Blog > Treatment Strategies > Addiction and Family Systems: Understanding Roles and Recovery
Addiction and Family Systems: How Clinicians Can Support the Whole Family
Addiction and family systems are deeply interconnected. When substance use destabilizes a household, family roles shift, communication breaks down, and patterns of enabling or conflict emerge. Using family systems theory, clinicians can better understand these dynamics, identify maladaptive roles, and guide families toward healthier boundaries, improved resilience, and more sustainable paths to recovery.
Last Updated: November 17, 2025


What You'll Learn
- How family systems theory explains addiction and family dynamics
- Common roles in addicted family systems and how they perpetuate dysfunction
- The difference between support and enabling
- Practical tools drawn from IFS, CBT, and DBT for family-focused treatment
- How ICANotes simplifies documentation for family systems approaches
The Family Systems Model of Addiction
Developed by psychiatrist Dr. Murray Bowen, family systems theory views the family as an interconnected emotional unit. Within this model, individual behavior cannot be understood in isolation, it is a reflection of the family’s relational dynamics.
When one family member struggles with addiction, the entire system shifts to adapt. Roles change, alliances form, and unspoken rules emerge in an attempt to restore stability. Unfortunately, these adaptations, though rooted in survival, often reinforce the very patterns that maintain the addiction.
Understanding the family systems model of addiction allows clinicians to move beyond an individual-focused lens. Instead, therapy targets the whole ecosystem: communication, boundaries, coping patterns, and intergenerational transmission of trauma.
The Addicted Family System in Motion
Families affected by addiction function much like a crew in a small boat caught in a relentless storm.
“The addicted person may be gripping the wheel, but the storm, fueled by substance use, thrashes everyone aboard.”
Some family members desperately bail water, others try to steer, and some freeze or pretend nothing is wrong. Tensions rise, exhaustion sets in, and blame becomes the loose cargo that’s thrown around to survive another day.
In this metaphor, the therapist is the lighthouse keeper — not calming the storm, but teaching the family to read the waves, recognize dangerous patterns, and chart safer courses together. This image captures the essence of the family systems approach to addiction: guiding families toward healthier rhythms of communication, boundaries, and shared purpose.
Common Roles in Addicted Family Systems
When addiction infiltrates the home, family members often adopt distinct psychological roles to maintain equilibrium. These roles, while adaptive in the short term, ultimately reinforce dysfunction.
| Role | Description | Clinical Insight |
|---|---|---|
| The Addicted Person | The individual whose substance use becomes the organizing principle of the family system. | Acts as the symptom bearer; the family’s emotional energy unconsciously revolves around their behavior. |
| The Enabler | Protects the addicted member from consequences by covering up, rescuing, or minimizing problems. | Motivated by love and fear but inadvertently maintains the addiction by removing accountability. |
| The Hero | The high achiever who compensates for chaos by being “perfect” in academics, work, or appearance. | Often struggles with anxiety, overfunctioning, and guilt while holding the family’s emotional weight. |
| The Scapegoat | Acts out, rebels, or engages in disruptive behavior that diverts attention from the true family problem. | Frequently seen as the “identified patient” in therapy, even though their behavior reflects deeper systemic dysfunction. |
| The Lost Child | Withdraws emotionally, avoids conflict, and becomes “invisible” within the family system. | Appears self-sufficient but often experiences profound loneliness, neglect, and disconnection. |
| The Mascot | Uses humor, charm, or lightheartedness to diffuse tension and distract others from pain. | Masks deep fear or sadness; relies on distraction as a coping mechanism within chaotic environments. |
These roles in addicted family systems are fluid, family members may move between them depending on stressors or stages of the addiction cycle. Identifying and naming these dynamics in therapy helps families understand their patterns with compassion rather than blame.

Tip
Distinguishing between support and enabling is crucial for families navigating the storm of addiction
The Codependent Cycle
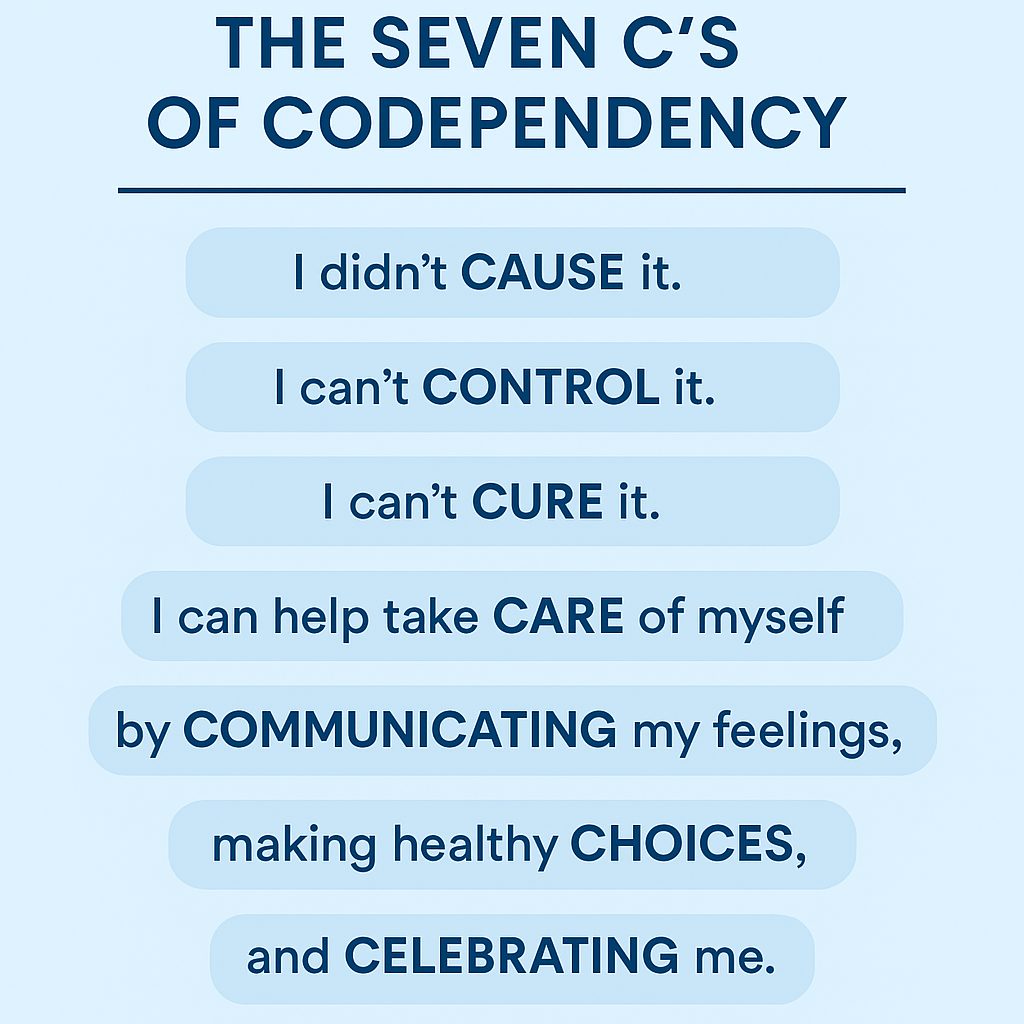
As addiction progresses, families often fall into codependent patterns: cycles of rescuing, controlling, or self-sacrifice that blur the line between love and enablement. Melody Beattie’s Codependent No More remains a cornerstone resource in this work, defining codependency as “a system of thinking, feeling, and behaving that keeps people focused on others’ problems rather than their own well-being.”
Clinicians can use the Seven C’s as a psychoeducational tool to help family members reframe their relationship to addiction.
This simple framework encourages clients to replace guilt and over-responsibility with self-compassion and autonomy. As one family therapist put it during the Supporting the Family in Navigating Addiction webinar:
“Do not set yourself on fire to keep others warm.”
Internal Family Systems (IFS) and Addiction
Internal Family Systems (IFS) therapy extends family systems principles inward, recognizing that each individual contains an “internal family” of parts — protectors, exiles, and managers — that interact much like members of a household.
In addiction treatment, IFS helps both clients and family members:
- Identify the protective parts that turn to substances or control behaviors for safety.
- Cultivate Self-energy — the calm, compassionate core that can lead with curiosity rather than judgment.
- Reduce polarization between family members by modeling internal harmony externally.
When clinicians integrate IFS and addiction work, they help families see that healing doesn’t come from eliminating parts, or people, but from understanding and reintegrating them.
Why Families Hesitate to Seek Help
Despite the pervasive impact of addiction, families often avoid therapy. Common barriers include:
- Shame and stigma (“We should handle this ourselves.”)
- Fear of exposure of family secrets or trauma
- Cultural norms discouraging external help
- Denial (“The real problem is the substance user, not us.”)
- Learned helplessness and fatigue
As clinicians, normalizing these reactions and reframing therapy as a collective path to healing, not blame, can open the door to engagement.
Clinical Strategies for Working with the Addicted Family System
A family systems approach to addiction therapy requires flexibility, empathy, and structural awareness. Effective interventions may include:
1. Psychoeducation
Before setting goals or interventions, ensure the family understands addiction as a systemic issue. Use visual metaphors, genograms, and role maps to illustrate dynamics.
2. Motivational Interviewing (MI)
Meet each family member where they are in the change process. A parent in denial requires a different approach than a sibling ready to set boundaries.
3. Cognitive Behavioral Therapy (CBT)
Identify automatic thoughts that sustain guilt and control (“If I don’t help, they’ll die”) and replace them with more adaptive cognitions (“I can love them and still protect my peace”).
4. Dialectical Behavior Therapy (DBT)
Use dialectical statements, “I love you and I won’t fund your addiction,” to help families hold compassion and limits simultaneously.
5. Gestalt Empty Chair Technique
Encourage family members to speak directly, even symbolically, to the loved one with addiction. This can release repressed emotions and foster closure when contact is limited.
6. Avoiding Triangulation
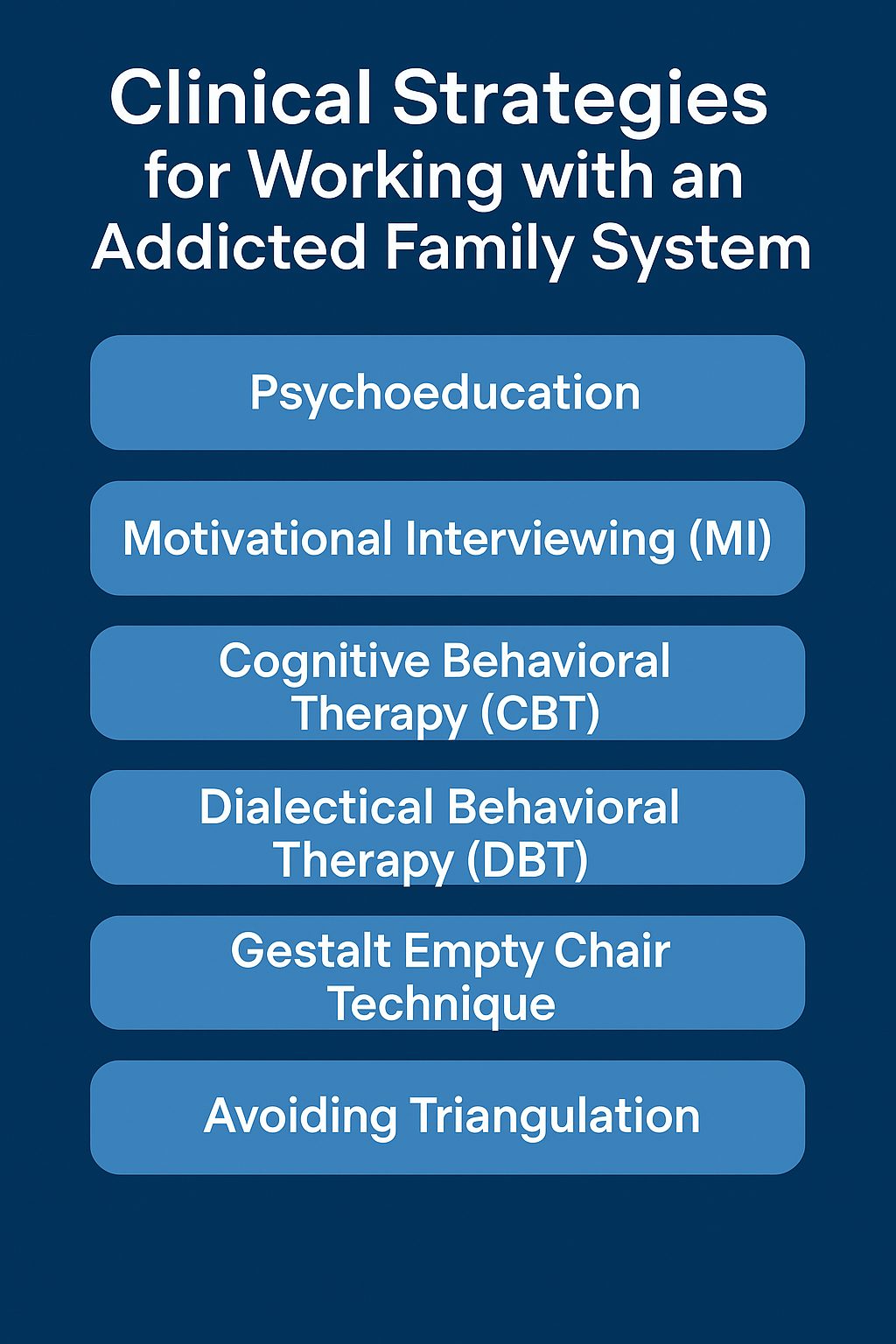
Stay alert to being pulled into family alliances. Maintain neutrality and model balanced boundaries to prevent reenacting the family’s internal conflict within the therapeutic relationship.
The Family’s Path to Recovery
Not every family’s journey ends with the addicted person achieving sobriety, but the family can still heal. Recovery for families means:
- Rebuilding self-identity apart from the addiction narrative
- Establishing consistent boundaries and emotional safety
- Seeking community support (e.g., Al-Anon, SMART Recovery Family & Friends, or NAMI Family-to-Family)
- Practicing mindfulness and self-compassion
- Developing realistic hope rather than false control
Clinicians can reinforce that recovery is relational, not conditional: the family’s wellness does not have to depend on the addicted person’s choices.
Documenting Family Systems Work in ICANotes
Delivering systemic therapy is complex, but documenting it doesn’t have to be. ICANotes provides specialized tools for clinicians using a family systems approach:
- Family & Couples Therapy Note Template: Prebuilt fields capture session focus, family roles, boundary setting, and engagement levels.
- Treatment Plan Integration: Link treatment plan goals directly to identified systemic patterns such as enabling, communication deficits, or boundary issues.
- Private Note Functionality: Record sensitive observations (e.g., triangulation, role shifts) without sharing them in client-facing summaries.
- Progress Tracking: Structured data fields simplify outcome monitoring for ongoing family work.
For clinicians using approaches like IFS and addiction or CBT-based family interventions, ICANotes streamlines documentation while preserving clinical nuance — helping you stay compliant, efficient, and therapeutically aligned.

Tip
Healing begins when families learn to see their patterns clearly, communicate authentically, and establish healthy boundaries rooted in love rather than fear.
Books and Continuing Education for Clinicians
- Beattie, M. (1986). Codependent No More: How to Stop Controlling Others and Start Caring for Yourself.
- Bowen, M. (1978). Family Therapy in Clinical Practice.
- Schwartz, R. (2021). No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems Model.
- Wegscheider-Cruse, S. (1989). Another Chance: Hope and Health for the Alcoholic Family.
To deepen your understanding of the family systems model of addiction and strengthen your therapeutic toolkit, consider the following continuing education opportunities:
- Diane Bigler, LCSW, LSCSW — Diane’s engaging and clinically grounded workshops explore topics such as Addiction and the Family System, Trauma and Resilience, and Supporting Families in Recovery. Her CE classes emphasize practical, evidence-based strategies for applying family systems theory in addiction treatment and can be found through leading CEU platforms such as PESI and Allied Behavioral Health CE.
These CE resources allow clinicians to translate theory into action, integrating systems-based insight with efficient, ethical, and compliant clinical workflows.
Frequently Asked Questions
Conclusion: From Chaos to Connection
The family systems theory perspective reminds us that addiction is never just one person’s illness, it’s a systemic wound. Healing begins when families learn to see their patterns clearly, communicate authentically, and establish healthy boundaries rooted in love rather than fear.
By integrating evidence-based frameworks like IFS, CBT, and DBT, clinicians can guide families from reactive cycles toward relational balance. And with tools like ICANotes, documenting that progress across individuals, couples, and families becomes seamless.
Ultimately, the work of supporting families through addiction is less about fixing what’s broken and more about helping them rediscover their capacity to navigate life’s storms together.
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
- Complete Notes in Minutes - Purpose-built for behavioral health charting
- Always Audit-Ready – Structured documentation that meets payer requirements
- Keep Your Schedule Full – Automated reminders reduce costly no-shows
- Engage Clients Seamlessly – Secure portal for forms, messages, and payments
- HIPAA-Compliant Telehealth built into your workflow
Complete Notes in Minutes – Purpose-built for behavioral health charting
Always Audit-Ready – Structured documentation that meets payer requirements
Keep Your Schedule Full – Automated reminders reduce costly no-shows
Engage Clients Seamlessly – Secure portal for forms, messages, and payments
HIPAA-Compliant Telehealth built into your workflow
Related Posts
About the Author
Diane Bigler, LCSW, LSCSW, is a Licensed Clinical Social Worker in Missouri and Kansas with over 25 years of experience in the mental health field. She has held clinical positions as an outpatient and in-home therapist and clinical supervisor in diverse settings. Diane was an Adjunct Professor of Social Work for 10 years at The University of Kansas, School of Social Welfare and a Field Liaison and Field Instructor. She has also held administrative positions as a Program Director and Coordinator. Diane is a popular local and national trainer on a wide variety of mental health and workplace development topics for clinicians and corporations and has facilitated over 500 training courses in the last few years. Visit her website http://www.







