Blog > Practice Management > EHR for Small Behavioral Health Practices: What to Look for in 2025
EHR for Small Behavioral Health Practices: What to Look for in 2025

Andrew Holderied, Head of Sales and RCM
Last Updated: July 15, 2025


What You'll Learn
-
Learn which EHR functionalities are must-haves for small behavioral health practices in 2025.
- Practical questions to ask when comparing systems to help practices find the best EHR for their unique needs.
- Best practices for rolling out a new EHR to ensure a smooth and successful transition.
- How the right EHR can protect sensitive data (HIPAA/42 CFR compliance), scale as the practice grows, and deliver strong ROI.
Contents
-
- Why EHRs Matter for Small Behavioral Health Practices
- Top Features to Look for in 2025
- EHR vs EMR: What's the Difference?
- Evaluating EHR for Small Practices: Questions to Ask
- Cost Considerations and Scalability
- Compliance and Security
- Best Practices for Implementation
- How to Prepare Your Team for a New EHR
- Choosing the Right EHR for Long-Term Success
Why EHRs Matter for Small Behavioral Health Practices
EHRs have become essential in behavioral health care, even for solo practitioners and small group practices. These practice management systems serve as a digital backbone for modern clinics, centralizing patient records, automating routine tasks, and reducing the administrative overhead that often burdens clinicians.
An efficient EHR for small practices can help:
- Reduce time spent on documentation: Click-based templates and auto-populating fields cut note-writing time dramatically.
- Improve billing accuracy: Integrated coding support helps capture the right CPT and E/M codes, reducing denials and underbilling.
- Enhance care coordination: Shared notes, secure messaging, and structured data make collaboration easier within multidisciplinary teams.
- Maintain regulatory compliance: Built-in alerts, access controls, and audit trails help keep practices aligned with HIPAA, CMS, and state-specific rules.
- Enable telehealth and remote care: EHRs with integrated video platforms make virtual visits seamless, which has been especially vital since the pandemic.
When documentation can be completed in just minutes with click-based narrative tools, platforms like ICANotes help clinicians spend less time typing and more time engaging with patients. More complete records mean more personalized care. In short, a well-designed behavioral health EHR isn’t just a digital filing cabinet; it’s the engine of your practice.
Top Features to Look for in 2025
Many small behavioral health practices look for click-to-document workflows, built-in telehealth, and automated coding tools — features that ICANotes was designed to offer out of the box, supporting prescribers and non-prescribers with intuitive, role-based functionality.
The right tools can dramatically reduce clinician burnout, improve patient engagement, and streamline day-to-day operations. Here's what to look for in 2025:
1. Behavioral Health-Specific Templates
General-purpose EHRs often miss the nuances of mental health treatment. Look for systems offering built-in templates for biopsychosocial assessments, progress notes and discharge summaries. These should reflect DSM-5/ICD-10 diagnostic criteria and support treatment plans for conditions like depression, anxiety, PTSD, and substance use disorders.
2. Click-to-Document Functionality
If you prescribe medication, you will need access to e-Prescribing tools. These features often come at a higher price point due to the need for DEA compliance, patient safety checks, and integration with pharmacies.
Look for systems that support real-time medication history, prescription tracking, and lab orders. These tools help improve patient care but require more secure infrastructure and regular updates, which add to the monthly cost.
In ICANotes, the Prescriber Plan includes these advanced features to support clinical decisions and streamline your workflow.
3. Integrated Telehealth
Telehealth is no longer optional. Your EHR should support HIPAA-compliant video visits with features like real-time charting, screen sharing, session timers, and automatic reminders. Ideally, the platform should also allow you to initiate virtual sessions directly from the schedule or patient chart.
4. Patient Portal Access
An easy-to-use patient portal empowers clients to take a more active role in their care. Look for portals that allow clients to complete intake forms, message their provider, view visit summaries, make payments, and manage appointments — all within a secure interface.
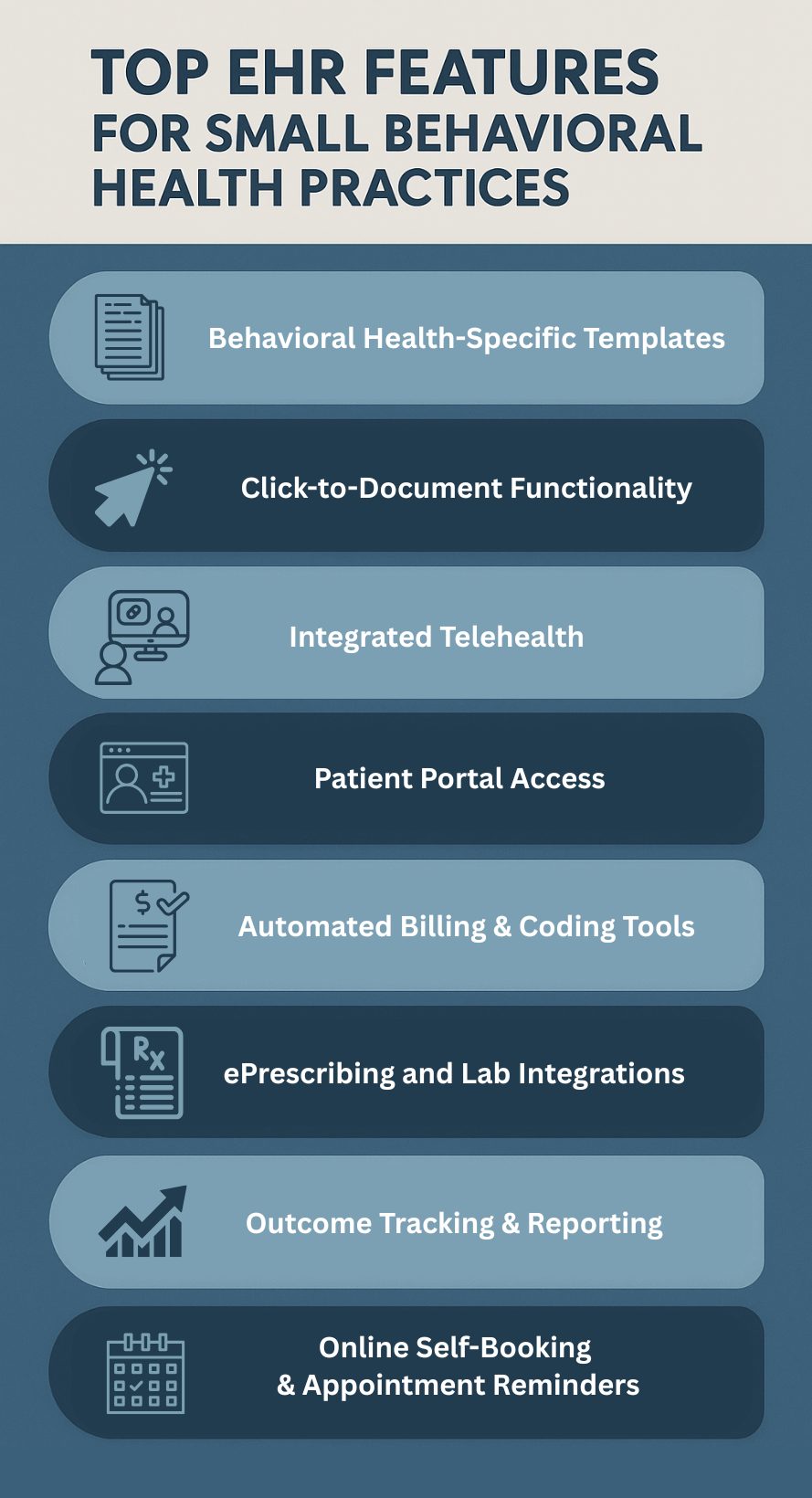
5. Automated Billing and Coding Tools
Billing is a pain point for many small practices. EHRs that include built-in coding guidance can help clinicians assign the correct CPT and E/M codes, reducing the likelihood of denials. Some systems also integrate with clearinghouses or offer revenue cycle management (RCM) as an optional service.
6. ePrescribing and Lab Integrations
If you have prescribing providers, make sure your EHR supports electronic prescribing (eRx), medication reconciliation, and controlled substances workflows (as well as seamless integration with state PDMP systems). Bonus points for systems that also offer lab ordering and result reviews within the same interface.
7. Outcome Tracking and Reporting
Demonstrating clinical progress is increasingly important for payers and value-based care initiatives. Choose an EHR with access to standardized screening tools (like PHQ-9, GAD-7, and ASRS) and the ability to generate outcome reports for individual patients and across your practice.
8. Online Self-Booking and Appointment Reminders
Many small practices operate without front-desk staff, so offering a way for new and returning clients to schedule, reschedule, or cancel appointments directly from your website is crucial. Look for systems like ICANotes that include integrated self-booking tools and automated email or text reminders to reduce no-shows and ensure clients show up prepared.
Use our calculator to learn what the ROI of using ICANotes could be for your business.
EHR vs EMR: What's the Difference?
The terms EHR (Electronic Health Record) and EMR (Electronic Medical Record) are often used interchangeably, but there are key differences:
- EMR systems for small practices typically focus on clinical data and internal documentation.
- EHRs are more comprehensive and include administrative functions like billing, scheduling, telehealth, and reporting.
In 2025, most modern software blurs the lines, but for small practices, an EHR is generally the better investment for holistic functionality.
Evaluating EHRs for Small Practices: Questions to Ask

Before choosing a platform, it's critical to evaluate how well an EHR system aligns with your practice's goals, workflows, and budget. Look for EHRs designed by clinicians — not retrofitted for behavioral health — that offer behavioral health–specific templates, telehealth, patient portals, and outcome-tracking tools. ICANotes exemplifies this category, having been built from the ground up for mental health users.
These questions can help you look past flashy features and focus on what really matters: long-term usability, flexibility, and compliance. A thoughtful selection process now can save you time, money, and headaches down the road.

Practical questions to guide your decision-making:
- Is this system specifically built for behavioral health? Look for software designed with mental health workflows in mind, not just adapted from general medical EHRs.
- Does it offer support for both prescribers and non-prescribers? Your team may include therapists, social workers, psychologists, and psychiatrists. Choose a system that accommodates various roles with tiered functionality.
- How customizable are the templates and forms? Can you modify note templates, intake forms, or treatment plans to match how your clinicians work? Flexibility can dramatically improve documentation efficiency.
- Can I integrate my current billing or clearinghouse tools? If you already use a billing solution or clearinghouse, check for integration compatibility. Seamless data flow can prevent costly errors and duplicate entries.
- What does onboarding and training look like? Does the vendor offer live support, video tutorials, or one-on-one training? Make sure your team has what they need to get up and running without frustration.
- Can I try the EHR before committing to a contract? Yes. ICANotes offers a free trial so you can explore the platform's features, workflows, and ease of use before committing. This gives you a risk-free opportunity to ensure it's a good fit for your practice.
- What kind of ongoing support is available? Look beyond onboarding. Is support available by phone or chat? Are response times fast and helpful? The quality of support can make or break your experience.
- Does it include compliance safeguards? Ensure that it has built-in tools for HIPAA and 42 CFR Part 2 and secure user access controls to protect sensitive data.
These questions can help you look past flashy features and focus on what really matters: long-term usability, flexibility, and compliance. A thoughtful selection process now can save you time, money, and headaches down the road.
Cost Considerations and Scalability
Transparent Pricing Tiers
Look for vendors that offer:
- Part-time and full-time plans
- Notes-only packages for documentation-only use
- Separate tiers for prescribers and non-prescribers.
Add-on Costs to Take Into Account
- Telehealth modules
- Text/email reminders
- Extra storage or document uploads
- Non-clinical staff accounts.
Scalability
An EHR for small practices should grow with you. Make sure the platform can accommodate additional users, locations, or service lines without major disruption.
Compliance and Security
Behavioral health records contain some of the most sensitive data in healthcare. Ensure your system meets:
- HIPAA compliance
- HITECH and Cures Act requirements
- Role-based access control
- Audit trails and user activity logging
- Regular security updates and encryption standards.
If your practice deals with substance use treatment, make sure the EHR is 42 CFR Part 2 compliant as well.
Best Practices for Implementation
Implementing a new EHR system can be transformative, but it also comes with challenges. Following best practices can help reduce disruption and ensure a smooth transition. Here’s how to set your small practice up for long-term success:
- Start with a pilot phase: Launch the EHR with a limited group of clinicians or a select subset of patients. This initial rollout can reveal technical issues or workflow challenges early on. Use the insights gathered to fine-tune templates, scheduling protocols, and documentation practices before expanding system-wide.
- Train your team: Comprehensive training is critical. Make sure everyone — clinicians, front desk staff, and billers — knows how to use the system. Take advantage of vendor-provided resources like live webinars, recorded tutorials, and knowledge bases. Consider role-specific training sessions to address different user needs.
- Transfer data securely: Care must be taken when migrating patient records from paper charts or another system. Confirm that the EHR vendor offers secure data migration services and clarify what's included—demographics, clinical notes, appointments, etc. Maintain backup copies of original records during the transition.
- Set realistic goals: Avoid trying to implement every feature at once. Focus on a phased approach — starting with documentation and scheduling, then adding billing, telehealth, and reporting tools. Success is measured by usability and adoption, not immediate perfection.
- Request regular check-ins: Establish a cadence of follow-ups with your vendor, especially in the first 90 days. Use these check-ins to troubleshoot issues, customize features, and get strategic advice. These meetings also help your team feel supported and heard.
- Monitor and adjust: After going live, track key metrics like documentation time, billing turnaround, or missed appointments. Use the data to refine workflows and ensure the system is delivering on its promises.
- Keep communication open: Encourage your team to share frustrations, suggestions, and successes. A feedback loop allows you to adapt processes and keep morale high during what can be a big adjustment.
By following these implementation best practices, small behavioral health practices can confidently and efficiently adopt EHR technology, setting the stage for improved care and a more streamlined operation.
How to Prepare Your Team for a New EHR

Implementing a new EHR system is not just a technical shift — it’s a cultural one. Here are ways to prepare your staff for success:
1. Involve Staff Early
Invite feedback from both clinical and administrative teams when selecting the system. Early buy-in makes training and adoption smoother.
2. Create EHR Champions
Designate one or two team members as internal experts. They can assist peers during and after implementation, reducing reliance on vendor support.
3. Customize Workflows Together
Use onboarding as a chance to rethink how your team operates. Map out current workflows and improve them using EHR tools.
4. Provide Ongoing Education
Training shouldn’t stop after going live. Schedule refreshers or tips-and-tricks sessions to ensure consistent usage.
5. Celebrate Milestones
Recognize small wins, such as the first successful billing cycle or fully digital note submission. It helps build confidence and morale.
Related: Which EHR Is Right for My Practice?
FAQs About EHR for Small Behavioral Health Practices
Choosing the Right EHR for Long-Term Success
For small behavioral health practices, selecting the right EHR in 2025 is more than a technical decision—it’s a strategic one. The right system can streamline operations, reduce administrative burdens, improve patient care, and support practice growth.
Whether you're switching from paper records, upgrading from a basic EMR, or looking for better documentation tools, prioritize platforms that are:
- Built for behavioral health
- Easy to use and customize
- Scalable as your practice grows
- Transparent in pricing and support
Choosing an EHR for small practices is an investment in your clinical efficiency and patient outcomes. Take the time to compare options, ask the right questions, and pick a system that works as hard as you do.
ICANotes offers a free trial that lets you explore features, test your typical workflows, and see how the system fits your needs. You can also book a live demo to get a guided walkthrough and ask questions before making a decision.
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
- Complete Notes in Minutes - Purpose-built for behavioral health charting
- Always Audit-Ready – Structured documentation that meets payer requirements
- Keep Your Schedule Full – Automated reminders reduce costly no-shows
- Engage Clients Seamlessly – Secure portal for forms, messages, and payments
- HIPAA-Compliant Telehealth built into your workflow
Complete Notes in Minutes – Purpose-built for behavioral health charting
Always Audit-Ready – Structured documentation that meets payer requirements
Keep Your Schedule Full – Automated reminders reduce costly no-shows
Engage Clients Seamlessly – Secure portal for forms, messages, and payments
HIPAA-Compliant Telehealth built into your workflow
Related Posts
Andrew Holderied is the Head of Sales and Revenue Cycle Management at ICANotes, bringing over 14 years of experience in healthcare technology. He has deep expertise in EHR, RCM, RPM, and EDI, and has dedicated his career to advancing solutions that enhance clinical workflows and financial outcomes for healthcare organizations. Andrew has successfully built and scaled high-performing sales teams at venture-backed companies, leading go-to-market strategies and driving revenue growth through data-driven execution and operational excellence.