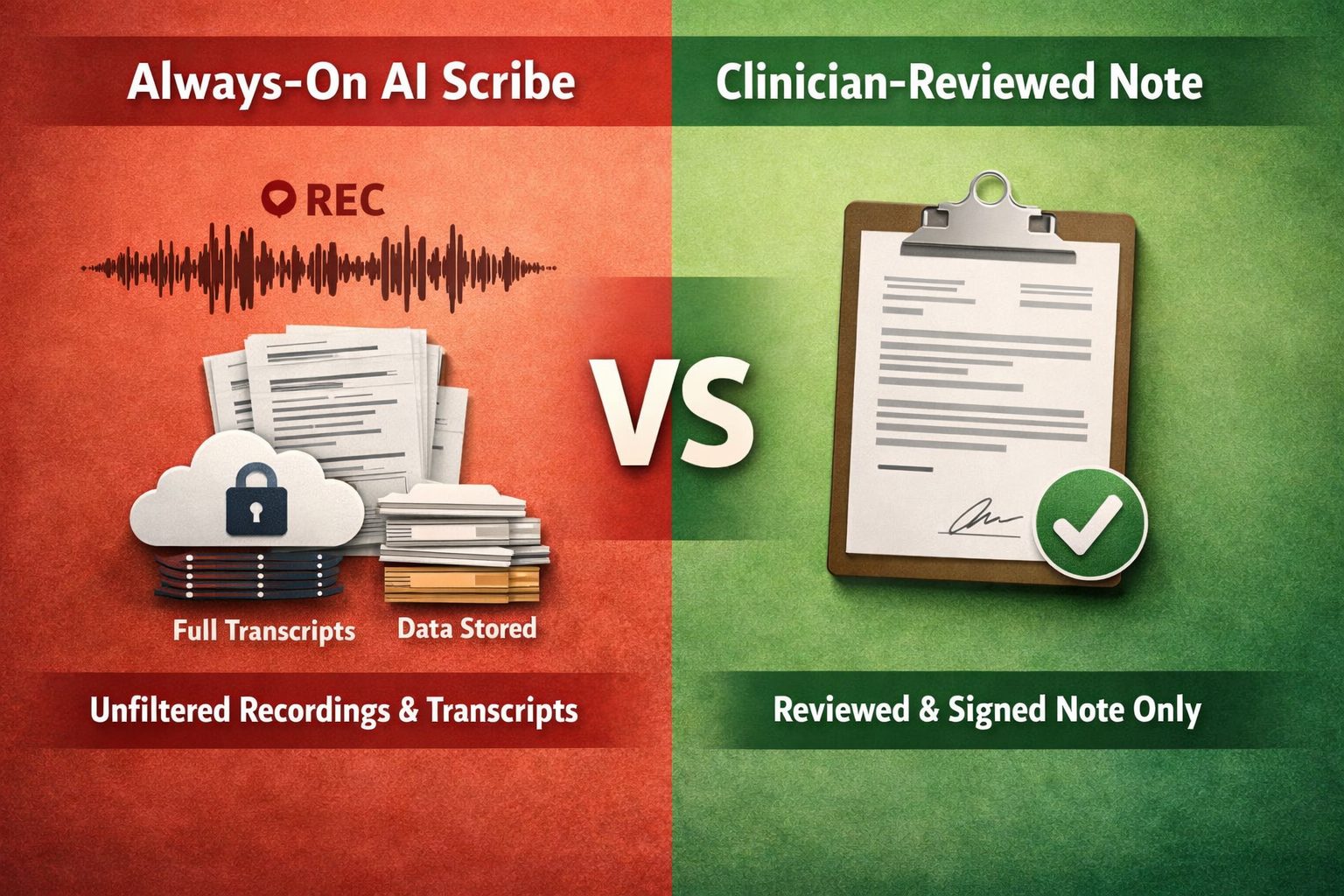
Therapy notes can be handwritten, however, there is a lot to consider before choosing to handwrite notes. First, whether it's a good idea to handwrite a mental health note depends on the type of note you plan to take. For example, you may feel more comfortable handwriting psychotherapy notes.
Psychotherapy notes are kept separately from a client's records. They are your private notes that may include the thoughts, ideas, or feelings you have during a session.
Psychotherapy notes are optional, so you can use any note-taking method or format you wish. Depending on your preferences, you might find it easier and faster to type than handwrite psychotherapy notes.
All other documentation, including progress notes, should not be handwritten. Progress notes are shareable and may be audited or subpoenaed. Clients also have a right to read their progress notes. Progress notes need to be accurate, legible, and easy to understand.
If you create electronic therapy notes, you reduce the risk of misunderstandings or other issues related to accuracy and readability.
Disadvantages of Handwritten Therapy Notes
Healthcare is transforming into a digital industry. More health care providers are embracing digital tools, such as EHR systems to improve patient outcomes. According to the Office of the National Coordinator for Health Information Technology (ONC), as of 2021, nearly 9 in 10 office-based physicians (approximately 88%) have adopted an EHR system, with 78% using certified EHR technology. An EHR system may include features such as documentation management, billing integrations and a telehealth platform.
In addition, digital tools like EHRs increase interoperability and patient access to their medical records. Both of these elements are critical to improving health outcomes and patient engagement. Today, patients expect personalized health care, and they want easy digital access to their medical records, including their mental health notes.
Handwritten notes do not fit into the digital healthcare transformation for many reasons. Here are some disadvantages of handwritten therapy notes and reasons to become a paperless practice:
- Time-consuming: Writing therapy notes should take up to 10% of your time, and the other 90% should be spent on patient care. If you're handwriting progress notes before entering them into your EHR, you're adding an extra step to your workflow. If you only keep handwritten notes in your practice, you don't get to access an EHR's note-taking templates, which can help you complete documentation tasks in less than five minutes.
- Worrisome to clients: Handwriting is a slower process than typing or clicking on pre-formatted data. If you prefer to take handwritten progress or psychotherapy notes during sessions, you'll spend a greater portion of your time writing, and this could make clients feel as if you aren't giving them your full attention. As a therapy best practice, you should minimize note-taking during sessions as much as possible.
- Repetitive: Writing therapy progress notes for regular clients can feel like a tedious process when certain elements are unlikely to change from one session to the next. For example, handwriting details about a client's diagnosis, symptoms, or appearance can get repetitive. Using an EHR system allows you to click on data and quickly add details to progress notes.
- Inaccurate: Since handwriting is a slower process than typing, it may be challenging to keep up with specific details a client shares. For example, if a client speaks rapidly about symptoms and important dates, you need to write fast. Writing too quickly could lead to errors, missing information, or sloppy handwriting — which can be hard to interpret later on.
- Lack of security: Handwritten therapy notes can easily get lost or misplaced, which puts patients' privacy at risk. As a behavioral health professional, you are obligated to protect your clients' privacy, whether you handwrite notes or store them electronically. With handwritten notes, this may mean keeping them in a locked file cabinet, but even that may not be enough to protect files from theft, fires, or other disasters.
- Difficult to correct: If you're typing a note and notice you misspelled a client's name or entered the wrong date of birth, you simply need to hit the backspace key and start over. If you handwrite therapy notes, mistakes are harder to change unless you use a pencil, which presents another problem — pencil marks are too easy to erase. It's better to type electronic therapy notes from the start to avoid creating documents that contain scribbles or crossed-out information.
- Harder to organize: Handwritten notes need to be stored in an organized manner so you can easily access them when you need to. This level of the organization takes time and continual maintenance. Electronic therapy notes are stored conveniently in one place and are much easier to access and keep organized.
- Impedes continuity of care: If you plan to go on vacation or refer your client to a different counselor for other reasons, you probably don't want to hand the new therapist handwritten notes. Handwritten notes are more difficult to read than typed documents, and you may worry about them getting lost as they travel from one place to the next.
- Reduces staff efficiency: Since handwritten documents are typically harder to read, your staff members may have to spend extra time in the workday deciphering progress notes or other information. They'll also have to locate the notes in a client's paper file, which can be a time-consuming task if notes aren't kept organized.
How Handwritten Therapy Notes Present Confidentiality Issues
Just like electronic therapy notes, handwritten notes must meet the standards set by the Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule. If a covered health care provider fails to comply with the Privacy Rule, they may be subject to a fine, or in some cases, imprisonment. Even if your practice isn't considered a covered entity under HIPAA, behavioral health professionals have an ethical obligation to protect client confidentiality.
Handwritten notes make it more challenging to maintain client confidentiality for several reasons. Unlike electronic documents, which can only be accessed by authorized users, anyone can pick up and read a handwritten note. It's also easy for handwritten notes to leave an office and get into the wrong hands.
For example, in recent years, employees have continued to inadvertently expose protected health information through practices like leaving notes unsecured or mishandling PHI, as documented in the May 2025 HIPAA Journal breach report, where numerous healthcare data breaches resulted from unauthorized access or improper disposal by staff members
Handwritten notes make it easier to breach confidentiality laws within a healthcare facility as well. For instance, a staff member might forget to file a client's record and leave it out in the open. Likewise, employees might not shred handwritten notes when they're supposed to, or they might drop off paper documents in an unsecured area. Something as simple as forgetting to lock a file cabinet could lead to a HIPAA violation.
Should You Be Using Electronic Therapy Notes Software?
Electronic therapy notes offer enhanced security and help keep practices HIPAA-compliant. In today's healthcare industry, electronic notes also play a vital role in delivering high-quality patient care. Here are reasons all practitioners should use note-taking software to create and maintain clients' records:
- Save time: Using note-taking software can drastically reduce the amount of time you spend completing documentation tasks. Electronic note software is often customizable, so you can create templates, checkboxes, or drop-down menus that suit your practice. You can quickly write progress or psychotherapy notes during or after appointments using customized point-and-click templates.
- Promote care coordination: Electronic therapy notes make it easier to communicate with other health care providers. For example, you can use secure therapy notes software to exchange medication information or medical histories with a client's primary care physician. This can help you provide safer, holistic care because you'll have a better understanding of each client's health overall.
- Share your notes with clients: Patients are becoming more involved in their healthcare, and part of this is due to the healthcare industry becoming more digitized. For example, psychologists who use EHR software will soon need to provide patients digital access to their notes under new federal rules. Even if these rules do not apply to your practice, you may still want to share notes with your clients and encourage them to be more engaged in their treatment. Electronic therapy notes make it easier to share legible notes that clients can understand and benefit from.
- Comply with privacy laws: Note-taking software, such as EHR systems, often include advanced security measures. EHR software should be certified by the Office of the National Coordinator for Health Information Technology (ONC) and offer password protection, audit trails, and data encryption. These features can help you establish HIPAA compliance, so you won't have to waste time or energy worrying about security issues.
- Improve your services: Electronic therapy notes can help your practice run more efficiently and get all staff members on the same page. As a result, you can provide high-quality care to your clients and improve their health outcomes.

If you want to enjoy the benefits of creating electronic therapy notes, your next step is to choose the right software for your practice. If you want to maximize your practice's efficiency and improve operations overall, consider implementing comprehensive EHR software.
EHR systems go beyond typical office management software. If you choose an EHR designed for the behavioral health field, you can use the system to complete all your documentation tasks, including note-taking, submitting insurance claim forms, and sharing notes with patients. With EHR software, you can update your practice, keep pace with other health care providers, and most importantly, meet or exceed your clients' expectations.
FAQ: Handwritten vs Electronic Therapy Notes
Making the Most of Your Time with ICANotes
When selecting an EHR for your behavioral health practice, you have a lot to consider. Not all EHRs or practice management systems reduce documentation time or solve workplace inefficiencies. Before choosing an EHR, identify your priorities and look for software features that will meet your needs and help you reach goals.
ICANotes is comprehensive EHR software designed to meet the needs of busy behavioral health professionals. Each feature was created to increase efficiency and decrease the documentation burden that mental health providers face. By incorporating ICANotes into your practice, you'll have access to the following features and benefits:
- Electronic notes for therapists: ICANotes has therapy note templates which make it easy to create, share, and manage electronic documents securely. Using these customizable templates and automated data population, you can quickly and accurately write progress notes and conduct assessments.
- Patient portal: Your clients can use the patient portal to access their medical history, confirm or cancel appointments, complete intake forms, request refills, and communicate with you electronically. The patient portal decreases your workload and improves patient satisfaction.
- Billing solutions: With flexible, integrated billing solutions, you can create superbills, process payments, and submit insurance claims all in your EHR.
- Telehealth capabilities: ICANotes offers the option to add telehealth capabilities to your plan. Using the telehealth feature, you can conduct HIPAA-compliant video sessions and offer your services from anywhere.
- E-prescribing: With the e-prescribing software, you can send accurate and legible prescriptions directly to a pharmacy from your office. E-prescribing makes it much easier and safer for patients to get the medications they need.
Lastly, you can be assured that ICANotes maintains full compliance with HIPAA to protect your practice and clients' privacy. As ONC-certified software, ICANotes will help you meet a range of state and federal standards.
Request a Free Trial of ICANotes Today

Note-taking is a part of the job as a behavioral health professional, but it doesn't need to take time away from your clients. ICANotes can help you save time, reduce your documentation burden and write better electronic therapy notes. To try ICANotes, request your free trial or contact our Sales team at 443-347-0990. If you'd like note-taking tips for therapists or more industry information, check out our blog.
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
- Complete Notes in Minutes - Purpose-built for behavioral health charting
- Always Audit-Ready – Structured documentation that meets payer requirements
- Keep Your Schedule Full – Automated reminders reduce costly no-shows
- Engage Clients Seamlessly – Secure portal for forms, messages, and payments
- HIPAA-Compliant Telehealth built into your workflow
Complete Notes in Minutes – Purpose-built for behavioral health charting
Always Audit-Ready – Structured documentation that meets payer requirements
Keep Your Schedule Full – Automated reminders reduce costly no-shows
Engage Clients Seamlessly – Secure portal for forms, messages, and payments
HIPAA-Compliant Telehealth built into your workflow
Related Posts
About the Author
Dr. October Boyles is a behavioral health expert and clinical leader with extensive expertise in nursing, compliance, and healthcare operations. With a Doctor of Nursing Practice (DNP) and advanced degrees in nursing, she specializes in evidence-based practices, EHR optimization, and improving outcomes in behavioral health settings. Dr. Boyles is passionate about empowering clinicians with the tools and strategies needed to deliver high-quality, patient-centered care.