Blog > Documentation > How to Write a Clinical Summary for Mental Health (Examples and Templates)
How to Write a Clinical Summary for Mental Health (Examples & Templates)
This guide walks you through exactly how to write a clinical summary for mental health care — from key elements to include, to formatting tips, to avoiding common pitfalls. You’ll see a mental health clinical summary example and a ready-to-use clinical summary template that can streamline your documentation, improve communication with other providers, and strengthen billing and compliance. Whether you’re a therapist, psychiatrist, or case manager, this resource will help you create summaries that are clear, defensible, and aligned with best practices, saving you time while enhancing continuity of care.

Last Updated: September 12, 2025


What You'll Learn
- Understand what a clinical summary is and why it matters in mental health care
- Follow step-by-step guidance on how to write a clinical summary that is clear and defensible
- Review a mental health clinical summary example to see best practices in action
- How to streamline summaries for care coordination, billing, and compliance
Contents
- Why a Clinical Summary is Essential for Continuity of Care
- Key Elements of a Mental Health Clinical Summary
- How to Write a Clinical Summary Step by Step
- Compliance, Billing, and Risk Management Benefits of Clinical Summaries
- FAQ: Clinical Summaries
- Conclusion: Writing Better Clinical Summaries with ICANotes
As the Chief Clinical Officer at ICANotes, there are many features in our platform that I genuinely love — but one of the most powerful and underutilized tools in our behavioral health EHR system is the Clinical Summary.
What is a Clinical Summary in Mental Health Care?
A clinical summary is a concise, high-level overview of a client’s diagnosis, treatment history, and current progress. In mental health settings, where care often involves a multidisciplinary team — psychiatrists, therapists, nurse practitioners, primary care providers, and case managers — a well-crafted clinical summary ensures everyone is working from the same information.
Why a Clinical Summary is Essential for Continuity of Care
Without a clear summary, clinicians risk repeating assessments, creating fragmented treatment plans, or even delivering conflicting care. A clinical summary for mental health connects the dots across disciplines, ensuring care remains informed, consistent, and client-focused.
Key Elements of a Mental Health Clinical Summary
A strong clinical summary gives you at-a-glance insights into:
- Where the client started
- What interventions have been attempted
- How the client is progressing
- Whether they’re stabilizing, improving, or showing signs of escalation
These details support real-time, evidence-informed decision-making, whether adjusting medications, updating treatment plans, or preparing for a transfer of care.
Mental Health Clinical Summary Example
Sample Template Structure
- Identifying Information – Client name, ID, date of birth
- Presenting Problem – Primary concerns at intake
- Diagnosis – Current DSM-5 diagnoses
- Treatment History – Prior interventions, therapy types, medications
- Progress Summary – Response to treatment, functional improvements, setbacks
- Current Medications – Name, dosage, and prescribing provider
- Next Steps / Recommendations – Planned adjustments or referrals
This mental health clinical summary template can be adapted to your practice needs. Below you can review an example of a complete clinical summary for mental health.

Mental Health Clinical Summary Example
Identifying Information
Client: J.D., Age 32, Female
DOB: 05/17/1993
Client ID: 45821
Date of Summary: 09/09/2025
Clinician: Sarah M., LCSW
Presenting Problem
J.D. presented with symptoms of persistent anxiety, difficulty sleeping, and panic episodes occurring 2–3 times per week. She reported increased stress at work, irritability, and avoidance of crowded environments.
Diagnosis
- Generalized Anxiety Disorder (F41.1)
- Panic Disorder without Agoraphobia (F41.0)
- Rule out: Major Depressive Disorder, recurrent, mild
Treatment History
- Weekly cognitive behavioral therapy (CBT) sessions for 12 weeks
- Completed 6 sessions of mindfulness-based stress reduction group
- Previous trial of sertraline (discontinued due to GI side effects)
- No history of psychiatric hospitalization
Progress Summary
J.D. has demonstrated moderate progress toward treatment goals. She reports fewer panic attacks (1–2 per month vs. weekly at intake), improved ability to use grounding techniques, and reduced work-related absenteeism. Sleep remains disrupted, averaging 5 hours per night. Client continues to avoid large social events, though has successfully attended small gatherings.
Current Medications
- Escitalopram 10 mg daily, prescribed by Dr. K. Johnson, MD (initiated 8/2025)
- Hydroxyzine 25 mg as needed for acute anxiety, prescribed by same provider
Next Steps / Recommendations
- Continue weekly CBT sessions for another 8 weeks with focus on exposure techniques
- Referral to sleep specialist for evaluation of chronic insomnia
- Medication follow-up with prescribing psychiatrist in 6 weeks
- Encourage ongoing practice of relaxation strategies and progressive exposure to social situations
How to Write a Clinical Summary Step by Step
- Collect Key Data – Pull from your compiled notes, treatment plans, and assessments.
- Focus on Relevance – Include only what’s essential for understanding the client’s care trajectory.
- Use Clear, Objective Language – Avoid jargon and overly subjective descriptions.
- Highlight Outcomes – Note progress, setbacks, and responses to treatment.
- Ensure Accuracy and Timeliness – Update summaries regularly to reflect current care.
Why Clinical Summaries Improve Communication
Clinical summaries are also essential for external communication. Whether you’re coordinating with a substance use treatment center, responding to a court order, supporting a disability claim, or communicating with another provider, a well-written clinical summary ensures your documentation is professional, complete, and defensible. It tells the clinical story clearly and responsibly.
Compliance, Billing, and Risk Management Benefits of Clinical Summaries
From a liability and risk management perspective, clinical summaries are your best friend. They show the clinical rationale behind your decisions, not just in a single note, but across the span of care. They demonstrate that the treatment was consistent with best practices and delivered in good faith. In an environment where defensive documentation is increasingly necessary, the clinical summary is a powerful safeguard.
And finally, let’s not forget billing and compliance. Medicare, Medicaid, and many private insurers now expect summaries as part of the documentation that supports medical necessity, level of care, and prior authorization approvals. A strong clinical summary helps justify ongoing services and supports clients in accessing the care they need, while protecting your practice from denials and recoupments. Prior authorization is a frequent requirement for ongoing mental health services. In Medicaid managed care plans, roughly 12.5% of prior authorization requests are denied, with some plans rejecting over 25% (1). A first-quarter CMS report identified top medical review denial causes, with 25% due to services not medically necessary, and 20% due to missing documentation (e.g., lack of timely face-to-face encounter records) (2).
Clinical summaries aren’t just helpful, they’re essential. If you’re not using them regularly, now is the time to start.
Using the ICANotes Mental Health EHR to Create a Clinical Summary
Let me show you how easy it is to create a clinical summary in ICANotes.
From any compiled note in the system, you can easily navigate to the clinical summary by clicking on the Create Clinical Summary button:
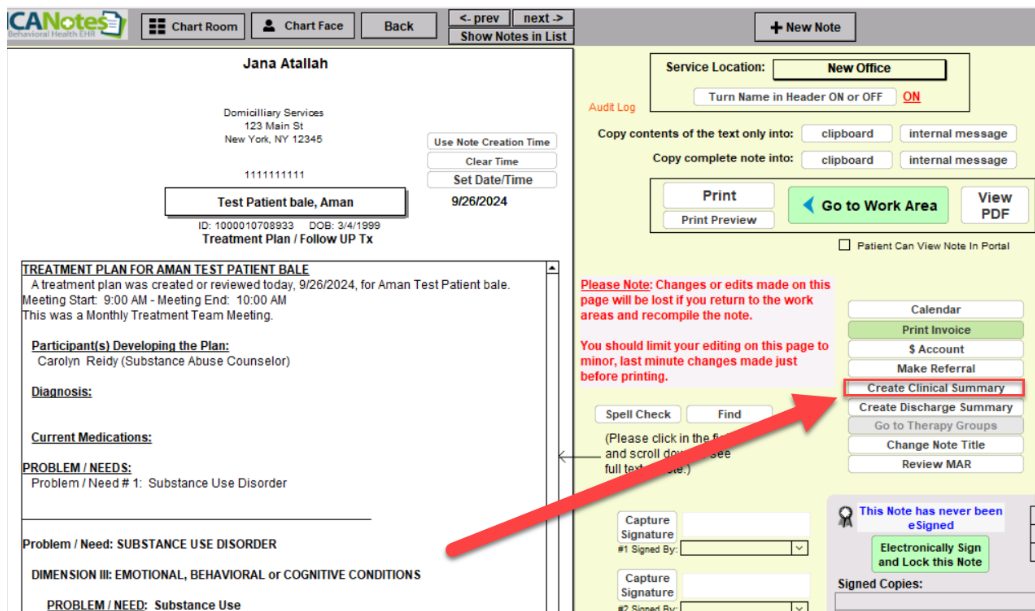
Let me show you how easy it is to create a clinical summary in ICANotes.
From any compiled note in the system you can easily navigate to the clinical summary by clicking on the Create Clinical Summary button:
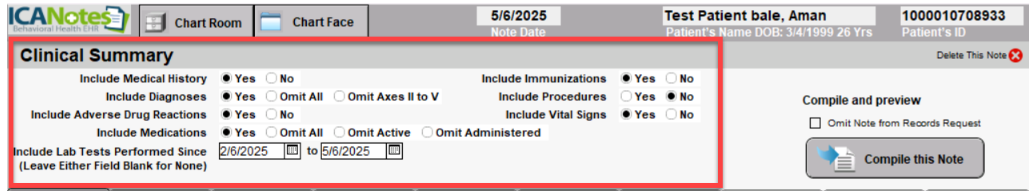
ICANotes then populates all the information into the Clinical Summary work area.
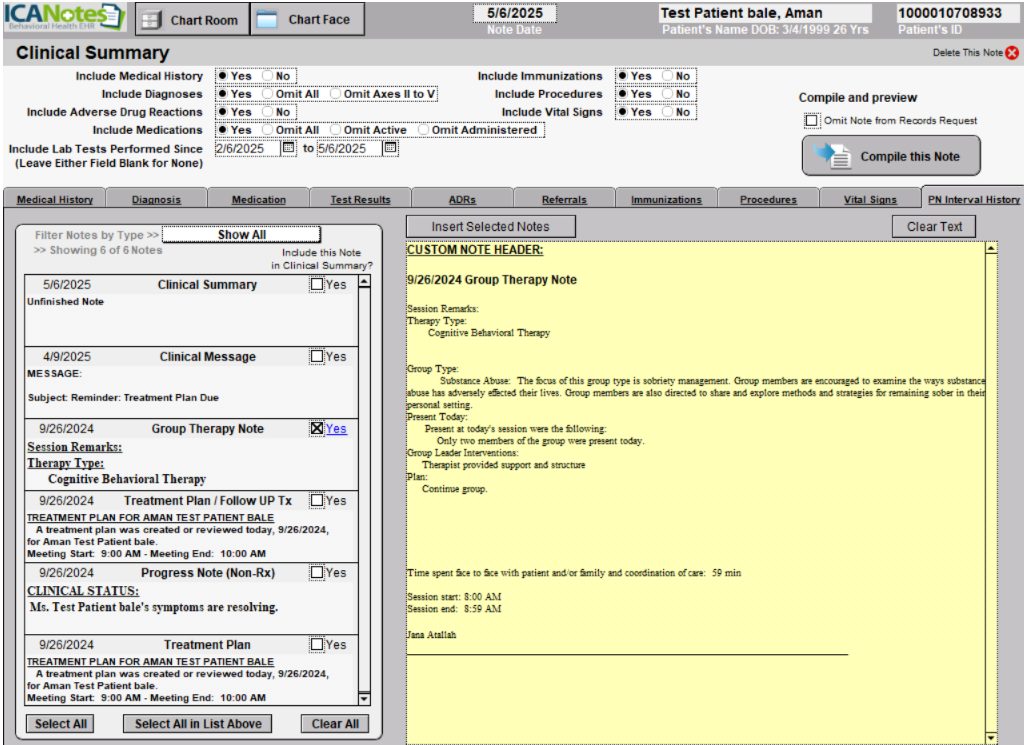
Once compiled, the system brings together all the key information you've selected — diagnoses, treatment history, progress updates, and current medications — into one streamlined clinical summary report. Using clinical summaries will enhance communication with external providers like the client’s primary care doctor, support billing and medical necessity documentation, reduce paperwork for your office, and ensure faster, clearer decision-making across the care team.
Frequently Asked Questions: Clinical Summaries
Conclusion: Writing Better Clinical Summaries with ICANotes
A well-written clinical summary is more than a compliance checkbox — it’s a tool that improves continuity of care, reduces liability, supports billing, and strengthens communication across providers. When done consistently, summaries help clinicians tell the client’s clinical story clearly, responsibly, and in a way that is useful for both treatment planning and administrative requirements.
Yet, writing effective clinical summaries can feel time-consuming and repetitive. That’s where ICANotes makes the difference. Our behavioral health EHR includes a Clinical Summary feature that automatically pulls together the essential elements of care — diagnoses, treatment history, medications, and progress — into a streamlined, professional document. With just a few clicks, clinicians can generate a summary that is accurate, consistent, and ready to share for care coordination, billing, or compliance.
By reducing manual effort and improving documentation quality, ICANotes helps you write better clinical summaries more efficiently, so you can spend less time on paperwork and more time focusing on client care.
Ready to simplify your clinical documentation? Book a demo or register for a free 30-day trial (no credit card required).
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
- Complete Notes in Minutes - Purpose-built for behavioral health charting
- Always Audit-Ready – Structured documentation that meets payer requirements
- Keep Your Schedule Full – Automated reminders reduce costly no-shows
- Engage Clients Seamlessly – Secure portal for forms, messages, and payments
- HIPAA-Compliant Telehealth built into your workflow
Complete Notes in Minutes – Purpose-built for behavioral health charting
Always Audit-Ready – Structured documentation that meets payer requirements
Keep Your Schedule Full – Automated reminders reduce costly no-shows
Engage Clients Seamlessly – Secure portal for forms, messages, and payments
HIPAA-Compliant Telehealth built into your workflow
Related Posts
About the Author
Dr. October Boyles is a behavioral health expert and clinical leader with extensive expertise in nursing, compliance, and healthcare operations. With a Doctor of Nursing Practice (DNP) and advanced degrees in nursing, she specializes in evidence-based practices, EHR optimization, and improving outcomes in behavioral health settings. Dr. Boyles is passionate about empowering clinicians with the tools and strategies needed to deliver high-quality, patient-centered care.