Blog > Treatment Strategies > EMDR Effectiveness: How EMDR Trauma Therapy Works
EMDR Effectiveness: How EMDR Trauma Therapy Works for Trauma Recovery
EMDR effectiveness has been widely demonstrated in trauma treatment, making Eye Movement Desensitization and Reprocessing (EMDR) one of the most researched and trusted therapies for PTSD and trauma-related conditions. EMDR trauma therapy works by helping the brain reprocess distressing memories through bilateral stimulation, reducing emotional intensity and restoring adaptive functioning. In this post, we explore EMDR therapy effectiveness, how EMDR trauma treatment works neurologically, and why it continues to be a first-line intervention for trauma recovery.

Last Updated: December 22, 2025


What You'll Learn
-
What research shows about EMDR effectiveness for trauma and PTSD
-
How EMDR trauma therapy works to reprocess distressing memories
-
Why EMDR trauma treatment is considered a first-line intervention for trauma recovery
-
How the eight phases of EMDR support measurable clinical outcomes
-
What makes EMDR therapy effective for both single-incident and complex trauma
-
How to document EMDR trauma treatment and progress clearly in clinical notes
Contents
- How EMDR Works: The Science Behind Bilateral Stimulation
- The Eight Phases of EMDR Therapy
- EMDR Effectiveness: What the Research Says About EMDR Trauma Treatment
- EMDR Trauma Therapy in Clinical Practice
- Frequently Asked Questions About EMDR Effectiveness
- Documenting EMDR Sessions in ICANotes
- Final Thoughts on EMDR Effectiveness
What Is EMDR Trauma Therapy?
Eye Movement Desensitization and Reprocessing (EMDR) is an evidence-based psychotherapy best known for its effectiveness in treating trauma. EMDR trauma therapy helps clients reprocess distressing memories that remain “stuck” in the nervous system, often driving symptoms such as hypervigilance, intrusive thoughts, emotional dysregulation, and avoidance. By addressing trauma at both the neurological and emotional levels, EMDR trauma treatment supports lasting symptom relief and improved functioning.
Rather than focusing primarily on verbal processing, EMDR uses bilateral stimulation — such as guided eye movements, tapping, or alternating auditory tones — to help clients reprocess traumatic material in a safe and controlled way.
The underlying premise is that trauma overwhelms the brain’s natural processing system, leaving painful memories “stuck” in their original sensory and emotional intensity. EMDR helps unlock and reprocess those memories, enabling new, adaptive associations and reducing emotional distress.
Today, EMDR is recognized as one of the most effective and well-researched trauma treatments available, endorsed by the World Health Organization (WHO), the American Psychiatric Association (APA), and the U.S. Department of Veterans Affairs.
How EMDR Works: The Science Behind Bilateral Stimulation
To understand how EMDR works, it helps to visualize the brain’s natural information-processing system. Under typical circumstances, the brain digests and integrates experiences over time — similar to how we consolidate memories during REM sleep.
Traumatic experiences, however, can disrupt this process. The brain essentially “freezes” the distressing event in raw form — complete with images, body sensations, beliefs, and emotions. These unprocessed fragments can then resurface in the form of flashbacks, hypervigilance, or emotional reactivity.
During EMDR, bilateral stimulation activates both hemispheres of the brain while the client focuses briefly on the traumatic memory. This dual attention — partly in the past, partly in the present — helps the nervous system complete the processing that was interrupted by trauma.
Many researchers believe bilateral stimulation facilitates communication between the amygdala (which processes threat), the hippocampus (which contextualizes memory), and the prefrontal cortex (which regulates emotion and perspective). In short, EMDR allows the brain to “re-file” a memory correctly so it no longer feels dangerous.
Clinically, clients often report that distressing images or sensations fade, and new, positive beliefs emerge in their place — like moving from “I’m powerless” to “I survived” or “and I’m strong.”
The Eight Phases of EMDR Therapy
EMDR therapy follows a structured, eight-phase protocol that provides consistency and safety for both clinician and client. Each phase builds upon the previous one to ensure the client is fully prepared before engaging in trauma reprocessing.
1. History Taking and Treatment Planning
The clinician gathers a detailed clinical history and identifies target memories. This includes assessing the client’s readiness, determining which experiences to reprocess, and creating a treatment plan that prioritizes safety and stability.
2. Preparation and Building Safety
In this phase, therapists teach grounding and self-soothing skills, ensuring clients have tools to regulate emotions during reprocessing. This might include safe-place visualization, deep breathing, or tactile grounding exercises.
3. Assessment of Target Memories
The clinician identifies the specific image or memory associated with the trauma, the negative belief about self (“I’m not safe”), a desired positive belief (“I can protect myself now”), and physical sensations linked to the event. The client rates two key metrics:
- SUD (Subjective Units of Distress) to measure distressing emotional intensity
- VOC (Validity of Cognition) to rate belief in the new positive statement
4. Desensitization and Bilateral Stimulation
While focusing on the target memory, the client follows the therapist’s cues for eye movements, taps, or tones. After each set, the client reports any new thoughts, feelings, or sensations that arise. The process continues until the distress level significantly decreases, a 0 or 1 on the SUDs scale.
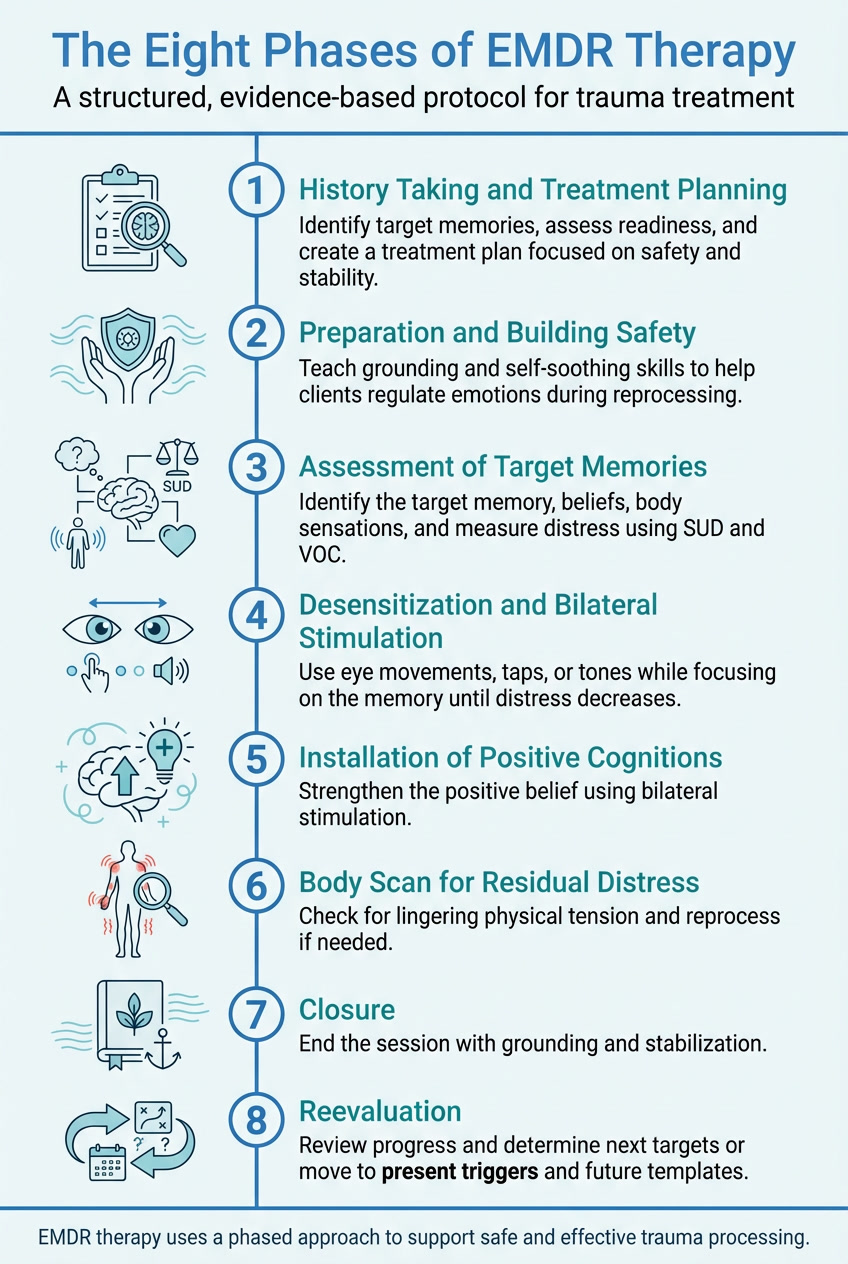
5. Installation of Positive Cognitions
Once the target memory no longer feels distressing, the clinician strengthens the positive belief. The client focuses on this belief while engaging in additional bilateral stimulation to reinforce it somatically and neurologically.
6. Body Scan for Residual Distress
The therapist guides the client to notice any lingering tension or discomfort in the body while recalling the event and positive cognition. If physical distress remains, additional reprocessing may occur.
7. Closure
Each session ends with grounding and stabilization to ensure the client feels safe leaving the session. The therapist may revisit self-soothing exercises or encourage journaling to monitor thoughts between sessions.
8. Reevaluation
At the start of the next session, the clinician assesses whether the previous target remains resolved or needs further reprocessing. If the prior target is resolved, the clinician identifies a new area for reprocessing. This phase helps evaluate progress and guide future treatment planning. If there are no new targets to address from this traumatic event, the clinician can move on to the second and third prongs of EMDR therapy — Present Triggers and Future Templates.
EMDR Effectiveness: What the Research Says About EMDR Trauma Treatment
EMDR effectiveness is supported by decades of clinical research and is widely recognized across international treatment guidelines. Multiple randomized controlled trials and meta-analyses have shown that EMDR trauma treatment is highly effective for reducing symptoms of post-traumatic stress disorder (PTSD), often in fewer sessions than other trauma-focused therapies. As a result, EMDR therapy effectiveness has been endorsed by organizations such as the World Health Organization (WHO), the American Psychiatric Association (APA), and the U.S. Department of Veterans Affairs.
Key Findings from the Research
- A 2013 meta-analysis published in PLoS ONE found EMDR produced significant reductions in PTSD symptoms, often in fewer sessions than CBT.
- The Journal of EMDR Practice and Research reports that between 77–90% of clients with single-event trauma no longer meet PTSD criteria after 3–6 sessions.
- The World Health Organization and U.S. Department of Veterans Affairs both list EMDR as a first-line treatment for PTSD in adults and children.
Beyond PTSD, EMDR has shown promise for a range of conditions, including anxiety, depression, phobias, chronic pain, and complex trauma. Its structured format and body-focused integration make it especially useful for clients who struggle with verbalizing trauma narratives.
EMDR Trauma Therapy in Clinical Practice
In real-world clinical settings, EMDR often complements other trauma-informed modalities. Clinicians integrate EMDR with approaches like DBT, IFS, or somatic therapy to tailor care for complex trauma presentations. In everyday clinical settings, EMDR trauma therapy is especially effective for clients who understand their trauma cognitively but continue to experience intense emotional or somatic responses. EMDR trauma treatment helps bridge this gap by engaging the brain’s natural information-processing system rather than relying solely on verbal insight.
The therapist’s attunement and pacing are crucial. Not every client is immediately ready for trauma reprocessing; stabilization, affect regulation, and psychoeducation may be needed first.
EMDR can be particularly powerful in cases where clients understand the trauma intellectually but continue to feel it viscerally. By engaging both cognitive and sensory pathways, EMDR helps bridge that gap, creating lasting change at both the emotional and neurological levels.
In everyday clinical settings, EMDR trauma therapy is especially effective for clients who understand their trauma cognitively but continue to experience intense emotional or somatic responses. EMDR trauma treatment helps bridge this gap by engaging the brain’s natural information-processing system rather than relying solely on verbal insight.
Frequently Asked Questions About EMDR Effectiveness
Documenting EMDR Sessions in ICANotes
Accurate documentation of EMDR trauma treatment is essential for demonstrating medical necessity, tracking clinical outcomes, and supporting the documented effectiveness of EMDR therapy over time.
High-quality documentation is essential when delivering EMDR, not only for clinical continuity but also for medical necessity and compliance.
ICANotes helps clinicians document EMDR sessions accurately and efficiently with structured, behavioral-health-specific templates that align with EMDR’s eight-phase model. Here’s how clinicians can streamline EMDR documentation within ICANotes:
- Use customizable progress note templates to capture each EMDR phase, including session targets, triggers, and desensitization responses.
- Track SUD and VOC scores directly in notes to document measurable progress.
- Integrate treatment plans and progress updates seamlessly with ongoing documentation to demonstrate clinical rationale and outcomes.
- Ensure defensible, compliant records with structured phrasing that supports medical necessity for trauma treatment.
- Collaborate across teams with secure, cloud-based access and HIPAA-compliant sharing of client progress.
With ICANotes, EMDR therapists can spend less time typing and more time focusing on attunement, pacing, and clinical connection.
Final Thoughts on EMDR Effectiveness
EMDR therapy offers clinicians a structured yet deeply transformative way to help clients heal from trauma. By combining neuroscience, mindfulness, and evidence-based structure, EMDR allows the brain to complete what trauma once interrupted — helping clients reclaim safety, self-trust, and resilience.
And with ICANotes, documenting EMDR sessions becomes faster, clearer, and more compliant. The platform’s behavioral-health-specific design ensures every note reflects your professional skill while supporting ethical and evidence-based care.
Related Posts
About the Author
Barbara Sheehan-Zeidler, MA, LPC, is the owner of Creative and Caring Counseling in Littleton, Colorado. She is an EMDR Trainer, EMDRIA-Approved Consultant, and Certified EMDR Therapist with advanced training in trauma-focused modalities including Internal Family Systems (IFS), IFS Somatic Therapy, AEDP, Polyvagal Theory, Sandplay, and Natural Processing. Barbara brings a relational, collaborative, and mindful approach to trauma healing and regularly presents at local and international conferences, offering training and consultation to clinicians and agency leaders.






