Blog > Documentation > Biopsychosocial Assessment Template
How to Write a Biopsychosocial Assessment + Examples and Templates
A biopsychosocial assessment is a tool clinicians use to understand how a client’s physical health, mental state, and life circumstances affect their well-being. This guide shows you exactly how to write one, with clear steps, sample questions, example notes, and a free template to use in your practice.

Last Updated: December 4, 2025


What You'll Learn
-
How to write a biopsychosocial assessment using a clear, structured format across biological, psychological, and social domains.
-
Key questions to ask in each section, plus example notes that illustrate how to translate client responses into clinically accurate documentation.
-
How to integrate biological, psychological, and social data into a cohesive narrative that supports diagnosis, treatment planning, and medical necessity.
-
A complete biopsychosocial assessment example—including a mental status exam and recommended treatment plan—to guide your clinical writing.
-
Best practices for improving assessment quality, avoiding common documentation errors, and strengthening your clinical formulation.
-
How standardized tools (PHQ-9, GAD-7, ASI, etc.) can enhance accuracy, track symptom severity, and support evidence-based care.
-
Time-saving tips and templates for streamlining your biopsychosocial assessments using ICANotes’ structured, menu-driven documentation tools.
Contents
What is a Biopsychosocial Assessment?
What is Included in a Biopsychosocial Assessment?
How to Write a Biopsychosocial Assessment as a Mental Health Professional
Biopsychosocial Assessment Example (with Template)
Tips for Writing a Biopsychosocial Assessment
Using Technology to Simplify Documentation
Why Use ICANotes for Biopsychosocial Assessments?
A strong biopsychosocial assessment forms the foundation for effective treatment. It helps you understand the full picture of a client’s health, identify underlying issues, and align care with their needs and goals. Done well, it also improves collaboration with other providers and supports accurate diagnoses and treatment planning.
What is a Biopsychosocial Assessment?
A biopsychosocial assessment is a clinical tool used to evaluate how biological, psychological, and social factors affect a client’s mental and physical health. It is typically completed during the intake process to support diagnosis, guide treatment planning, and document medical necessity.
The biopsychosocial model, developed by Dr. George Engel in 1977, emphasizes that health is influenced by physical conditions, mental states, behaviors, relationships, and environment.
In behavioral health settings, this approach helps identify underlying causes of symptoms, such as trauma or social stressors. It also supports more accurate documentation and allows for personalized, whole-person care.
Streamline your Intakes with this powerful form!
Download our Fillable Biopsychosocial Intake Form
Whether you're onboarding new clients or updating charts, this form helps you gather everything you need in one place.
What is Included in a Biopsychosocial Assessment?
Biological Factors
Psychological Factors
Social Factors
A biopsychosocial assessment typically includes detailed information across three core domains: biological, psychological, and social. Together, these areas offer a full picture of a client’s health, functioning, and environment.
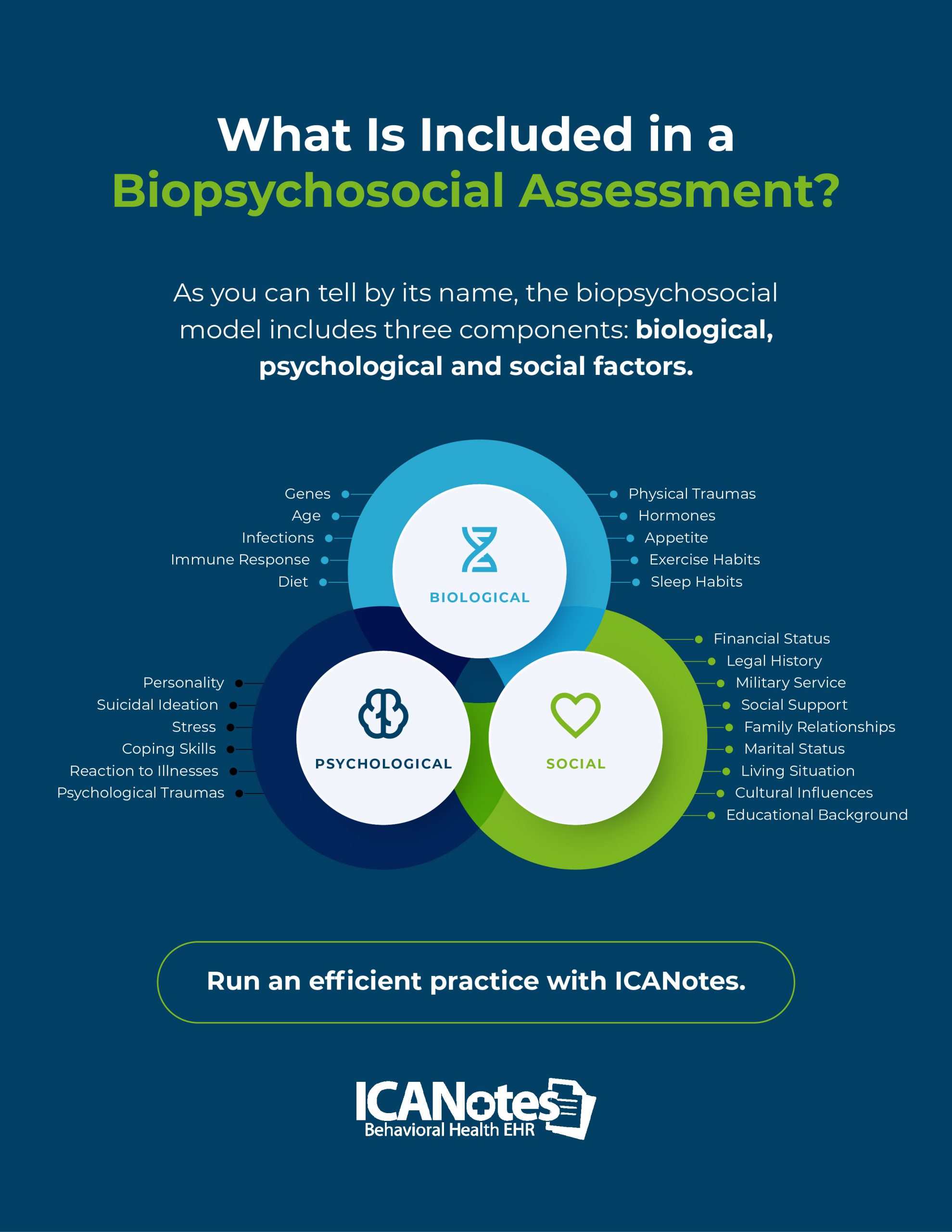
1. Biological Factors
Biological factors in a biopsychosocial assessment include a client’s physical health, medical history, and genetic background. This may involve chronic illnesses, current medications, past surgeries, sleep habits, diet, substance use, and family history of medical or mental health conditions.
Clinicians assess these areas to understand how physical health may be contributing to mental or emotional symptoms. Questions often focus on recent medical issues, allergies, past treatments, and inherited conditions that may influence diagnosis and care planning.
Useful biological domains to assess include:
- Genes
- Age
- Immune Response
- Infections
- Environmental toxins
- Physical traumas
- Diet
- Appetite
- Hormones
- Sleep/exercise habits
Example Biological Assessment Questions
Asking clear, structured questions can help surface important patterns. Examples include:
- Do you have any ongoing or chronic health conditions?
- What medications are you currently taking, and how do they affect you?
- Have you had any surgeries or hospitalizations in the past?
- Is there a history of mental health or substance use issues in your family?
- How would you describe your typical sleep and eating routines?
Gathering this information helps clinicians identify whether physical health issues may be contributing to psychological symptoms or creating barriers to treatment.

Example Biological Assessment Section
Client is a 42-year-old male with Type 2 diabetes, hypertension, and chronic migraines. He takes metformin 500 mg twice daily and lisinopril 20 mg daily. Headaches occur about three times per week and are managed with over-the-counter ibuprofen. Sleep averages 5–6 hours per night due to nocturia and pain. Diet is high in processed foods due to a busy work schedule. No history of surgeries, hospitalizations, or known drug allergies. Family history includes maternal depression and paternal cardiovascular disease.
2. Psychological Factors
Psychological factors include a client’s thoughts, emotions, behaviors, and coping skills. These internal experiences are central to mental health and often interact with physical symptoms. For instance, over 36% of people with chronic pain report depressive symptoms, and more than 55% experience anxiety or depression.
This part of the assessment explores how clients handle stress, regulate emotions, and manage mental health symptoms. It also includes mental health history, prior diagnoses, treatment experiences, and current psychological functioning.
Common psychological domains to assess include:
- Personality
- Psychological traumas
- Stress
- Coping skills
- Suicidal ideation
- Reaction to illness
Example Psychological Assessment Questions
These questions help guide your understanding of the client’s emotional and mental state:
- What brings you in today?
- How long have you been experiencing this issue?
- How would you describe your overall mood and mental state?
- What are some of your personal strengths and challenges?
- Have you ever been in therapy or taken medication for mental health?
- Have you experienced any traumatic events in your life?
- Do you ever have thoughts of harming yourself or others?
- What are you hoping to gain from therapy or treatment?
Gathering this information helps clinicians identify psychological patterns that may contribute to a client’s distress and tailor interventions that support meaningful progress.

Example Psychological Assessment Section
Client reports six months of anxiety and low mood, with sleep disruption, irritability, and work-related worry. Describes panic attacks 1–2 times per month. Denies current suicidal ideation but recalls past thoughts during a stressful period two years ago. No psychiatric hospitalizations. History of generalized anxiety disorder, previously treated with short-term CBT. Not currently on psychiatric medication. Describes himself as a perfectionist and struggles with uncertainty. Uses mindfulness and exercise to cope.
3. Social Factors
Social factors include the external conditions that influence a client’s relationships, identity, and access to resources. These may involve family dynamics, income, education, housing, cultural background, and community ties.
Research shows that social determinants like income, education, and neighborhood safety strongly affect mental health. Stable housing and financial security support well-being, while poverty, unemployment, and discrimination can increase stress and worsen symptoms. Assessing these areas helps identify both barriers and supports that influence treatment.
Common social domains to assess include:
- Family relationships
- Social support
- Marital status
- Cultural influences
- Food security
- Income level
- Discrimination
- Living situation
- Military service
- Spiritual or religious background
- Hobbies and recreational activities
- Sexual history
- Financial status
- Legal history
- Educational background
- Employment status and work history
- Access to affordable healthcare
Example Social Assessment Questions
These questions help uncover the client’s broader social environment:
- Who do you live with, and who do you see most often?
- What is your relationship like with your family?
- Do you have close friends or a support system you can rely on?
- Are you involved in any community, spiritual, or cultural groups?
- What kind of work do you currently do? What have you done in the past?
- How much stress does your job or financial situation cause?
- Have you ever served in the military?
- Have you had any legal issues, been arrested, or sentenced for a crime?
- Do you have consistent access to food, housing, and healthcare?
Assessing social factors helps paint a fuller picture of the client’s circumstances and allows for treatment plans that account for both internal and external influences on mental health.

Example Social Assessment Section
The client lives with a long-term partner and reports a supportive relationship. Works full-time as a customer service supervisor; satisfied overall but notes recent stress from understaffing. Holds a bachelor’s degree and is financially stable with limited savings. Maintains weekly contact with his mother. Identifies as non-religious and is not active in community or spiritual groups. Social life is limited outside of work, though he is interested in joining a sports league. No legal issues or military history.
How to Write a Biopsychosocial Assessment as a Mental Health Professional
After you've gathered data about your client, you can write a biopsychosocial assessment report. Your report will help you understand your client as a whole individual to devise an effective treatment plan. You can also share your assessment with colleagues or physicians to coordinate care.
Here's a biopsychosocial assessment outline to help you get started.
Basic Information
Begin your report with basic information about your client. This should include:
- Identifying information: Include the client’s name, gender, date of birth, and marital status.
- Referral: Name the person or agency that referred the client and the reason for the referral.
- Presenting problem: Summarize why the client is seeking help, how long the issue has been present, their perspective on the problem, and any past attempts to address it.
- Source of data: List tools or methods used to collect information (e.g., interviews, questionnaires, records). Note how involved the client was in the process.
- General description of the client: Describe the client’s appearance, mood, and engagement during the session. Note any issues with memory, thinking, speech, or signs of distress.
Client's History and Current Functioning
Summarize key areas of the client’s background and current functioning that impact their mental health:
- Family history: Include relationships during childhood and any family history of substance use, legal issues, or psychiatric conditions.
- Education: Note academic history, challenges, and current goals.
- Employment: Outline current job status, work history, and relevant skills or training.
- Spiritual beliefs: Mention religious or spiritual affiliation and community involvement.
- Military service: Indicate if the client served, with their role, service dates, major stressors, and discharge type.
- Medical history: Include current health status, major illnesses or injuries, medications, and family medical history.
- Mental health: Describe past and current experiences with mental illness, trauma, or abuse.
- Substance use: Summarize history of alcohol or drug use, including treatment or rehab.
- Social life: Note support system, relationships, hobbies, and community involvement.
- Daily functioning: Assess the ability to meet basic needs like housing, food, and personal care.
- Legal history: Mention past or current legal concerns, including domestic issues.
- Strengths and coping: Identify coping skills, strengths, and areas of resilience.
- Other factors: Include any relevant environmental or psychosocial issues, such as discrimination or identity-related stress.

Your Assessment and Recommendations
After you provide an overview of your client's current and past psychological, biological, and social states, it's time to include your professional assessment. You might offer the following information:
- Brief summary: In about three to five sentences, summarize what you've already written in your report, including your client's primary problem and any associated factors. Describe your client's level of urgency regarding the problem. Mention any secondary issues or concerns your client shared.
- Client's appearance: Describe how your client appeared during the interview, including signs of anxiety or depression and any memory or speech issues. If you also conducted a mental status exam during your initial meeting with a client, include it in this section.
- Your observations: Provide your observations of the client and their current state. Discuss your assessment of the client's motivation to use your service and modify behaviors.
- Diagnosis: Include your diagnosis and any diagnoses your client claimed they'd been given in the past by other therapists.
- Goals and recommendations: Identify long-term and short-term goals. Describe the type of treatment you think is best for your client and any suggestions for services and resources. Include how long you think your client should receive treatment.
Biopsychosocial Assessment Example (with Template)
To bring all the elements together, here’s a sample biopsychosocial assessment written in a structured format. This example shows how information from the biological, psychological, and social domains can be integrated into a cohesive clinical narrative. It also follows a format commonly used in intake documentation across behavioral health settings.

Sample Biopsychosocial Assessment
Client Overview
Name: Maria L.
Age: 35
Date of Assessment: November 15, 2025
Referral Source: Self
Presenting Problem: Maria reports increased anxiety, difficulty sleeping, and persistent low mood over the past several months, affecting her work and personal life.
Biological
Maria has a history of hypothyroidism and seasonal allergies. She is currently prescribed levothyroxine 75 mcg daily. She denies any recent hospitalizations or surgeries. Sleep is disrupted (4–5 hours per night), and appetite is reduced. She does not use alcohol, tobacco, or recreational drugs. No known drug allergies. Family history includes depression (mother) and high blood pressure (father).
Psychological
Maria describes a pattern of persistent worry, fatigue, and occasional panic attacks. She reports difficulty concentrating and feeling overwhelmed at work. Symptoms began approximately six months ago following the loss of a close friend. She denies current suicidal ideation but has experienced passive thoughts of hopelessness. Maria was previously in therapy during college for mild depression. She identifies journaling and walking as helpful coping strategies. No history of psychiatric hospitalization.
Social
Maria lives alone in an apartment and works as a marketing coordinator. She reports a high level of job-related stress and limited work-life balance. She is close to her sister, who lives nearby, but reports minimal social interaction outside of work. She expresses interest in joining a support group but is unsure how to start. Financially stable with moderate student loan debt. No legal issues or military service. Identifies as Catholic but is not currently practicing.
Mental Status Exam
Client is alert, oriented x3, and appropriately groomed. Eye contact is limited but improves with rapport. Mood is described as “anxious and tired,” with congruent affect. Speech is clear and goal-directed. No delusions or hallucinations noted. Thought content is focused on recent loss and work stress. Insight and judgment are fair.
Assessment and Plan
Maria presents with symptoms consistent with generalized anxiety disorder and possible adjustment disorder with depressed mood. Symptoms appear to be exacerbated by recent grief and occupational stress. She shows motivation to engage in therapy and has several protective factors, including stable housing and family support.
Plan:
- Begin weekly individual therapy focused on anxiety management and grief processing
- Provide psychoeducation on GAD and healthy coping techniques
- Refer to the primary care physician for thyroid evaluation and sleep concerns
- Recommend support group options and assist with initial outreach
- Reassess symptom severity in 4 weeks using GAD-7 and PHQ-9.
Tips for Writing a Biopsychosocial Assessment
A clear, well-structured biopsychosocial assessment helps other providers understand the client’s clinical picture, contributes to diagnostic accuracy, and supports coordinated care. Use the following tips to strengthen your assessment writing process.
1. Distinguish Objective Facts from Subjective Impressions
Be intentional about separating what the client reports from your clinical observations.
- Objective information includes direct quotes, reported symptoms, or past diagnoses.
- Subjective impressions reflect your clinical judgment, such as observed affect, tone of voice, or behavior during the session.
Always clarify the source. For example:
- “Client reports difficulty sleeping for the past three months.”
- “Clinician observed flat affect and minimal eye contact.”
This distinction supports documentation accuracy and helps other providers interpret your findings.
2. Provide a Balanced Perspective
Your assessment should present a well-rounded view of the client’s functioning. Include not only symptoms and challenges but also protective factors, coping strategies, and personal strengths. This helps reduce stigma and supports a strengths-based, person-centered treatment approach.
For example, a client struggling with anxiety may also have strong insight, supportive relationships, or effective coping strategies worth noting.
3. Prioritize the Most Pressing Issues
Identify the most urgent or clinically significant concerns and lead with those. While all information is valuable, not every detail needs equal emphasis. Focus your narrative on the symptoms or factors that most directly impact functioning, safety, or treatment direction.
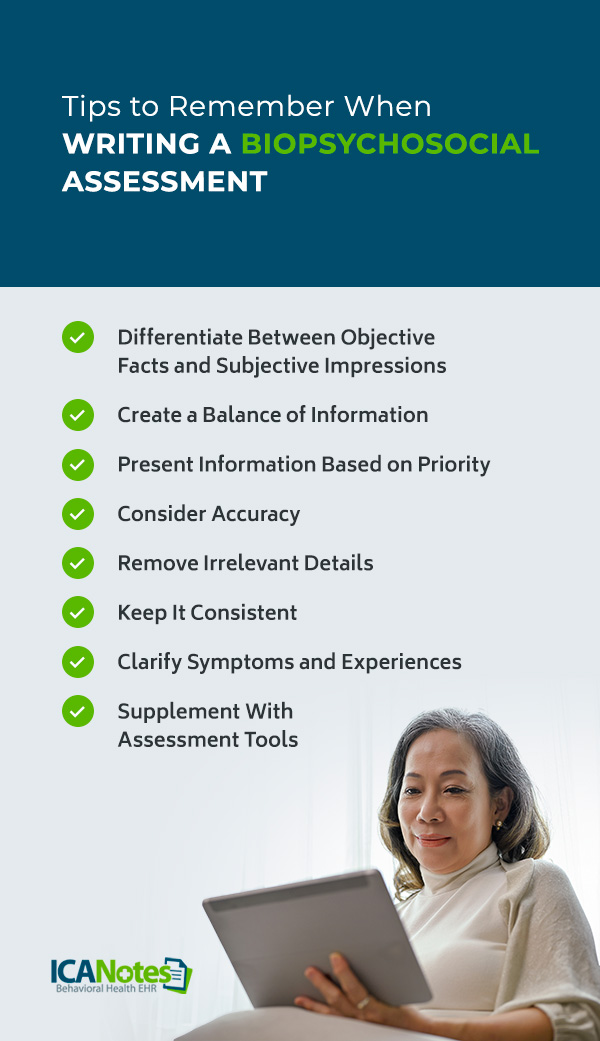
For example, suicidal ideation, active substance use, or recent trauma may need deeper exploration and planning than more chronic, low-impact issues.
4. Ensure Clinical Accuracy
Your report may be referenced by other clinicians, case managers, or insurers. Be precise when summarizing symptoms, history, and treatment needs. Double-check that diagnoses are supported by the documented data and that terminology is used correctly.
Avoid speculation, exaggeration, or assumptions. If a statement is based on the client’s report or your impression, make that clear in your wording.
5. Focus on Relevant Details
Keep your documentation concise by filtering out tangents or information that does not contribute to clinical understanding or treatment planning. Focus on data that explains the client’s current functioning, diagnoses, or goals.
It’s also acceptable if one area (biological, psychological, or social) yields less data. For instance, a client’s symptoms may be strongly influenced by financial stress (social) without clear biological contributors. In such cases, prioritize the relevant domains.
6. Maintain Consistency with Findings
Make sure your narrative and diagnostic impressions align. If you diagnose major depressive disorder, your assessment should describe hallmark features like low mood, fatigue, guilt, sleep or appetite changes, or suicidal ideation.
Inconsistent or vague notes can undermine the credibility of your documentation and make treatment planning more difficult for other providers.
7. Clarify Ambiguous Responses
Clients may describe their experiences in broad or emotional terms. Ask gentle follow-ups to clarify duration, frequency, intensity, and impact.
For example:
- “I’m really stressed” becomes, “I feel overwhelmed at work 5 days a week, and it’s been building for 3 months.”
- “I’ve been down lately” becomes, “I’ve had low mood most days, and it’s starting to affect my appetite and motivation.”
These details strengthen your formulation and support an accurate diagnosis.
8. Use Standardized Assessment Tools When Appropriate
Supplementing your clinical interview with validated tools can improve reliability and objectivity. Consider integrating brief measures that assess symptom severity, risk, or functional impact.
Commonly used tools include:
- PHQ-9 for depression
- GAD-7 for anxiety
- K10 for psychological distress
- MDQ for mood disorders
- HAM-A for anxiety symptoms
- LEC-5 for trauma history.
These instruments can support diagnosis, justify medical necessity, and help monitor change over time.
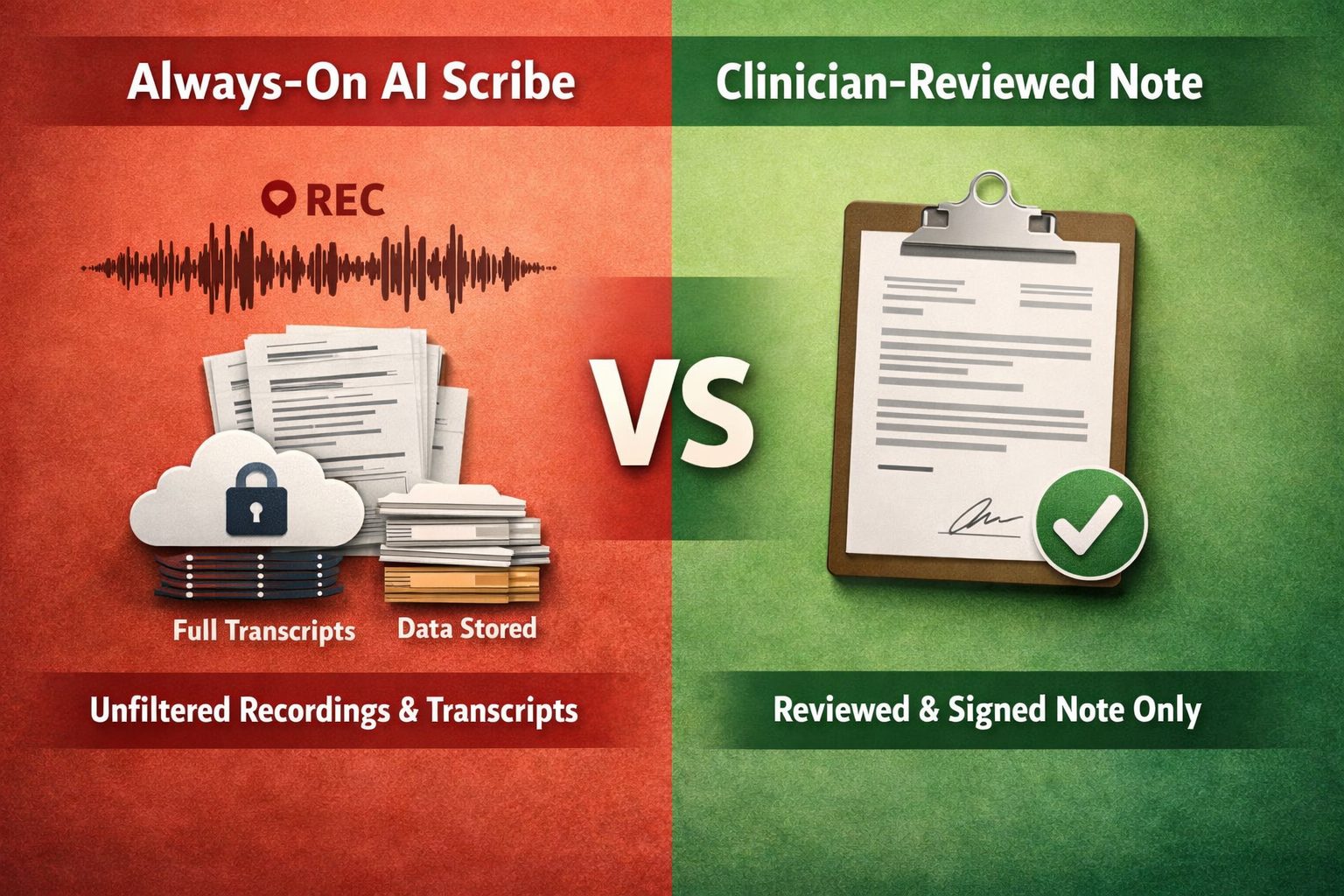
Using Technology to Simplify Documentation
Clinical documentation is a core part of behavioral health care, but it can be time-consuming without the right support. In addition to biopsychosocial assessments, providers often manage progress notes, treatment plans, consent forms, and other records that require accuracy, organization, and compliance.
ICANotes is a mental health EHR built to reduce your documentation burden. With ICANotes, you can:
- Scan and store digital forms
- Access records securely from any device
- Keep documentation organized and HIPAA-compliant
- Use prebuilt templates and auto-populate fields to save time
- Create accurate, legible notes that support better care and faster reimbursement
- Improve client satisfaction through a secure patient portal.
ICANotes helps you work more efficiently so you can focus more on clinical care.
Why Use ICANotes for Biopsychosocial Assessments?
ICANotes makes it easy to complete biopsychosocial assessments by allowing clients to enter their intake information through a secure, mobile-friendly form. This data flows directly into the clinician’s assessment note, reducing duplicate entry and saving time during documentation.
Clinicians can use ICANotes’ menu-driven templates to generate detailed, structured assessments with just a few clicks. Built-in tools like PHQ-9, GAD-7, and ASI scales are included to help collect standardized data and support compliance.
ICANotes helps behavioral health professionals document faster, reduce errors, and focus more on patient care. Start a 30-day free trial or schedule a demo to see it in action.
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
- Complete Notes in Minutes - Purpose-built for behavioral health charting
- Always Audit-Ready – Structured documentation that meets payer requirements
- Keep Your Schedule Full – Automated reminders reduce costly no-shows
- Engage Clients Seamlessly – Secure portal for forms, messages, and payments
- HIPAA-Compliant Telehealth built into your workflow
Complete Notes in Minutes – Purpose-built for behavioral health charting
Always Audit-Ready – Structured documentation that meets payer requirements
Keep Your Schedule Full – Automated reminders reduce costly no-shows
Engage Clients Seamlessly – Secure portal for forms, messages, and payments
HIPAA-Compliant Telehealth built into your workflow
Frequently Asked Questions
Related Posts
Dr. October Boyles is a behavioral health expert and clinical leader with extensive expertise in nursing, compliance, and healthcare operations. With a Doctor of Nursing Practice (DNP) from Aspen University and advanced degrees in nursing, she specializes in evidence-based practices, EHR optimization, and improving outcomes in behavioral health settings. Dr. Boyles is passionate about empowering clinicians with the tools and strategies needed to deliver high-quality, patient-centered care.