Blog > Billing and Insurance > Tips for Passing Behavioral Health Utilization Review
Clinical Documentation Tips for Passing a Behavioral Health Utilization Review
Behavioral health utilization reviews can disrupt care and reimbursement if your documentation doesn’t hold up to scrutiny. This article equips clinicians with clear strategies and sample note language to support medical necessity, reduce denials, and pass reviews with confidence—whether you're in outpatient therapy or higher levels of care.

Last Updated: June 5, 2025

Mental health clinicians are no strangers to the frustrating dance of insurance authorizations. A utilization review (UR) can feel like an administrative hurdle, but in reality, it’s your opportunity to clearly demonstrate the medical necessity of treatment. Good documentation doesn’t just protect your client’s care—it protects your time and income, too.
Whether you're working in outpatient therapy, intensive outpatient programs (IOP), or higher levels of care, here are essential documentation strategies to help you succeed in utilization reviews.
What Is a Utilization Review in Behavioral Health?
A utilization review is the insurance company’s process for determining whether the services you’re providing—or planning to provide—are medically necessary. Reviews may occur before treatment starts (preauthorization), during care (concurrent review), or after services have been rendered (retrospective review).
You’ll typically be asked to submit documentation or speak with a reviewer about:
- The client’s current symptoms and functioning
- The treatment plan and goals
- Progress made (or lack thereof)
- The rationale for continued care
Why Clinical Documentation Matters
In behavioral health, your clinical judgment may be spot-on—but if your documentation doesn’t reflect it, payers may still deny care. Utilization review decisions are based solely on what’s documented, not on what was said or implied during a session. That means even the most effective therapy can be deemed “not medically necessary” if your notes don’t tell a clear story.
When documentation is vague, repetitive, or disconnected from the treatment plan, it raises red flags for reviewers. Common issues that lead to denials include:
- Using general language like “talked about stress” without tying it to functional impairment
- Repeating the same note structure across sessions without showing progress or reassessment
- Failing to update goals or interventions when the client’s condition changes
These lapses can result in denied authorizations, delayed payments, or worse—interrupted care for your clients.
By contrast, clear, concise, and goal-oriented notes do more than satisfy compliance checkboxes. They:
- Demonstrate medical necessity by showing how symptoms impair daily functioning
- Track client progress toward specific goals, or explain why progress isn’t occurring
- Support continuity of care through updated treatment plans and clinical rationale
- Provide protection during audits by presenting a defensible record of decision-making
In short, high-quality documentation isn’t just paperwork—it’s a clinical tool, a legal safeguard, and a vital bridge between care and coverage. And with today’s growing demand for mental health services, payers are scrutinizing notes more than ever. Let your documentation be your strongest advocate.
Tips for Documenting with Utilization Review in Mind
1. Align Notes with Diagnoses and Treatment Goals
Make sure each session note connects the intervention to the client’s diagnosis and goals from the treatment plan. Reviewers want to see consistency and purpose behind each session.
Instead of: “Client was tearful and discussed recent stress.”
Try:
“Client presented with tearfulness and hopelessness consistent with MDD diagnosis; discussed recent work-related stress contributing to worsening depressive symptoms and inability to function at work.”
2. Highlight Functional Impairment
Use language that shows how symptoms are interfering with the client’s daily life—this is central to medical necessity.
Examples to include:
- “Unable to maintain employment due to panic attacks”
- “Withdrawn from social and family interactions”
- “Significant sleep disturbance impeding concentration at school”
3. Demonstrate Progress or Justify Lack of It
Utilization reviewers expect either measurable progress or a strong clinical justification for why progress is slow.
Progress language:
“Client reports a 50% reduction in panic attacks since initiating exposure therapy.”
Justification for lack of progress:
“Client remains emotionally dysregulated due to recent trauma exposure; continued stabilization through DBT skills is clinically indicated.”
4. Document Interventions Clearly
Use specific and evidence-based intervention language. Avoid generic phrases like “talked about feelings” or “provided support.”
Instead of: “Supportive counseling provided.”
Try: “Utilized cognitive restructuring to challenge maladaptive thoughts contributing to suicidal ideation.”
5. Include Risk Factors When Relevant
If your client presents with suicidal ideation, self-harming behaviors, substance use, or other clinical risk factors, be sure to document these clearly and describe the specific interventions you’re using to manage the risk. This not only justifies continued treatment but also demonstrates your commitment to client safety and clinical oversight.
Payers want to see that you're actively assessing and addressing risk, not just noting its presence.
✅ Example Progress Note Language:
"Client endorsed passive suicidal ideation with no current plan or intent. Denied access to lethal means. Initiated safety planning during session and provided client with crisis line resources. Clinician will follow up in 48 hours and increase session frequency to twice weekly for continued monitoring."
This kind of language:
- Documents the presence of risk
- Shows an immediate clinical response
- Outlines a plan for follow-up and containment
- Supports medical necessity by indicating that care must continue to ensure safety
Even if the client’s risk level is low or has improved, noting this change with context still supports your request for continued services
Struggling to find the right words?
Download our free cheat sheet of sample progress note language that clearly supports medical necessity and strengthens your case with payers. Perfect for outpatient, IOP, or higher levels of care.
Get your copy now — keep it nearby when writing or preparing for reviews.
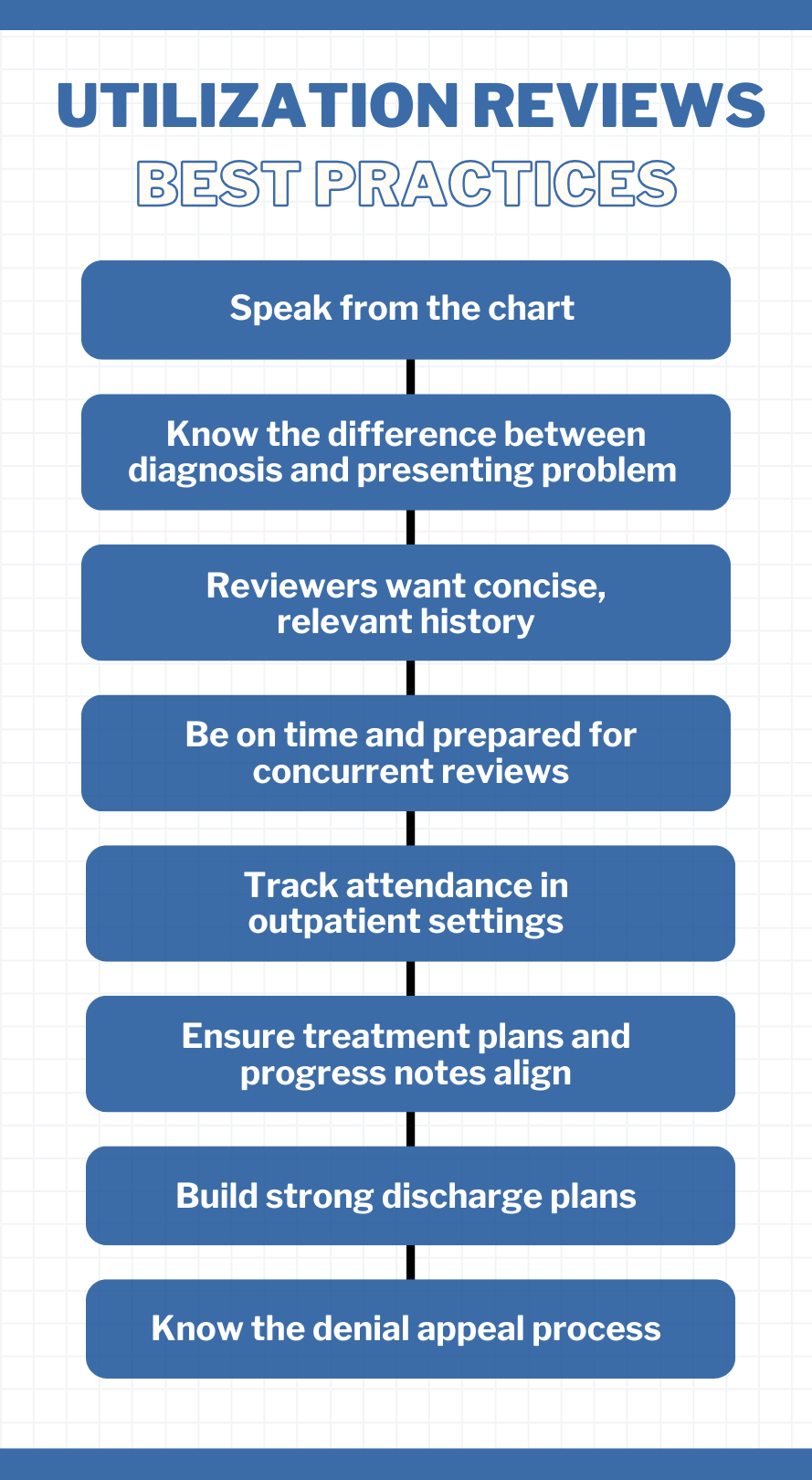
Utilization Review Best Practices
Utilization reviews don’t just evaluate your clinical decisions—they scrutinize the accuracy, clarity, and consistency of your documentation. Being prepared with best practices can make the difference between approval and denial. The following tips will help you navigate reviews confidently, advocate effectively for your clients, and ensure your notes stand up to payer expectations.
- Speak from the chart. Never offer opinions. Stick to what is documented.
- Know the difference between diagnosis and presenting problem. The diagnosis might be MDD, but the presenting problem is increased suicidal thoughts or inability to function.
- Reviewers want concise, relevant history. Stick to what's clinically significant for the current treatment episode.
- Be on time and prepared for concurrent reviews. Know your patient’s attendance, medication changes, and treatment plan details.
- Track attendance in outpatient settings. Missed sessions can result in denials for "failure to meet criteria."
- Ensure treatment plans and progress notes align. Reviewers will check for documentation that supports planned interventions and goals.
- Build strong discharge plans. Include continued goals, follow-up supports, crisis contacts, and client "homework."
- Know the denial appeal process. Start with a peer review and escalate to formal appeals with proper patient waivers when needed.
How ICANotes Supports Documentation for Behavioral Health Utilization Reviews
When it comes to passing a behavioral health utilization review, the quality of your documentation matters—and ICANotes was built to make it easier.
ICANotes is a behavioral health EHR designed to help clinicians write faster, more complete, and medically defensible notes that meet payer expectations. Here's how it supports you during utilization reviews:
-
Structured Templates Linked to Diagnoses
ICANotes automatically links clinical documentation to ICD-10 diagnoses and treatment goals, ensuring every note reflects medical necessity.
-
Built-In Mental Health Terminology
Choose from preconfigured, clinically-relevant phrases tailored to behavioral health. This reduces vague language and makes it easier to show functional impairment and progress over time.
-
Integrated Treatment Plans
Treatment plans are built into the workflow and can be easily updated to reflect changes in symptoms, functioning, and progress—perfect for meeting concurrent review requirements.
-
Audit-Ready Notes
Every note generated in ICANotes is time-stamped, securely stored, and consistent with payer standards, helping clinicians avoid denials and withstand audits.
-
Faster Progress Notes
With its click-based interface, ICANotes enables you to produce comprehensive notes in minutes, freeing up time to focus on care instead of paperwork.
-
Smart Progress Note Generation
Produce detailed, defensible notes in minutes—so you spend less time charting and more time delivering care.
-
Clinical Summary Generator
Create complete utilization review packets with one click. ICANotes compiles diagnoses, treatment plans, and session notes into an exportable, reviewer-friendly document.
-
Managed Care Alerts
Set alerts for when managed care sessions are about to run out so no review opportunity is missed.
Whether you're preparing for a preauthorization or responding to a concurrent review, ICANotes helps ensure your documentation is accurate, defensible, and reimbursement ready.
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
- Complete Notes in Minutes - Purpose-built for behavioral health charting
- Always Audit-Ready – Structured documentation that meets payer requirements
- Keep Your Schedule Full – Automated reminders reduce costly no-shows
- Engage Clients Seamlessly – Secure portal for forms, messages, and payments
- HIPAA-Compliant Telehealth built into your workflow
Complete Notes in Minutes – Purpose-built for behavioral health charting
Always Audit-Ready – Structured documentation that meets payer requirements
Keep Your Schedule Full – Automated reminders reduce costly no-shows
Engage Clients Seamlessly – Secure portal for forms, messages, and payments
HIPAA-Compliant Telehealth built into your workflow
Final Thoughts on Behavioral Health Utilization Review
Utilization reviews can feel like interruptions to care—but with strong documentation, they can instead be opportunities to advocate effectively for your clients. Write with clarity, be outcome-focused, and always tie your work to medical necessity. Tools like ICANotes can streamline this process by helping you structure notes, link them to diagnoses and goals, and generate consistent language that meets payer expectations.
Related Posts
Dr. October Boyles is a behavioral health expert and clinical leader with extensive expertise in nursing, compliance, and healthcare operations. With a Doctor of Nursing Practice (DNP) from Aspen University and advanced degrees in nursing, she specializes in evidence-based practices, EHR optimization, and improving outcomes in behavioral health settings. Dr. Boyles is passionate about empowering clinicians with the tools and strategies needed to deliver high-quality, patient-centered care.