Blog > Treatment Strategies > Trauma Informed Therapy Techniques That Build Trust & Safety
Trauma Informed Therapy Techniques: A Clinician's Guide to Healing Practices
Trauma informed therapy techniques provide clinicians with the framework and tools to help clients process painful experiences safely and effectively. Grounded in principles of safety, empowerment, and trust, these trauma informed interventions can transform the therapeutic relationship — reducing the risk of retraumatization and enhancing emotional regulation. In this guide, you’ll explore evidence-based trauma therapy techniques, therapeutic techniques for trauma, and practical applications you can use right away in session, plus download a free trauma informed care cheat sheet to keep these best practices within reach.

Last Updated: October 9, 2025

What You'll Learn
-
The six core principles that define trauma-informed care
-
How trauma informed therapy techniques differ from traditional approaches
-
Which trauma therapy techniques — including EMDR, TF-CBT, and somatic methods — are most effective
-
How to integrate trauma informed interventions into your practice environment and documentation
-
Ways to apply therapeutic techniques for trauma safely with diverse client populations
Contents
- Six Core Principles of Trauma Informed Care
- The Impact of Trauma on Mental Health
- Evidence-Based Trauma Therapy Techniques
- Integrating Trauma Informed Therapy Techniques into Clinical Settings
- Addressing Secondary Trauma and Burnout in Mental Health Professionals
- Ethical Considerations in Trauma Therapy
- Documentation Best Practices for Trauma Therapy
- FAQs: Trauma-Informed Therapy Techniques and Interventions
- Conclusion: Building a Trauma Informed Practice
Introduction to Trauma Informed Therapy Techniques
Let’s begin with what trauma-informed therapy really means, and why it’s become essential for every behavioral health clinician.
Trauma informed therapy techniques are essential for creating safety, empowerment, and healing in the therapy room. Whether you treat clients with PTSD, anxiety, or complex trauma histories, understanding trauma informed interventions allows you to meet clients where they are — without retraumatizing or overwhelming them.
In this guide, you’ll explore:
-
The six core principles of trauma-informed care
-
Evidence-based trauma therapy techniques like EMDR and TF-CBT
-
Therapeutic techniques for trauma that restore agency and trust
-
A downloadable trauma informed care cheat sheet for everyday reference
The need for trauma informed therapy techniques stems from the reality that we all know too well — the majority of those we serve are navigating the impact of traumatic experiences from their past. In fact, 70% of adults in the U.S have experienced some type of traumatic event at least once in their lives. Regardless of your area of specialty, understanding and applying the principles of trauma informed care will not only enhance your practice but also allow you to incorporate these essential skills into your daily sessions, ultimately helping your clients achieve a better quality of life.
What is Trauma Informed Therapy?
Trauma-informed therapy isn’t a modality — it’s a mindset that integrates safety, choice, collaboration, and empowerment into all aspects of care. Instead of asking “What’s wrong with you?” the trauma-informed clinician asks, “What happened to you, and how did you survive?”
This approach emphasizes:
-
Recognizing the prevalence and impact of trauma
-
Understanding the neurobiological and emotional effects of traumatic stress
-
Creating environments where both clinician and client feel safe
-
Building trust and transparency throughout treatment
| Principle | Clinical Application | Therapist Reminder |
|---|---|---|
| Safety | Create a physically and emotionally safe environment; set clear boundaries and predictable routines. | “How can I help my client feel safe today?” |
| Trust & Transparency | Explain what you’re documenting, why questions are asked, and how information will be used. | “Did I communicate expectations clearly?” |
| Peer Support | Offer referrals to peer networks or support groups; integrate lived-experience perspectives when appropriate. | “Am I offering opportunities for connection?” |
| Collaboration | Share decision-making power; invite clients to set pace, goals, and intervention choices. | “Am I partnering or directing?” |
| Empowerment | Highlight strengths and resilience; reinforce skills that increase autonomy and self-efficacy. | “Did I highlight what’s working?” |
| Cultural Humility | Respect cultural, gender, and identity differences in trauma expression and healing; adapt care accordingly. | “Am I aware of my own biases?” |
Six Core Principles of Trauma Informed Care
Trauma-informed care is based on six core principles that guide and direct treatment. With these principles in mind, therapists will be able to address traumatic experiences with confidence and competency.
The 6 principles of trauma informed care are:
- Safety. Your clients have to feel safe throughout every step of this vulnerable treatment process. Not only that, but the therapist must feel the same. Dealing with trauma is an extremely intense and challenging process, so all parties must feel supported during the discomfort. Having sound supervision and institutional support is essential for this.
- Trustworthiness and Transparency. Trauma can destroy trust, for this reason, developing a trusting foundation is essential in an effective care setting. Therapists and other staff should behave in transparent and consistent ways to benefit the clients. When difficult treatment decisions are made, it should be clear why these choices are made and the expected outcomes they hope to achieve, bringing the client alongside in decision making whenever possible.
- Peer Support. Trauma symptoms should improve with good therapy, however having additional support outside of session is essential to long-term healing. Attending support groups, connecting with friends and family, and even exploring new hobbies are all part of trauma-informed care interventions.
- Collaboration. Power differences often lead to trauma and similar power differences may present in therapy. Building a model that facilitates collaboration between the client and therapist can enhance feelings of trust and the client’s perceptions about their own abilities.
- Empowerment. When a client feels a sense of control over their life, they can thrive. Increasing feelings of confidence and self-determination can increase a client’s ability to problem solve, navigate difficulties, utilize their coping skills, and become resilient.
- Humility and Responsiveness. Therapists who are practicing from a trauma-informed lens are able to determine when they are and are not the experts in a given situation. This practice of humility and awareness is essential to remaining unbiased. Within the therapy setting, a professional should constantly be working to understand their client’s experience from their perspective, remaining attuned and responsive throughout each session.

Bring Trauma-Informed Care Principles to Life in Every Session
Download our Trauma-Informed Care Cheat Sheet — a practical, clinician-designed reference that helps you:
✅ Ensure safety, trust, and empowerment in every interaction
✅ Prevent retraumatization with structured, evidence-based care
✅ Integrate cultural awareness and collaboration into treatment
✅ Stay grounded with self-reflection prompts and session checklists
It’s a quick, printable guide that turns theory into actionable practice — so you can deliver trauma-informed care with confidence, compassion, and clinical precision.
The Impact of Trauma on Mental Health
Trauma sources and trauma symptoms are widely diverse and will manifest differently from person to person. Some trauma may stem from a single acute source, like a car accident or an incident of physical assault, while other times trauma will develop from chronic exposure to high stress, abuse, or victimization, like military combat or abusive relationships. Some people will have just one type of trauma, while many others will have a series of varied traumatic experiences, also known as “compound trauma.”
The negative impact of trauma on a person’s physical, mental, and spiritual health is widely accepted, and whether you look at the effects from a psychological, physiological, or spiritual lens, the results are evident. It is important to remember when working with clients through a trauma lens is that both trauma experiences, as well as responses, are highly individual, requiring clinicians to view this work with nuance.
Trauma produces more than the widely expected symptoms of post-traumatic stress disorder (PTSD). It can create layers of dysfunction that shape and color the way a person interacts with the world. Some impacts of trauma include:
- Mistrust and paranoia
- High anxiety, leading to social anxiety, agoraphobia, and other phobias
- Unsuccessful, unhappy, and abusive relationships
- Educational and occupational limitations
- Mood disorders, like major depression and bipolar disorders
- Problems with income, transportation, and housing
To help better understand the complexity and individuality of these responses, we can look to experts in the field of trauma informed therapy techniques:
Two people that experienced childhood sexual abuse could present in completely different ways. One could react in an expected way by being leery of adults, appearing cold and distant to others, and struggling to enjoy relationships with anyone. The other could have what is perceived to be a counterintuitive response by becoming very sexually motivated and socially extroverted. This response can feel jarring but is actually quite common. Interestingly, this phenomenon has been widely studied. Dr. Bruce Perry noted these differences in the children he worked with in his book The Boy Who Was Raised As A Dog.
These differences could start immediately, or they could take years to fully develop and only begin to emerge when brought forth either through a developmental or situational trigger, or other major life event. Therapists working with clients can help themselves while helping their clients by being acutely aware of trauma and its impact. Without acknowledgement of the barrier, clients may quickly display a plateau in treatment without meeting their goals.
Evidence-Based Trauma Therapy Techniques
When addressing trauma in therapy, it’s essential to use trauma informed therapy techniques that are not only compassionate and client-centered but also grounded in research and proven effectiveness. Trauma informed therapy encompasses a variety of evidence-based techniques that have been developed and refined to help individuals process and heal from the complex effects of trauma.
These approaches are designed to address the multifaceted nature of trauma, offering tailored strategies that can support clients in reclaiming their lives and fostering resilience. Each of the following trauma therapy techniques aligns with trauma-informed principles while addressing different aspects of recovery.
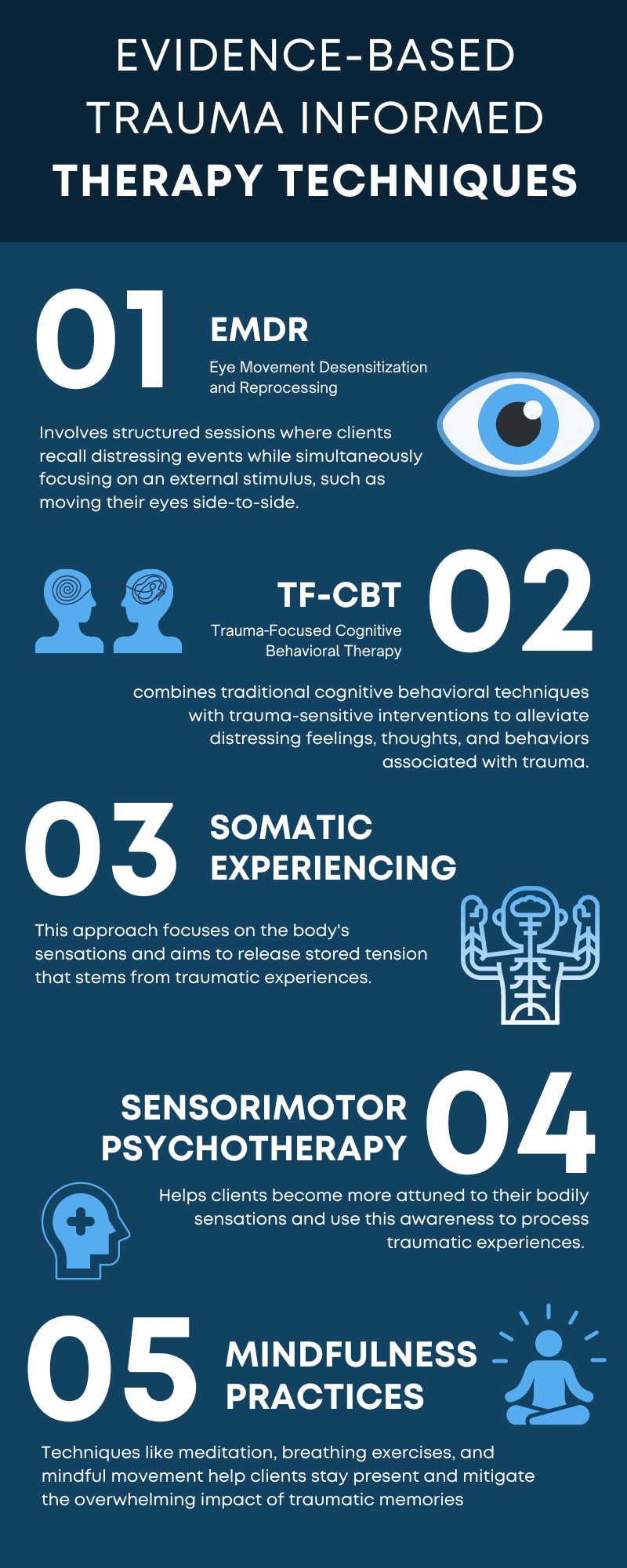
1. Eye Movement Desensitization and Reprocessing (EMDR)
Uses bilateral stimulation (eye movements, tapping) to help clients reprocess distressing memories.
-
Best for: PTSD, single-incident trauma
-
Key benefit: Rapid symptom reduction with minimal verbal disclosure
2. Trauma-Focused Cognitive Behavioral Therapy (TF-CBT)
Integrates psychoeducation, relaxation, and exposure for trauma processing.
-
Best for: Children, adolescents, families
-
Key benefit: Combines structure with emotional regulation training
3. Somatic Experiencing
Focuses on bodily sensations to release trauma stored in the nervous system.
-
Best for: Clients with hyperarousal or dissociation
-
Key benefit: Reduces physiological reactivity and improves regulation
4. Sensorimotor Psychotherapy
Integrates talk therapy with body awareness to process trauma held in the nervous system. This approach helps clients recognize and release automatic physical responses linked to past experiences.
-
Best for: Clients with chronic tension, dissociation, or body-based trauma responses
-
Key benefit: Promotes integration of emotional and physical awareness for deeper healing
5. Mindfulness and Grounding
Incorporates present-moment awareness and sensory focus.
-
Best for: Clients with flashbacks or intrusive thoughts
-
Key benefit: Reduces anxiety and anchors clients in safety
Utilizing these evidence-based trauma informed care interventions can enhance the therapeutic relationship and support clients in their recovery journey. Each approach offers unique benefits, and often, integrating multiple methods yields the best outcomes. A trauma informed therapist may integrate multiple approaches to best meet the needs of each client, considering the specific nature and effects of their trauma.
| Intervention | Focus Area | Ideal Client | Therapist Role | Example Technique |
|---|---|---|---|---|
| EMDR | Memory reprocessing | PTSD | Facilitator | Bilateral eye movement |
| TF-CBT | Cognitive reframing | Youth | Instructor | Trauma narrative writing |
| Somatic Experiencing | Body awareness | Dissociative clients | Co-regulator | Pendulation exercises |
| Sensorimotor Psychotherapy | Mind-body integration | Clients with chronic tension or dissociation | Guide and observer | Tracking posture, movement, and impulses |
| Mindfulness | Present awareness | Anxiety, stress | Coach | 5-4-3-2-1 grounding |
Integrating Trauma Informed Therapy Techniques into Clinical Settings
Creating a trauma informed clinical environment involves more than just individual therapy sessions. It requires an organizational culture shift and consistent practices to support both clients and staff. Bringing trauma informed care interventions into the clinical setting can enhance your practice by creating a space that invites trust, autonomy, and transparency for every client. Though it may seem abstract at first, focusing on a few ways to represent the guidelines will get you heading in the right direction.
Some of the best ways to bring trauma informed care interventions into psychotherapy include:
- Being aware of the possibility of every client you interact with having a history of trauma, and navigating conversations and treatment modalities with that awareness.
- Providing insight to clients throughout assessment and treatment, normalizing their own personal responses to traumatic experiences.
- Being transparent about your scope of practice in trauma work. It’s crucial to communicate your level of expertise and training in trauma treatment to your client, and to recognize when certain trauma experiences or responses are beyond your capability. Referring clients to other professionals when necessary is essential to providing ethical and effective trauma care.
- Compiling and offering a list of available in-person and online trauma-focused support groups in the community to support your client in maintaining or building new peer support options.
- Encouraging the client to be engaged and involved in all decisions throughout treatment. Be sure to make recommendations and offer insights into the risks and rewards of each intervention. For example, complete direct trauma work is often distressing in the moment but incredibly beneficial in time.
- As treatment continues over time, placing more of the decision-making power on the client. This act serves to reinforce their autonomy and increases levels of trust and power.
- Reminding the client that you are there to support and provide guidance, but they are the expert on their own experience. Here, you will remain accepting of their experience and practice humility as needed.
Case Vignette: Applying Trauma Informed Techniques in Session
Client: “Maria,” a 35-year-old survivor of childhood abuse, experiences panic when discussing the past.
Therapist response: Instead of pushing for disclosure, the clinician applies therapeutic techniques for trauma grounded in choice and pacing.
-
Begins session with grounding: “Let’s notice your feet on the floor.”
-
As emotions rise, uses somatic tracking: “Where do you feel that tension?”
-
Ends with empowerment: “You controlled how deep we went today—well done.”
This approach models trauma informed interventions that prioritize safety, collaboration, and emotional regulation.
Addressing Secondary Trauma and Burnout in Mental Health Professionals
Secondary trauma is the emotional and behavioral response to learning about or witnessing a traumatic event experienced by someone else. It can also be referred to as secondary traumatic stress, vicarious trauma, or secondary stress disorder. Secondary trauma can have negative effects on a person's life, including: job performance, professional satisfaction, intent to leave a job, relationships, and personal happiness.
Clinicians who work routinely with trauma are at risk of developing secondary, or vicarious trauma, and burnout. This is a natural result of consistent exposure to the pain and trauma that clients bring to each session, however it can and should be addressed before, during, and after the impact is felt. Addressing these issues is essential for maintaining staff well-being and effective client care.
The following measures should be put in place for all clinicians who experience exposure to traumatic stories.
- Selfcare and Boundaries: While it may feel unreasonable, it is essential for clinicians to practice selfcare both in their personal lives, as well as through setting boundaries around caseload, work hours, and client lists. As we enter this field, it can feel like we need to jump in with both feet due to the immense need we see in the communities we serve. However, striving for a balanced caseload and firm boundaries around hours can stave off secondary trauma and burnout.
- Clinical Supervision: No one is an expert in trauma informed care on day one. In fact, to be successful and ethical in trauma informed therapy, a clinician must always be learning new perspectives, approaches, studies, etc. Therapists in the trauma field need to seek out high-quality education, training opportunities, and clinical supervision to ensure they maintain high standards of care for their clients. Having weekly clinical supervisions with someone competent in trauma informed therapy and frequent check-ins with co-workers or colleagues can drastically improve your skills and is essential to ensuring checks and balances in the therapeutic process.
- Continuous Clinical Training: Continuing to improve your clinical knowledge of trauma work can mitigate the risk of burnout and secondary trauma by routinely building clinical capacity and skills. There are countless training opportunities for people interested in growing their trauma informed care knowledge. Eye-movement desensitization and reprocessing (EMDR), trauma-focused cognitive behavioral therapy (TF-CBT), and other specific treatment interventions can add to your repertoire of available therapy tools.
Ethical Considerations in Trauma Informed Therapy
Ethical issues play a significant role in trauma therapy. Upholding confidentiality, ensuring informed consent, and maintaining professional boundaries are vital for ethical conduct.
- Confidentiality is crucial in trauma-informed practices. Clients need to trust that their sensitive information will be kept private. Any breaches of confidentiality can significantly damage the therapeutic relationship and exacerbate trauma symptoms.
- Informed consent must be comprehensive. Clients should have clear explanations of the trauma-informed care interventions, potential risks, benefits, and alternatives. This transparency fosters trust and empowers clients to make informed decisions about their treatment.
- Maintaining professional boundaries ensures ethical conduct in trauma therapy. Boundaries help create a safe and predictable environment, which is essential for trauma survivors who often experience boundary violations. Clear professional lines prevent the risk of re-traumatization and maintain the integrity of the therapeutic relationship.
- Cultural sensitivity and humility are also crucial. Trauma affects individuals differently, shaped by cultural, social, and personal contexts. Therapists must approach each client with an open mind, respect diverse backgrounds, and acknowledge their own potential biases.
- Finally, ethical decision-making processes need to prioritize client safety and autonomy. When faced with ethical dilemmas, the well-being and rights of the client should be at the forefront of any decision-making. This involves continuous ethical education and reflective practice to navigate the complexities of trauma therapy responsibly.
Addressing these ethical considerations ensures that trauma informed therapy upholds the highest standards of care, protecting and empowering clients throughout their healing journey.
Trauma therapy is not an add-on service clinicians can learn through trial and error. It is a specialty field that needs to be studied and well understood before taking on a single client for trauma work. Even after this understanding has been established, it is essential for therapists to never attempt to work with trauma clients in a vacuum. Supervision and continuing education will ensure you know what you don’t know, alleviating ethical violations and irreparable damage to individuals seeking your care.
By understanding the 6 principles of trauma informed care — safety, trust, support, collaboration, empowerment, and humility — therapists can improve their skills, and support clients in improving their symptoms.
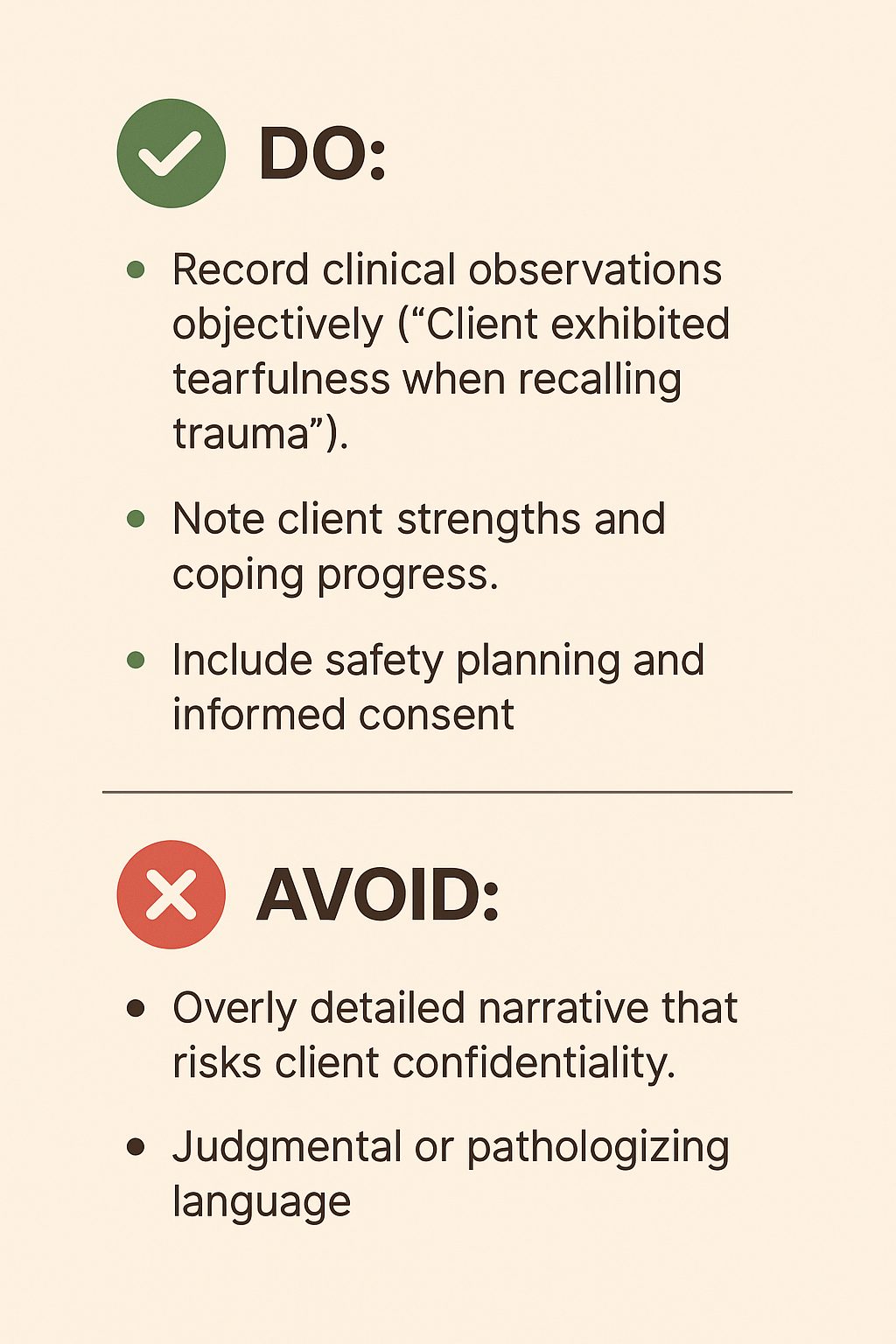
Documentation Best Practices for Trauma Therapy
Clinicians practicing trauma-informed care should document with clarity and care.
ICANotes simplifies trauma-informed documentation by offering structured templates and built-in prompts that reinforce ethical standards and clinical accuracy.
ICANotes gives behavioral health clinicians the tools to practice trauma-informed care with confidence.
✅ Menu-driven note templates for trauma therapy and crisis interventions
✅ Evidence-based rating scales for PTSD and anxiety
✅ AI Scribe to capture session details accurately without breaking rapport
✅ Built-in compliance features to protect client confidentiality
Start your free 30-day trial of ICANotes, no credit card required!
FAQs: Trauma-Informed Therapy Techniques and Interventions
Conclusion: Building a Trauma Informed Practice
Implementing trauma informed therapy techniques means moving beyond symptom management to true healing. By applying trauma informed interventions consistently, clinicians can help clients reclaim safety, self-trust, and empowerment.
Keep your skills sharp — download our Trauma Informed Care Cheat Sheet for a one-page refresher you can reference in session. Pair it with ICANotes, the behavioral health EHR that helps you document trauma-informed sessions faster and more accurately — without breaking rapport.
Related Posts

Kaylee Kron
LMSW
About the Author
Kaylee Kron, LMSW, GC-C, is a certified grief counselor with over a decade of experience. She has worked extensively in nonprofit hospice care, helping individuals navigate their grief journeys. As an author, speaker, and advocate, Kaylee brings a wealth of knowledge and compassion to her work, creating spaces for acknowledgment and healing.