Blog > Treatment Strategies > Treatment Goals for Depression: SMART Goals & Objectives That Work
Treatment Goals for Depression: A Step-by-Step Guide That Works
Clear, measurable treatment goals for depression are essential for effective therapy and defensible documentation. This guide walks mental health clinicians through how to create treatment plan goals and objectives for depression, including the use of SMART goals to improve focus, motivation, progress tracking, and clinical outcomes. You’ll find practical examples, evidence-based strategies, and documentation tips to support high-quality, goal-driven depression treatment planning.

Last Updated: January 9, 2026


What You'll Learn
- Why clearly defined treatment goals for depression are essential for engagement, progress tracking, and outcomes
- How to write effective treatment plan goals and objectives for depression that are specific, measurable, and clinically meaningful
- How to apply the SMART goals framework for depression to improve motivation and accountability
- Examples of short-term and long-term treatment plan goals for depression across symptom severity levels
- How to align goals with evidence-based interventions and standardized measures like the PHQ-9
Contents
- Key Components of a Depression Treatment Plan
- Setting SMART Goals for Depression
- Examples of Treatment Goals and Objectives for Depression
- Therapeutic Interventions That Support Goals
- Track Progress and Adjust Your Treatment Plan
- Create Treatment Plans That Actually Work
- FAQs: Treatment Goals for Depression
- How ICANotes Supports Treatment Goals for Depression
Nearly 29% of U.S. adults report being diagnosed with depression in their lifetime — a figure that has increased by almost 10 percentage points since 2015. As depression becomes more prevalent, mental health clinicians increasingly need structured, evidence-based approaches to guide care.
Depression treatment plan goals and objectives are not simply documentation requirements — they are the foundation of effective, goal-directed therapy. A thorough assessment is the starting point, but clear, measurable goals are what translate clinical insight into actionable treatment. When goals are well defined, both clinicians and clients gain direction, motivation, and a reliable way to track meaningful progress over time.
In this guide, you’ll learn how to create treatment goals for depression that support real clinical outcomes. From understanding diagnostic criteria (such as the requirement that five or more symptoms be present during the same two-week period), to aligning goals with evidence-based interventions (including antidepressant treatments shown to significantly reduce symptoms within eight weeks), this article offers practical, step-by-step guidance. Whether you are new to treating depression or refining your clinical approach, these strategies will help you set treatment goals that meaningfully support recovery.
Understanding Treatment Goals for Depression
Setting meaningful treatment goals for depression serves as the cornerstone of effective therapy. Unlike generic treatment approaches, goal-oriented therapy provides structure, direction, and measurable outcomes that benefit both clients and therapists.
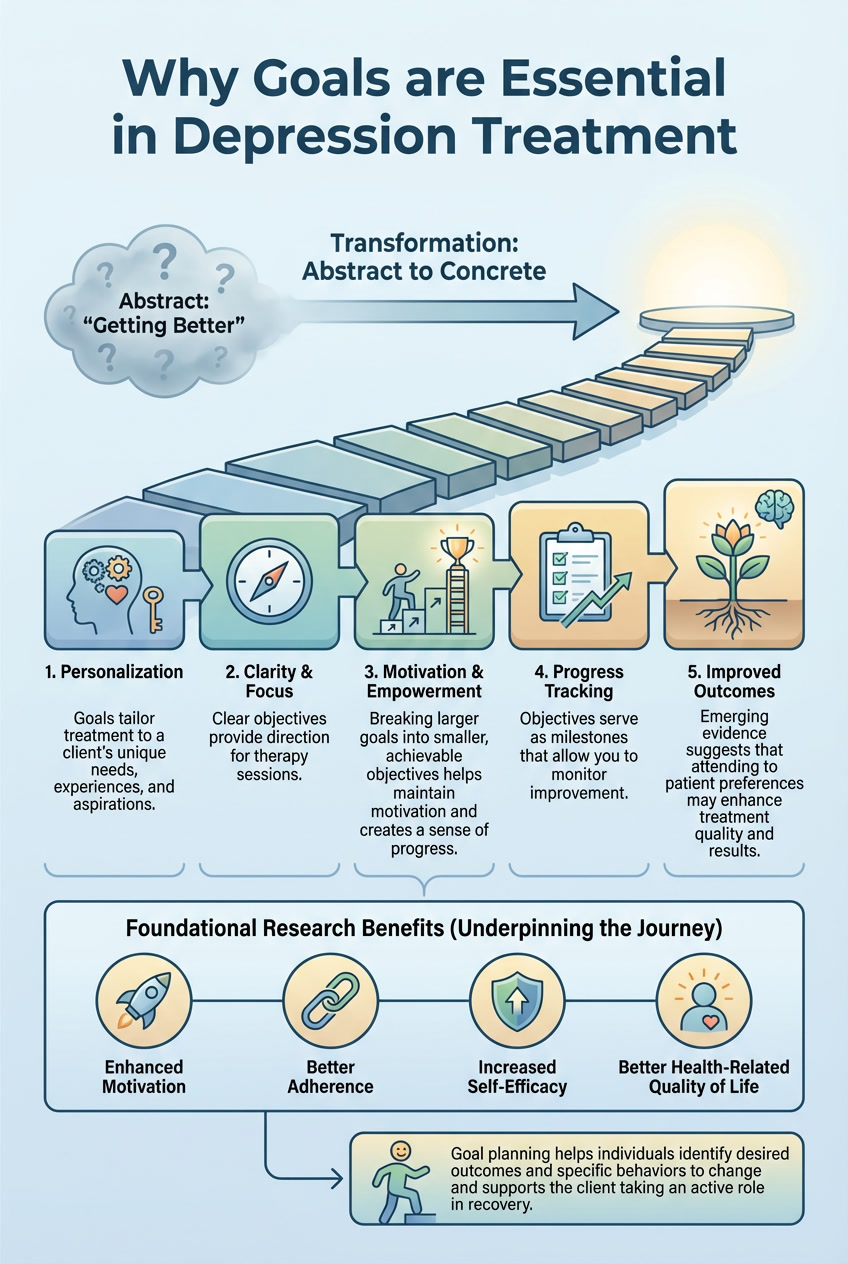
Why goals are essential in depression treatment
Treatment goals transform the abstract concept of "getting better" into concrete, achievable steps. Research shows that goal planning has been proven to enhance motivation, adherence, self-efficacy, and health-related quality of life. These goals aren't administrative formalities — they're powerful therapeutic tools that deliver specific benefits:
- Personalization: Goals tailor treatment to a client’s unique needs, experiences, and aspirations, ensuring therapy addresses what matters most to them.
- Clarity and focus: Clear objectives provide direction for therapy sessions, helping both client and therapist concentrate on priority issues rather than getting sidetracked.
- Motivation and empowerment: Breaking larger goals into smaller, achievable objectives helps maintain motivation and creates a sense of progress, especially during challenging periods.
- Progress tracking: Objectives serve as milestones that allow you to monitor improvement, celebrate successes, and identify areas needing adjustment.
- Improved outcomes: Emerging evidence suggests that attending to patient preferences may enhance treatment quality and results.
Goal planning helps individuals identify desired outcomes and specific behaviors to change. This process supports the client in taking an active role in recovery, fostering a sense of control that's often diminished during depressive episodes.
How goals guide therapy and recovery
Goal setting happens as an ongoing collaborative process between client and therapist. Throughout treatment, these goals continually guide therapeutic interventions, help evaluate progress, and keep recovery on track.
Treatment goals help clarify what steps need to be taken and keep both client and therapist focused on specific outcomes. This means starting with identifying the problem clearly, then setting realistic and meaningful goals as the foundation of your treatment plan.
Goal planning theory suggests that goals which are conscious, specific, and sufficiently challenging produce better results. Rather than setting a vague goal like "feeling better," a client might aim to "attend one social event per week" or "reduce negative self-talk by practicing thought records daily."
The SMART framework guides goal setting in depression treatment:
- Specific: Goals need to be clear and detailed, leaving no room for misinterpretation.
- Measurable: To track progress, goals must be quantifiable.
- Achievable: Goals should be realistic and attainable for your individual situation.
- Relevant: Your goals should be tailored to your unique circumstances and the factors influencing your depression.
- Time-bound: Setting timeframes for achieving objectives helps build structure and maintains focus.
Goal setting empowers the client to take charge of their mental health journey. This leads to improved quality of life — from healthier relationships to greater satisfaction in daily routines. Collaborative goal setting aligns with the principles of recovery that encompass self-determination, self-management, personal growth, and choice.
Research indicates that when clients receive treatment perceived as truly relevant to their needs, they exhibit greater commitment and engagement. This increased engagement significantly decreases drop-out rates, increases satisfaction, and improves outcomes. Evidence also suggests that clients are more likely to remain in therapy when treatment is congruent with their understanding of their problems and is perceived as helpful in addressing those problems.
Key Components of a Depression Treatment Plan
A depression treatment plan consists of four critical components that work together to create a roadmap for recovery. Understanding these elements allows you to develop structured approaches for addressing depressive symptoms effectively.
Related: Creating a Depression Treatment Plan: Examples & Best Practices
1. Problem identification
Creating an effective treatment plan starts with accurately identifying the specific depressive disorder and its severity. This initial diagnostic assessment typically utilizes standardized tools like the Patient Health Questionnaire (PHQ-9) to gauge symptom severity and determine the nature of depression.
Therapists need to understand which type of depression a client is experiencing before jumping into solutions. This might include major depressive disorder, persistent depressive disorder (lasting at least two years), or depression related to medical conditions. Problem identification also recognizes that around 30% of people with depression have treatment-resistant depression, where multiple medications or therapies have failed to improve symptoms.
The problem statement should describe the client’s presenting issues concisely, noting how depression impacts their daily functioning, relationships, and quality of life. This foundation ensures subsequent interventions target the right issues instead of applying generic approaches that prove ineffective.
2. Goal setting
After identifying the problem, collaborative goal setting becomes the next critical step — often missing from work with young people. Rather than therapists dictating treatment directions, the most meaningful therapy goals should come from within the client.
Effective goal setting transforms "feeling better" into concrete outcomes. You can start small when beginning therapy for depression. Goals provide direction, helping both client and therapist stay focused on specific desired endpoints that address the gap between the client’s current state and where they want to be.
The goal-setting process typically happens through discussions at the beginning of therapeutic interventions. These goals become concrete representations of intended endpoints and differ from academic or general life goals, although there may be overlap. Through this collaborative process, you gain autonomy and control that's often diminished during depressive episodes.
3. Measurable objectives
Goals without measurable objectives remain wishful thinking. Measurable objectives break down larger goals into concrete, quantifiable steps that allow for tracking progress. Avoid vague objectives like "client will have less anxiety" or "client will isolate less" as these don't provide clear metrics for improvement.
Create specific, measurable objectives such as: "Client will engage in two grounding exercises each morning on the bus prior to entering school building to aid in reduction of social anxiety." Progress can then be measured using standardized assessment tools like the PHQ-9 for depression or GAD-7 for anxiety, tracking score reductions from baseline (e.g., "reduction of score on PHQ-9 from 15 to 11 over eight weeks").
These measurable objectives serve as milestones that help maintain motivation throughout treatment. They also provide clear evaluation criteria to determine whether interventions are working or need adjustment.
4. Interventions and strategies
The final component involves selecting specific therapeutic techniques and strategies to address your depression symptoms. These typically include:
- Psychotherapy approaches: Including cognitive behavioral therapy (CBT), which helps challenge and change unhelpful thoughts; interpersonal therapy (IPT), which focuses on improving relationships; and supportive therapy, which emphasizes understanding your current struggle.
- Medication options: Antidepressants that have shown to reduce symptoms by greater than 50% after eight weeks of use, including escitalopram, mirtazapine, paroxetine, venlafaxine, and amitriptyline.
- Lifestyle modifications: Physical activity, dietary changes, sleep hygiene improvements, and increasing social support.
- Alternative treatments: Options like meditation, yoga, or acupuncture that complement traditional approaches.
For mild to moderate depression, psychotherapy is often tried first, with medication added later if needed. People with moderate or severe depression usually begin with medication as part of their initial treatment plan. Finding the right treatment may require trial and error, as what works varies between individuals.
Through careful implementation of these four components — problem identification, goal setting, measurable objectives, and targeted interventions — your depression treatment plan becomes a powerful tool for guiding recovery rather than just paperwork to complete.
Setting SMART Goals for Depression
Depression recovery requires clear direction and measurable milestones. The SMART goal framework offers a practical method for developing treatment goals that genuinely support progress in depression management.
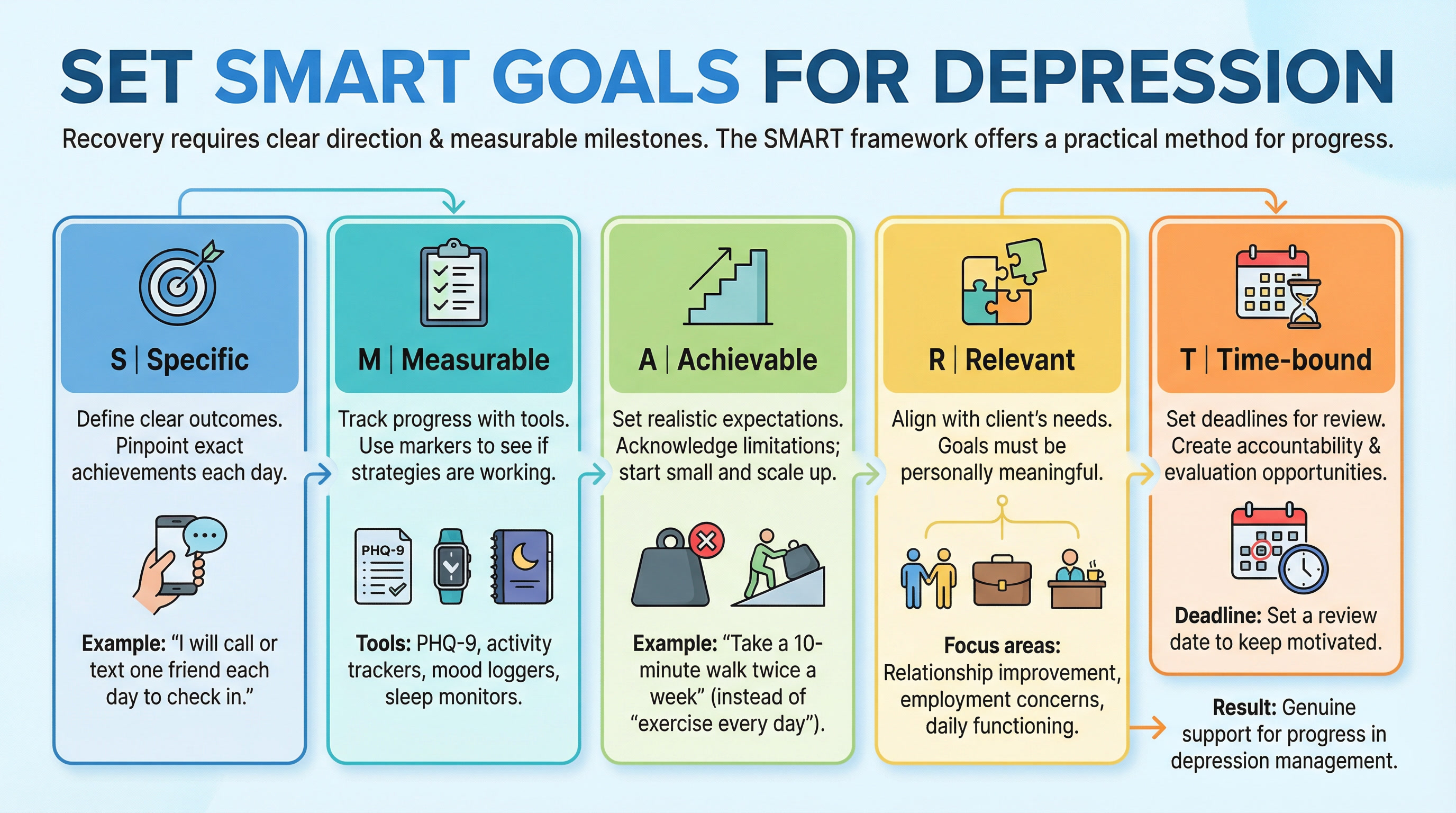
Specific: Define clear outcomes
Vague intentions like "feel better" or "be more active" often lead nowhere when battling depression. Specific goals pinpoint exactly what the client wants to achieve each day. Change "I want to connect with people" to "I will call or text one friend each day to check in" for clear direction.
Specificity helps break the paralysis that often accompanies depression by providing concrete actions to focus on. A well-defined goal answers the who, what, when, where, and why questions. Transform general objectives like "eat healthier" into specific actions such as "eat one serving of vegetables with lunch and dinner every day this week."
Measurable: Track progress with tools like PHQ-9
Without clear markers, it's difficult to know if your depression management strategies are working. The Patient Health Questionnaire-9 (PHQ-9) serves as a reliable tool for tracking progress, with scores of 5, 10, 15, and 20 representing cutpoints for mild, moderate, moderately severe, and severe depression, respectively.
This 9-item self-report measure assesses how frequently a client has experienced symptoms over the past two weeks. Administered regularly, it helps you make informed treatment decisions — a score of ≥ 9 indicates that medication doses might need adjustment, while scores < 5 suggest maintenance at the current dosage.
Other measurement approaches include:
- Activity tracking (counting completed walks or social interactions)
- Mood logging (rating mood on a scale daily)
- Sleep pattern monitoring (tracking hours and quality)
- Social interaction frequency
Achievable: Set realistic expectations
Recovery from depression isn't a straight line but rather a winding road with ups and downs. Setting attainable goals acknowledges a client’s current limitations while pushing gently toward improvement. If a client is struggling to get out of bed, aiming to run a marathon next week isn't realistic — but walking to the mailbox might be an excellent starting point.
The goal is to build momentum to break out of the vicious cycle of depression and inactivity. Start small and scale up. Rather than committing to "exercise every day," try "take a 10-minute walk twice a week."
Relevant: Align with client's needs
Goals must feel personally meaningful rather than imposed by others. A major aspect of providing patient-centered care involves being responsive to preferences, needs, and values when making treatment decisions.
Research suggests that when patients receive treatment perceived as truly relevant to their needs, they exhibit greater commitment and engagement in therapy, which significantly decreases drop-out rates and improves outcomes. Depression treatment goals should address the functional domains that matter most to the client — whether relationship improvement, employment concerns, or daily functioning.
Time-bound: Set deadlines for review
Without timeframes, goals can drift without progress. Setting specific deadlines creates a roadmap telling the client not just where they want to go but by when. "I will practice mindfulness for 10 minutes every day for the next two weeks" provides a concrete timeframe.
Time boundaries create accountability while offering natural opportunities to evaluate progress. According to the SMART criteria, goals should have deadlines that keep the client motivated. Follow this three-part approach:
- Set a goal (start journaling)
- Establish a timeframe (15 minutes, five days weekly, for three weeks)
- Schedule a review date to assess consistency and benefits.
Examples of Treatment Goals and Objectives for Depression
Treatment goals for depression come in different forms and timeframes, tailored to each person's unique circumstances and severity of symptoms. Concrete examples help you and your clients transform abstract concepts into actionable steps.
Short-term goals for depression
Depression treatment initially focuses on stabilizing mood and addressing immediate concerns. Short-term goals typically span a few days to several weeks and aim to build momentum for recovery. Depending on symptom severity, these goals might include:
For mild depression:
- Establishing a daily self-care practice involving exercise, healthy eating, and sufficient sleep, engaging in at least one self-care activity daily for four weeks
- Increasing social connection by participating in at least one social interaction weekly, such as meeting a friend for coffee
For moderate depression:
- Learning and implementing three specific coping techniques like deep breathing, progressive muscle relaxation, or journaling over six weeks
- Challenging negative thought patterns daily using cognitive restructuring techniques
For severe depression:
- Developing and implementing a safety plan to reduce risk of self-harm
- Attending all scheduled therapy sessions and adhering to prescribed medication regimens
Long-term goals for recovery
Beyond immediate symptom relief, long-term goals focus on sustained improvement and preventing relapse. These typically span months or even years, addressing deeper aspects of recovery:
- Reducing depressive symptoms so that PHQ-9 scores decrease from the current baseline (such as 15) to a lower target (such as 10 or below)
- Improving overall functioning and enhancing quality of life
- Building emotional resilience to better cope with stress and bounce back from setbacks
- Strengthening self-confidence and reducing guilt, particularly in specific life domains like parenting or work
Sample objectives for daily functioning
Measurable objectives break down larger goals into concrete, quantifiable steps. Effective objectives avoid vague statements like "client will have less anxiety" or "client will isolate less." Instead, consider these measurable examples:
- "Client will use progressive muscle relaxation and guided mindfulness practices each night 30 minutes prior to bed to improve sleep quality for the next 8 weeks"
- "Client will use the notes app as a thought log to capture cognitive distortions and replace them with balanced thoughts daily for 4 weeks"
- "Client will score 20 or below on the Beck Depression Inventory for 5 consecutive sessions"
- "Client will verbalize at least 3 coping skills for managing depression"
Case-based examples of goal setting
Sarah, a 28-year-old single mother experiencing persistent sadness, concentration difficulties, and feelings of worthlessness:
Goal 1: Improve mood and reduce depressive symptoms
- Objective: Identify and challenge negative thought patterns contributing to feelings of worthlessness
- Intervention: Use cognitive restructuring techniques to identify automatic negative thoughts and replace them with balanced perspectives
Goal 2: Improve sleep and appetite regulation
- Objective: Develop a structured sleep routine
- Intervention: Provide psychoeducation using CBT-I to integrate into sleep routine
Goal 3: Strengthen self-confidence around parenting
- Objective: Challenge self-critical thoughts related to being the "perfect parent"
- Intervention: Use CBT techniques to incorporate realistic, compassionate self-perceptions
Each example demonstrates how properly formulated goals and objectives create a clear path forward in depression treatment, providing structure, direction, and measurable milestones for recovery.
Therapeutic Interventions That Support Goals
Evidence-based therapeutic interventions form the backbone of successful depression treatment goals. Each approach offers unique benefits that address different aspects of depression, helping your clients achieve their recovery objectives.
Cognitive Behavioral Therapy (CBT)
CBT stands as one of the most well-documented and validated psychotherapeutic methods available for depression treatment. This approach targets depressed patients' irrational beliefs and distorted cognitions by challenging and reversing them. CBT helps you identify negative thought patterns and replace them with healthier, more realistic ones.
Studies demonstrate that CBT is an effective treatment strategy for depression, with a meta-analysis of 115 studies showing that combined treatment with pharmacotherapy is significantly more effective than medication alone. Evidence suggests that relapse rates for patients treated with CBT are lower compared to those treated with pharmacotherapy alone.
Interpersonal Therapy (IPT)
IPT focuses on improving your client's relationships with others to relieve mental health symptoms. Typically scheduled as a 12-16 week, once-weekly therapy for acute major depression, IPT helps identify triggers of depressive symptoms related to losses, social isolation, or difficulties in social interactions.
The basic principles of IPT include understanding that problematic interpersonal relationships directly relate to current mood, and improving these relationships will improve mood and mental health symptoms. IPT can help with bipolar disorder, eating disorders, and anxiety disorders.
Mindfulness-Based Cognitive Therapy (MBCT)
MBCT combines elements of CBT with mindfulness-based stress reduction. Originally developed for preventing relapse in people with recurrent depression, MBCT helps clients become better at recognizing and disengaging from habitual negative thinking patterns.
Research shows that eight weeks of MBCT treatment during remission reduces relapse rates. It can serve as a potential alternative to reduce or even stop antidepressant treatment without increasing relapse risk, especially for patients with more than two previous episodes.
Medication and pharmacological support
Several antidepressants have proven effective, including SSRIs, SNRIs, and atypical antidepressants. The decision to include medication requires weighing risks and benefits with input from a healthcare professional.
Lifestyle and behavioral activation
Behavioral activation helps increase engagement in pleasant activities, bringing clients into contact with reinforcing environmental contingencies. Physical activity is recommended by most depression treatment guidelines, as regular exercise alleviates symptoms and prevents relapses. Behavioral activation techniques help integrate pleasant activities into daily life, increasing positive interactions with the environment.
Track Progress and Adjust Your Treatment Plan
Regular progress monitoring determines whether your depression interventions work effectively or need adjustment. Tracking symptom changes helps you make informed treatment decisions.
Assessment tools that actually work
The Patient Health Questionnaire-9 (PHQ-9) and Beck Depression Inventory-II (BDI-II) stand out as the most widely used and validated tools for measuring depression severity. Both demonstrate excellent reliability at pre- and post-treatment (PHQ-9 α = .74 and .81; BDI-II α = .87 and .90).
These standardized assessments provide valuable insights:
- PHQ-9: Scores of 5, 10, 15, and 20 represent cutpoints for mild, moderate, moderately severe, and severe depression [7]
- BDI-II: Generally takes 10 minutes to complete and measures behavioral manifestations and severity
Given the PHQ-9's brevity and alignment with diagnostic criteria, many clinicians prefer it for routine monitoring.
When to revise treatment goals
The ideal timeframe for reassessment follows a structured pattern. Evaluate progress every two weeks during the first six weeks of treatment. Schedule visits every three weeks until achieving remission or changing treatment strategy. Once remission occurs, assessment every three months becomes sufficient.
Revise treatment goals whenever:
- A PHQ-9 score change of 5 or more points occurs (clinically significant change)
- Client shows partial response (improvement of 30-50%)
- Client shows no response (improvement ≤30%)
Make clients partners in progress reviews
Treatment plans should function as agreements between you and your client. Both parties must understand and consent to the material within the plan. Update treatment plans every 3-6 months, always in collaboration with your client.
Self-reporting of depression symptoms through tools like PHQ-9 reduces stigma and encourages honest symptom disclosure, placing clients at the center of their recovery journey.
Related: How to Make Progress with Your Clients in their Treatment Plans
Access Our Sample Treatment Plan Library
Get instant access to our full library of sample treatment plans.
Create Treatment Plans That Actually Work
Depression treatment requires structured goals, not wishful thinking. You've discovered how SMART goals transform vague intentions into concrete steps toward recovery. Rather than settling for abstract concepts, you now have a clear roadmap that both you and your client can follow.
Recovery builds on small, achievable goals that create momentum and confidence. Whether you're addressing mild symptoms or severe depression, tailored objectives address a client’s unique circumstances while providing measurable ways to track improvement.
The therapeutic approaches discussed, from CBT to medication options, work best when aligned with the client’s specific goals. These evidence-based interventions become powerful tools when matched with a client’s particular needs and preferences.
Track progress to ensure success. Tools like the PHQ-9 offer objective ways to monitor symptom changes, helping determine whether your current approach works or needs adjustment. Regular reassessment ensures your treatment plan evolves alongside the client’s changing needs.
Effective depression treatment centers around collaboration. The client’s active involvement in setting goals, selecting interventions, and reviewing progress places them at the heart of their recovery journey. This collaborative approach empowers the client to take ownership of their mental health while receiving professional guidance and support.
Depression may feel overwhelming for a client, but with clear treatment goals and evidence-based interventions, recovery becomes achievable. Focus on what truly matters — helping your clients move toward recovery with structured, measurable treatment plans that deliver results.
Frequently Asked Questions: Treatment Goals for Depression
How ICANotes Supports Treatment Goals for Depression
Creating effective treatment goals for depression requires more than clinical insight — it also depends on documentation tools that support clarity, consistency, and follow-through. ICANotes is purpose-built for behavioral health clinicians, making it easier to translate assessment findings into clear, measurable treatment plan goals and objectives.
Structured Goal Documentation That Supports Clinical Thinking
ICANotes guides clinicians through structured treatment planning workflows that align goals, objectives, and interventions without forcing rigid or generic templates. This structure helps ensure that depression treatment goals are:
-
Clearly linked to assessment findings
-
Written in measurable, outcome-oriented language
-
Easy to review and update over time
By organizing goals within a behavioral-health-specific framework, ICANotes supports both clinical reasoning and documentation requirements.
Seamless Alignment Between Goals and Progress Notes
One of the most common challenges in depression care is keeping treatment goals aligned with what actually happens in sessions. ICANotes helps bridge that gap by allowing clinicians to reference treatment plan goals directly within progress notes.
This connection makes it easier to:
-
Demonstrate how session interventions support established goals
-
Track progress toward treatment plan goals for depression over time
-
Maintain consistency across documentation
The result is clearer clinical storytelling and stronger documentation for utilization review.
Support for Measurement-Based Care
ICANotes supports the use of standardized screening tools commonly used in depression treatment, such as the PHQ-9. Incorporating these tools into documentation helps clinicians:
-
Establish baseline symptom severity
-
Monitor progress toward treatment goals objectively
-
Adjust goals and interventions based on data
This measurement-based approach strengthens both clinical decision-making and the defensibility of depression treatment plans.
Efficient Updates as Goals Evolve
Treatment goals for depression are not static. As symptoms improve, or new challenges emerge, goals and objectives must be updated. ICANotes makes it easier to revise treatment plans without duplicative work, helping clinicians:
-
Update goals and objectives at required intervals
-
Reflect clinical changes accurately
-
Maintain a clear historical record of treatment progression
This flexibility supports responsive, ethical care while reducing administrative burden.
Built Specifically for Behavioral Health Workflows
Unlike generic EHRs, ICANotes is designed specifically for behavioral health settings. That means treatment goals, objectives, and interventions are documented in language and workflows that reflect how clinicians actually practice.
For clinicians treating depression, this translates into treatment goals that are clearer, easier to manage, and better aligned with both clinical standards and documentation expectations.
See how ICANotes supports goal-driven depression treatment planning.
Start a free ICANotes trial to explore structured treatment goals, integrated progress notes, and outcome tracking — designed specifically for behavioral health clinicians.
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
- Complete Notes in Minutes - Purpose-built for behavioral health charting
- Always Audit-Ready – Structured documentation that meets payer requirements
- Keep Your Schedule Full – Automated reminders reduce costly no-shows
- Engage Clients Seamlessly – Secure portal for forms, messages, and payments
- HIPAA-Compliant Telehealth built into your workflow
Complete Notes in Minutes – Purpose-built for behavioral health charting
Always Audit-Ready – Structured documentation that meets payer requirements
Keep Your Schedule Full – Automated reminders reduce costly no-shows
Engage Clients Seamlessly – Secure portal for forms, messages, and payments
HIPAA-Compliant Telehealth built into your workflow
Related Posts
About the Author
Dr. October Boyles is a behavioral health expert and clinical leader with extensive expertise in nursing, compliance, and healthcare operations. With a Doctor of Nursing Practice (DNP) and advanced degrees in nursing, she specializes in evidence-based practices, EHR optimization, and improving outcomes in behavioral health settings. Dr. Boyles is passionate about empowering clinicians with the tools and strategies needed to deliver high-quality, patient-centered care.







