Blog > Documentation > The Essential Components of an Initial Psychiatric Evaluation Template
The Essential Components of an Initial Psychiatric Evaluation Template
Writing a thorough initial psychiatric evaluation is essential for accurate diagnosis, treatment planning, and clinical continuity. In this post, we break down what should be included in a comprehensive initial psychiatric evaluation and offer a sample psychiatric evaluation to help psychiatrists and PMHNPs document efficiently and effectively. Plus, learn how ICANotes streamlines the entire process—from structured templates to seamless PDMP integration.

Last Updated: June 20, 2025

Accurate and thorough documentation is foundational to quality psychiatric care. For psychiatrists and psychiatric nurse practitioners, the initial psychiatric evaluation is more than just a clinical requirement—it sets the stage for diagnosis, treatment planning, and ongoing care. Yet, with increasing time constraints and administrative burdens, it’s easy to miss key details or fall into inefficient workflows.
Whether you’re refining your current documentation process or adopting a new EHR, having a structured initial psychiatric evaluation template can save time, improve compliance, and lead to better outcomes for both patients and providers.
What Is an Initial Psychiatric Evaluation?
An initial psychiatric evaluation is a comprehensive assessment of a patient’s mental, emotional, and behavioral health. It typically takes place during a first appointment and includes a detailed history, clinical observations, and formulation of a diagnostic impression and treatment plan.
This document becomes the foundation for future encounters—informing medication decisions, therapy recommendations, and coordination with other healthcare providers.
Key Components of a Comprehensive Psychiatric Evaluation Template
The ideal psychiatric assessment template balances structure with clinical flexibility. Here are the essential components that should be included:
1. Identifying Information / Demographics
- Patient name, DOB, MRN
- Date of evaluation
- Provider name and credentials
2. Reason for Referral / Chief Complaint
- Patient’s presenting problem in their own words
- Context of referral (self, primary care, emergency, etc.)
3. History of Present Illness (HPI)
- Onset, duration, and severity of symptoms
- Triggers, exacerbating/relieving factors
- Functional impact (work, relationships, daily life)
- Prior interventions and response
- Results from any evidence-based rating scales
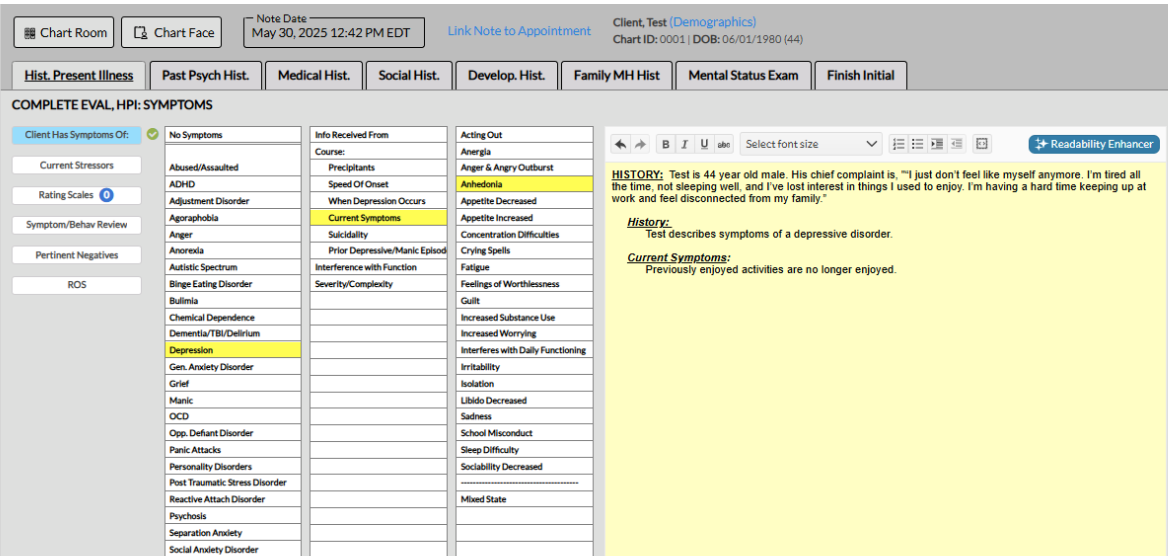
This is the HPI section of the comprehensive psychiatric evaluation template built into ICANotes. A fully narrative psychiatric assessment report is generated by clicking the relevant menu options. The menu content is fully customizable. With the mobile-friendly psychiatric intake module, most of the history is pre-populated by the patient, saving the clinician valuable documentation time.
4. Past Psychiatric History
- Previous diagnoses
- Hospitalizations
- Medications and adherence
- Prior psychotherapy or substance use treatment
5. Medical History
- Chronic conditions, surgeries, current medications
- Neurological concerns
- Allergies and adverse drug reactions
6. Substance Use History
- Alcohol, illicit drugs, prescription misuse
- Frequency, duration, and consequences
- History of withdrawal or overdose
7. Family History (Psychiatric and Medical)
- Mental health diagnoses in family
- Family medical history
- Substance use, suicide, violence, or chronic illness
8. Social and Developmental History
- Childhood and upbringing
- Education, employment, housing
- Legal issues, trauma history, support systems
9. Mental Status Examination (MSE)
- Appearance and behavior
- Mood and affect
- Speech and thought process
- Cognition
- Insight and judgment
- Suicidal/homicidal ideation
10. Diagnosis
- DSM-5 diagnoses (primary and secondary)
- Rule-outs, differential, or provisional diagnoses
11. Clinical Formulation and Psychiatric Impression
- Summary of key findings
- Biopsychosocial understanding of the case
- Level of care justification (e.g., outpatient vs. intensive outpatient vs. inpatient)
12. Treatment Plan
- Medication recommendations and rationale
- Therapy referrals or treatment modality
- Lab tests or diagnostic workup (e.g., CBC, metabolic panel, thyroid function)
- Safety planning (if applicable)
- Follow-up schedule
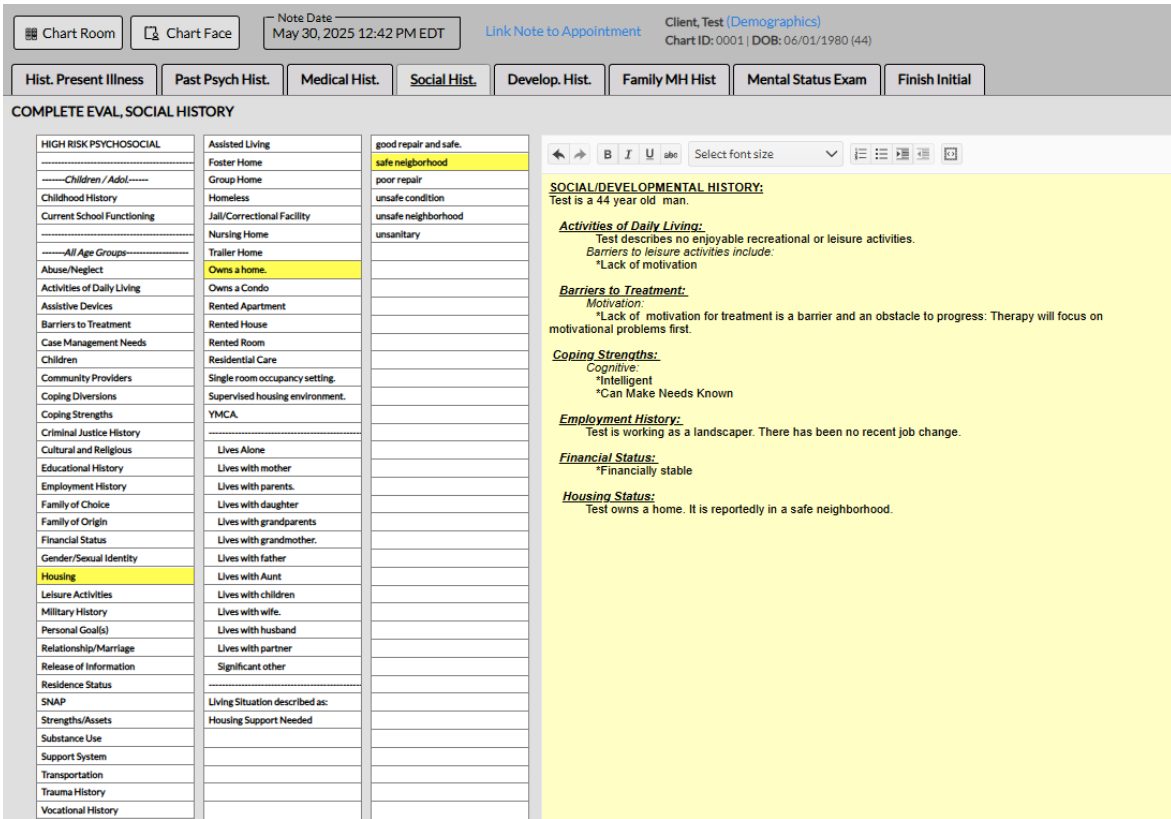
This is the Social History section of the inital psychiatric evaluation template in ICANotes. Comprehensive multi-level menus organized in a clinically logical way allow the psychiatrist or nurse practitioner to quickly produce a detailed narrative.
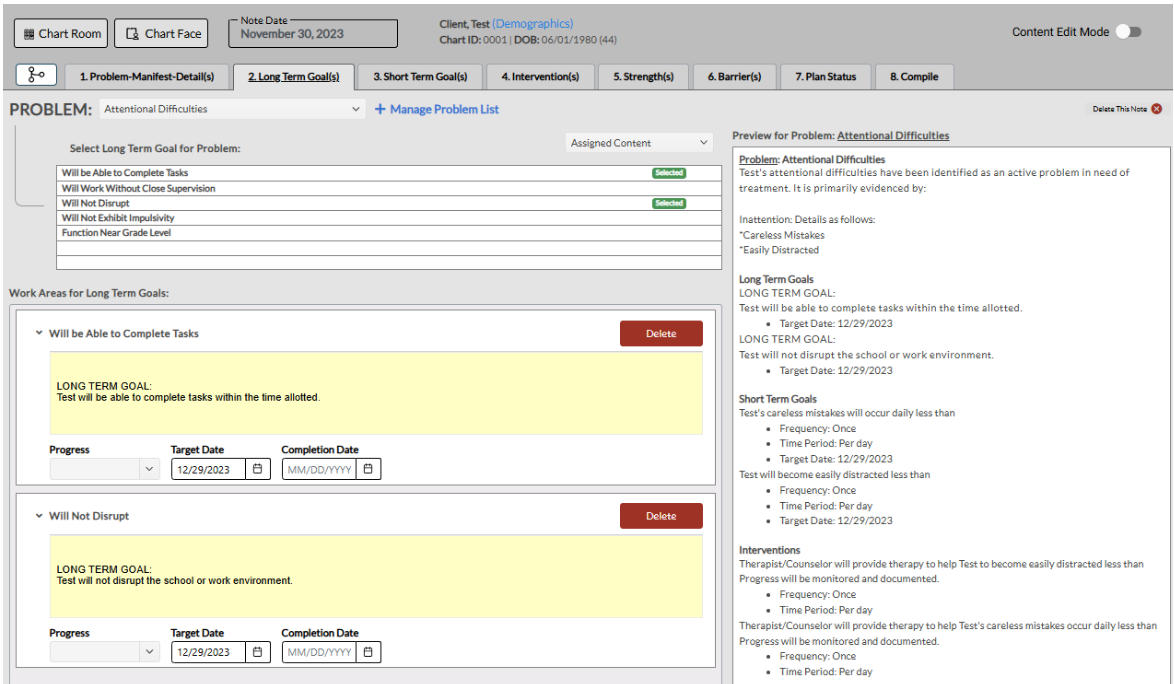
The Treatment Plan module in ICANotes contains robust clinical content for 90 common psychiatric problems and their manifestations. It also includes a wide range of long-term and short-term goals and intervention options.
13. CPT Codes and Billing
-
Service codes appropriate for the visit (e.g., 90791, 99205)
- Ensure documentation support medical necessity and complexity level
Why a Comprehensive Psychiatric Evaluation Template Matters
A comprehensive, consistent psychiatric assessment template ensures nothing critical is overlooked, while also:
- Supporting billing and documentation compliance (e.g., justifying level-of-service codes)
- Improving interdisciplinary communication
- Enhancing clinical decision-making through better data capture
- Reducing risk of liability by including key safety assessments
How ICANotes Helps You Document Initial Psychiatric Evaluations More Efficiently
ICANotes was built specifically for behavioral health professionals—including psychiatrists and psychiatric nurse practitioners. Its menu-driven initial evaluation template is designed to streamline documentation while maintaining the highest clinical standards.
With ICANotes, you can:
- Use click-to-insert narrative content that aligns with clinical phrasing and DSM-5 criteria
- Auto-populate relevant fields from patient history to reduce redundancy
- Seamlessly generate PDF reports that are professional, shareable, and audit-ready
- Access built-in MSE tools, risk assessments, rating scales, and diagnostic libraries
- Customizable templates for specific populations or specialties (e.g., geriatrics, addiction, child psychiatry)
- Automatically determine the highest reimbursable CPT code based on the content of your note
- Order labs directly through integrated lab workflows or document lab needs in your treatment plan
- Justify level of care with structured clinical formulation fields that support medical necessity
- Ease the burden of PDMP checks with seamless integration into state databases during the e-prescribing workflow
The result? You spend less time writing and more time focused on patient care—without sacrificing the depth or quality of your documentation.
Conclusion
A well-structured initial psychiatric evaluation template isn't just a documentation tool—it's a clinical asset. By standardizing the intake process and ensuring completeness, you improve outcomes, reduce risk, and support continuity of care.
With ICANotes, you don’t have to choose between efficiency and thoroughness. Our intelligent templates help you deliver exceptional documentation—fast.
Want to see a sample psychiatric evaluation created in ICANotes?
Download our Initial Psychiatric Evaluation Example PDF and explore how ICANotes can help you streamline your documentation without cutting corners.
Schedule a Live Demo
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals—built to streamline documentation, improve compliance, and enhance patient care.
- Simplify clinical charting
- Stay organized with appointment scheduling
- Reduce no-shows with automated reminders
- Improve client engagement with a secure patient portal
- Provide flexible care with HIPAA-compliant telehealth
Simplify clinical charting
Stay organized with appointment scheduling
Reduce no-shows with automated reminders
Improve client engagement with a secure patient portal
Provide flexible care with HIPAA-compliant telehealth
Frequently Asked Questions
Related Posts
Dr. October Boyles is a behavioral health expert and clinical leader with extensive expertise in nursing, compliance, and healthcare operations. With a Doctor of Nursing Practice (DNP) from Aspen University and advanced degrees in nursing, she specializes in evidence-based practices, EHR optimization, and improving outcomes in behavioral health settings. Dr. Boyles is passionate about empowering clinicians with the tools and strategies needed to deliver high-quality, patient-centered care.