Blog > Treatment Strategies > Six-Step Crisis Intervention: Clinical Steps for Counselors & Therapists
When a client presents in crisis — such as acute emotional distress or suicidal ideation — clinicians must respond quickly, ethically, and with clear clinical judgment.
The Six-Step Crisis Intervention process provides a structured, evidence-informed approach to assessing risk, stabilizing the client, and determining immediate next steps when safety is a concern. Designed for use in real-time clinical settings, this framework supports effective decision-making during mental health emergencies.
This guide walks counselors, therapists, social workers, and psychiatric providers through each step of the crisis intervention process, with practical guidance on assessment, response, and documentation to support ethical, defensible care.

Last Updated: February 9, 2026

What You'll Learn
-
The six-step crisis intervention process and how clinicians apply each step during mental health emergencies, including assessment, stabilization, and determination of appropriate next steps when safety is a concern
-
How to assess risk and safety concerns, including suicidal ideation, acute emotional distress, and other indicators that may require heightened monitoring, coordination, or escalation of care
-
What to focus on clinically at each stage of the crisis intervention process to stabilize the client, reduce immediate risk, and support clear, time-sensitive clinical decision-making
-
How crisis intervention differs from ongoing therapy, including when short-term stabilization is appropriate versus when referral, higher levels of care, or emergency services may be warranted
-
Key ethical and documentation considerations that support defensible, audit-ready crisis care, including risk assessment rationale, safety decisions, and clinical judgment during high-risk encounters
What Is Crisis Intervention?
Crisis intervention is a focused, time-sensitive approach used to help individuals regain stability after experiencing a psychological or emotional crisis. The goal is to reduce immediate distress, ensure safety, and connect the person with resources that support recovery. It is most often used in situations involving trauma, suicidal ideation, sudden loss, substance use, or acute mental health episodes.
This approach is grounded in crisis intervention theory, which explains how overwhelming events can disrupt a person’s ability to cope and function. When normal coping skills fail, timely intervention helps prevent long-term harm and supports a return to pre-crisis functioning.
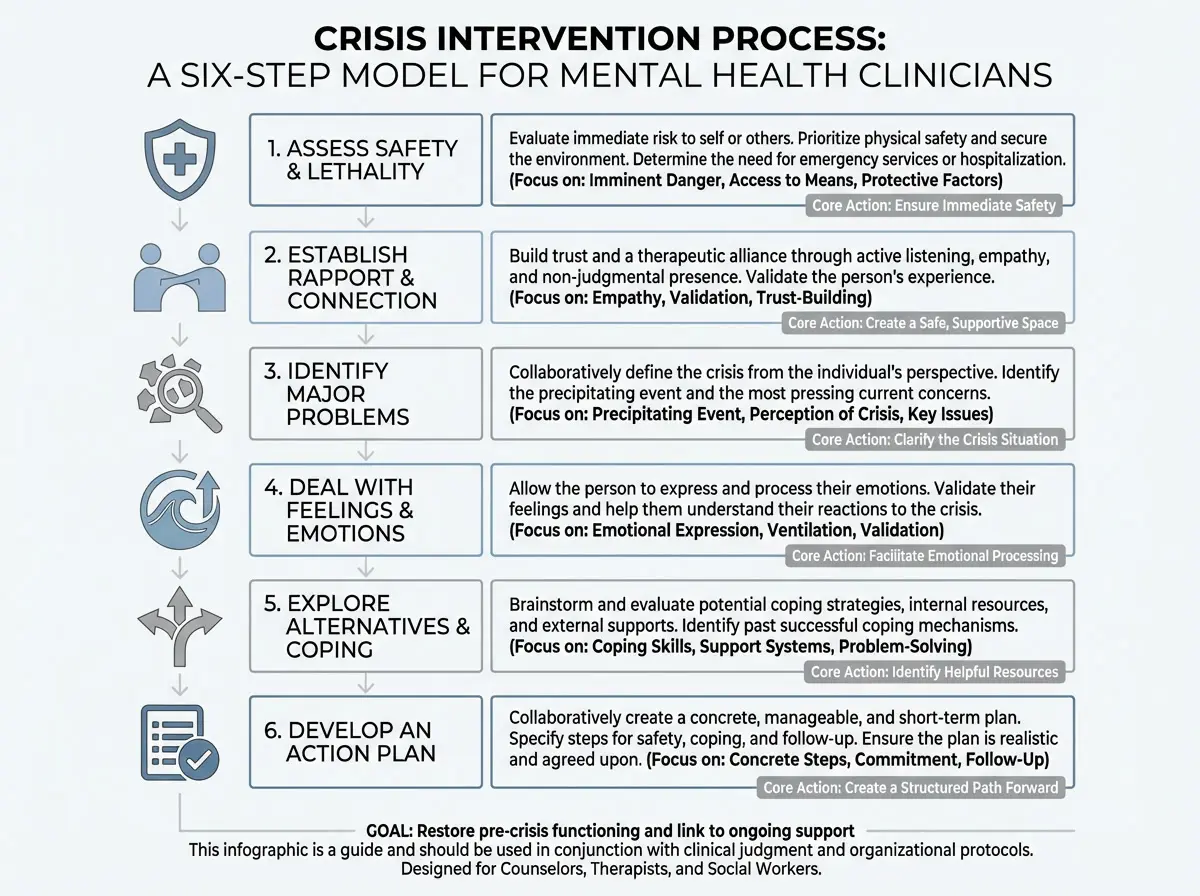
The six-step crisis intervention process provides clinicians with a structured, time-limited framework for responding to mental health emergencies. Each step builds on the previous one, guiding clinical decision-making from initial safety assessment through stabilization and actionable next steps.
Step 1: Assess Safety and Immediate Risk
The first priority in any crisis intervention is ensuring the individual’s immediate safety. Before addressing emotions, problem-solving, or coping strategies, clinicians must determine whether the client poses an imminent risk to themselves or others.
At this stage, clinicians conduct focused suicide and homicide risk assessments, paying close attention to indicators such as suicidal ideation, agitation, impulsivity, access to lethal means, and the client’s ability to maintain self-control. This assessment is ongoing and may evolve as new information emerges.
A critical component of safety assessment involves limiting access to potentially dangerous items. These may include obvious risks such as firearms or medications, as well as everyday objects that could be used for harm. The client’s environment, level of supervision, and treatment setting all influence how safety measures are implemented.
For example, an inpatient psychiatric setting typically offers more environmental controls and supervision than mobile crisis or community-based care. In less controlled settings, clinicians may need to coordinate additional supports or emergency services to reduce risk and ensure continuity of safety.
Only once the client is in a reasonably safe and stable environment can the clinician move forward with the remaining steps of crisis intervention.
Clinical Context
Updated Crisis Standards Clinicians Should Know
Crisis intervention occurs within a rapidly evolving care landscape. Clinicians should be aware of current standards that influence escalation, coordination, and documentation during mental health emergencies.
- 988 Suicide & Crisis Lifeline: The primary national access point for mental health crisis support. Clinicians should understand when referral to 988 is appropriate and how crisis services may coordinate with outpatient providers.
- Mobile Crisis Teams: Many regions deploy mobile crisis units to respond on-site, reduce emergency department utilization, and divert individuals from law enforcement involvement. Awareness of local availability supports timely escalation.
- Documentation & Liability Risk: Crisis encounters carry heightened clinical and legal risk. Documentation should clearly reflect risk assessment findings, clinical reasoning, and the rationale for safety decisions or referrals.
Step 2: Establish Rapport and a Therapeutic Connection
Once immediate safety concerns have been addressed, the next priority is establishing a calm, supportive connection with the client. In crisis situations, rapport is not about building a long-term therapeutic alliance — it is about helping the individual feel heard, understood, and emotionally contained enough to continue engaging.
During this step, clinicians focus on presence, empathy, and validation, rather than problem-solving or interpretation. A steady tone, simple language, and nonjudgmental responses help reduce emotional intensity and signal safety. The goal is to communicate: “You are not alone, and we can work through this together.”
Effective rapport-building during crisis intervention may include:
-
Using active listening skills such as brief reflections and summaries
-
Validating the client’s emotional experience without endorsing harmful behavior
- Using brief reflections and validation to confirm understanding without shifting into problem-solving
-
Avoiding “why” questions or premature advice
-
Allowing pauses and silence when appropriate
-
Maintaining a calm, grounded demeanor to support de-escalation
This step lays the foundation for the work that follows. When clients feel respected and emotionally supported, they are better able to clarify the nature of the crisis, express their emotions, and collaborate on next steps. Only after rapport has been established should the clinician move into identifying the primary crisis and its contributing factors.
Be ready when your clients need you most!
Download our Crisis Intervention Toolkit for Mental Health Clinicians—equip yourself with the essential tools to confidently navigate crisis situations in your practice. This toolkit is packed with evidence-based de-escalation techniques, guided questions for assessing suicide risk, and printable safety plans and coping tool worksheets.
Step 3: Identify the Primary Crisis and Precipitating Factors
Once rapport has been established, the clinician works collaboratively with the client to define the primary crisis. This step focuses on understanding what precipitated the current situation and what feels most urgent to the individual in this moment.
Rather than addressing every stressor at once, clinicians help clients narrow the focus to the specific events, thoughts, or circumstances that triggered the crisis. This may include recent losses, interpersonal conflicts, traumatic experiences, substance use, or sudden changes in functioning.
During this step, clinicians prioritize the client’s perspective, using open-ended questions and reflective clarification to ensure the problem is clearly understood. The goal is not to interpret or reframe prematurely, but to arrive at a shared understanding of the crisis that will guide the remaining steps.
Key considerations during this stage include:
-
Identifying the precipitating event or series of events
-
Clarifying how the client perceives the crisis and its impact
-
Distinguishing immediate concerns from longer-term issues
-
Noting existing supports or coping resources relevant to the situation
By clearly defining the primary crisis, clinicians can move forward with greater focus, helping the client process emotions, explore coping options, and develop an appropriate action plan.
Step 4: Support Emotional Expression and Processing
After the primary crisis has been identified, clinicians provide space for the client to express and process the emotions associated with the situation. Intense feelings such as fear, anger, shame, grief, or hopelessness are common during crises and can interfere with clear thinking if left unaddressed.
During this step, the clinician’s role is to facilitate emotional expression without rushing to fix the problem. This may involve reflective listening, naming emotions, and normalizing the client’s reactions to overwhelming circumstances. The goal is not to eliminate distress, but to help the client feel emotionally regulated enough to continue engaging in the intervention.
Effective emotional processing during crisis intervention may include:
-
Encouraging the client to describe what they are feeling in their own words
-
Reflecting and validating emotions without minimizing or escalating them
-
Normalizing emotional responses to crisis situations
-
Monitoring for emotional escalation that may require a return to safety-focused interventions
As emotional intensity decreases, clients are better able to consider options, access coping resources, and participate collaboratively in planning next steps.
Step 5: Explore Coping Strategies and Available Supports
Once emotional intensity has decreased, clinicians work collaboratively with the client to identify coping strategies and sources of support that can help manage the immediate impact of the crisis. This step focuses on practical, short-term options rather than long-term treatment goals.
Clinicians begin by exploring the client’s existing coping skills, noting which strategies have been helpful in the past and which may be realistic to use in the current situation. When internal coping resources are limited, greater emphasis may be placed on external supports, such as trusted individuals, community resources, or crisis services.
During this step, clinicians help clients:
-
Identify coping strategies that can reduce distress in the short term
-
Consider situational supports, including friends, family, or professional resources
-
Evaluate which options feel accessible and acceptable right now
-
Avoid overwhelming the client with too many choices
While gentle reframing may be used to challenge catastrophic thinking, the primary goal is not to promote positivity, but to expand the client’s sense of available options and increase their ability to cope safely until the crisis resolves.
This step prepares the groundwork for developing a clear, actionable crisis plan in the final stage of intervention.
As coping strategies and support options become clearer, the focus shifts to translating these insights into a concrete plan that helps the client maintain safety and navigate the period immediately following the crisis.
Step 6: Develop a Clear and Actionable Crisis Plan
In the final step of crisis intervention, the clinician and client collaborate to develop a clear, realistic plan that outlines what will happen next. This plan translates identified coping strategies and supports into specific, actionable steps the client can follow after the intervention.
Effective crisis plans are concrete and achievable, taking into account the client’s current emotional state, resources, and capacity. The focus is on short-term actions that promote safety, stability, and continuity of care, rather than long-term treatment goals.
In many cases, this process closely aligns with the development of a structured mental health safety plan, which helps translate coping strategies and support resources into clear, written steps the client can follow after the intervention. A well-designed safety plan supports client understanding, reinforces collaboration, and provides concrete guidance if distress escalates.
A crisis plan may include:
-
Specific coping strategies the client agrees to use
-
Contact information for supportive individuals or services
-
Referrals to appropriate clinical, medical, or community resources
-
Clear guidance on when and how to seek additional help if distress escalates
Throughout this process, clinicians emphasize collaboration and client choice, reinforcing the individual’s sense of control and agency. When clients leave a crisis intervention with a plan they understand and feel capable of following, they are better positioned to maintain safety and continue recovery.
For clinicians focused on audit-ready, defensible documentation during high-risk encounters, see our guide on the golden thread documentation in mental health. For deeper legal context on liability considerations when suicidal ideation or imminent risk is present, see Legal Liability Issues in Suicide Care.
Clinical Decision Point
When to Escalate the Level of Care
Crisis intervention may exceed the scope of outpatient care when immediate safety cannot be reasonably ensured. Clinicians should consider escalation when clinical judgment indicates that additional support or containment is necessary.
- Active suicidal ideation with intent, plan, or access to means
- Inability to establish or maintain immediate client safety
- Severe impairment due to psychosis, intoxication, or cognitive disorganization
- Absence of protective factors or refusal of recommended safety measures
- Clinical judgment that outpatient intervention alone is insufficient
Escalation may include coordination with mobile crisis teams, referral for emergency evaluation, higher levels of care, or connection to crisis resources such as the 988 Suicide & Crisis Lifeline, depending on local protocols and ethical considerations.
Clinical Examples of the Six-Step Crisis Intervention Process
The six-step crisis intervention process is designed to be flexible and responsive to a wide range of clinical situations. The examples below illustrate how the steps may be applied in real-world settings, while emphasizing that clinical judgment and situational context always guide decision-making.
Clinical Example
Example 1: Client Experiencing Suicidal Ideation After a Relationship Loss
A client presents with acute emotional distress following the sudden end of a long-term relationship and reports passive suicidal thoughts.
Step 1: Assess Safety and Immediate Risk
The clinician conducts a suicide risk assessment, evaluates access to means, and determines the level of supervision needed to ensure safety.
Step 2: Establish Rapport
Through calm presence and validation, the clinician helps the client feel heard and emotionally supported without rushing into problem-solving.
Step 3: Identify the Primary Crisis
The focus is narrowed to the recent relationship loss and the client’s fear of being alone, rather than longstanding relationship patterns.
Step 4: Support Emotional Processing
The client is given space to express grief, shame, and hopelessness associated with the loss.
Step 5: Explore Coping and Supports
Together, the clinician and client identify immediate coping strategies and supportive contacts who can help reduce isolation.
Step 6: Develop an Action Plan
A short-term plan is created that includes specific coping actions, scheduled follow-up, and clear guidance on when to seek additional help if distress escalates.
Note: This example is for educational purposes and does not replace clinical judgment or local emergency protocols.
Clinical Example
Example 2: Client in Acute Distress Related to Substance Use
A client presents during a crisis triggered by a recent relapse and fear of losing housing and employment.
Step 1: Assess Safety and Immediate Risk
Immediate safety is assessed, including current substance use, level of intoxication, and risk of harm to self or others.
Step 2: Establish Rapport
The clinician maintains a calm, nonjudgmental stance to reduce shame and support continued engagement.
Step 3: Identify the Primary Crisis
The precipitating factors are clarified as the recent relapse combined with immediate concerns about housing and job stability.
Step 4: Support Emotional Processing
The clinician supports expression of fear, frustration, and self-blame while monitoring for emotional escalation.
Step 5: Explore Coping Strategies and Supports
Available coping strategies and external supports are explored, including substance use resources, trusted individuals, and community services.
Step 6: Develop an Action Plan
A concrete plan is developed outlining next steps, referrals, follow-up arrangements, and guidance for seeking additional help if risk increases.
Note: This example is for educational purposes and does not replace clinical judgment, medical advice, or emergency protocols.
Using Clinical Judgment
These examples demonstrate how the six-step process provides structure without rigidity. Clinicians may move back and forth between steps as needed, particularly if safety concerns re-emerge. The model is intended to support ethical, organized responses to crisis while allowing flexibility based on the client’s needs, setting, and level of risk.
Core Skills That Support Effective Crisis Intervention
While the six-step crisis intervention process provides structure, effective outcomes depend on how clinicians apply the model in real-world situations. Crisis work requires clinical judgment, flexibility, and the ability to adapt interventions to the individual, the setting, and the level of risk involved.
The following core skills support safe, ethical, and effective crisis intervention across settings:
Accurate and Ongoing Assessment
Assessment informs every decision in crisis intervention, from evaluating risk to determining appropriate next steps. Because crises evolve rapidly, clinicians must continually reassess safety, emotional intensity, and available supports. Using structured, evidence-informed assessment tools helps reduce assumptions and supports sound clinical decision-making.
Collaborative Empowerment
Crises often leave individuals feeling overwhelmed and powerless. Effective intervention restores a sense of control by involving clients in decision-making whenever possible. Collaboration does not eliminate the need for firm clinical guidance, but it ensures the client’s voice, strengths, and preferences remain central to the process.
Action-Oriented Clinical Focus
Crisis intervention is time-limited and goal-directed. Clinicians prioritize practical actions that reduce immediate risk and promote stabilization. Each step of the process should move the client toward greater safety through concrete, achievable actions rather than abstract insight or long-term change goals.
Present-Moment Orientation
Crisis work focuses on what will help the client cope now. Interventions emphasize immediate relief, stabilization, and access to supports rather than techniques that require extended practice or long-term treatment engagement. This focus helps prevent overwhelm and supports follow-through.
Whole-Person Clinical Perspective
Effective crisis intervention considers emotional, cognitive, behavioral, social, and environmental factors. Viewing the client within the broader context of their life — including relationships, resources, and stressors — helps clinicians address not only immediate safety but also factors that influence recovery and continuity of care.
Benefits of the Six-Step Crisis Intervention Model
Crisis intervention plays a critical role in stabilizing individuals during periods of acute distress. When applied effectively, structured crisis responses can reduce immediate risk, support emotional regulation, and improve short-term outcomes across clinical and emergency settings.
The six-step crisis intervention model offers several practical benefits for clinicians:
-
Provides a clear, structured framework for responding to high-stakes situations, reducing uncertainty during crisis encounters
-
Supports consistent safety-focused decision-making, particularly when assessing risk and determining next steps
-
Balances listening and action, ensuring clients feel heard while still moving toward stabilization
-
Promotes collaboration and client engagement, helping restore a sense of control during overwhelming situations
-
Improves clinical efficiency, allowing clinicians to respond effectively without drifting into long-term treatment planning
-
Adaptable across settings, including outpatient care, emergency departments, mobile crisis teams, and community-based services
By offering a systematic yet flexible approach, the six-step model helps clinicians respond to crises with confidence while maintaining ethical, client-centered care.
Other Crisis Intervention Models Clinicians May Encounter
Several crisis intervention frameworks are used across clinical, emergency, and community settings. While these models differ in structure and emphasis, they share a common goal: stabilizing individuals during acute distress. The table below highlights how commonly used crisis intervention models compare at a high level.
Comparison: Other Crisis Intervention Models Clinicians May Encounter
The models below are commonly used across clinical, emergency, and community settings. This table provides a high-level overview to help you recognize each framework’s emphasis and typical use — clinical judgment and local protocols always guide application.
| Model | Typical Setting | Core Focus | Stages / Steps | Best For |
|---|---|---|---|---|
| Roberts’ Seven-Stage Crisis Intervention Model | Behavioral health, community crisis, ED/urgent care | Safety, assessment, problem definition, coping, action planning | 7 stages | Clinicians who want a structured, stepwise framework for assessment + stabilization |
| ABC Model (Affective–Behavioral–Cognitive) | Brief clinical encounters, crisis lines, outpatient triage | Rapid triage: emotions (A), behaviors/safety (B), thoughts/meaning (C) | 3 domains | Fast structure when time is limited and clarity is needed quickly |
| SAFER-R Model | Emergency response, disasters, first responder and critical incident contexts | Stabilization, acknowledgment, facilitating understanding, encouraging coping, referral/follow-up | 6 steps (SAFER-R) | High-stress incident stabilization with an emphasis on rapid support + referral |
| Lerner & Shelton’s 10-Step ATSM Protocol | Tactical / operational environments; high-acuity behavioral emergencies | Threat/safety management, stabilization, communication, and coordinated handoff | 10 steps | Scenarios requiring clear safety roles, coordinated response, and structured escalation |
Clinical note: Frameworks vary by setting and training. Many clinicians integrate elements across models while following organizational protocols and using clinical judgment.
Clinical note: These models are not mutually exclusive. Many clinicians draw from multiple frameworks depending on setting, training, and level of risk. The six-step crisis intervention model remains widely used due to its balance of structure, flexibility, and applicability across care environments.
Clinical Documentation Support for Crisis Intervention
Applying the Six-Step Crisis Intervention Model depends on timely assessment, accurate documentation, and clear follow-through. In high-acuity situations, clinicians need tools that support rapid clinical decision-making without adding unnecessary administrative burden.
ICANotes is a cloud-based EHR designed specifically for behavioral health workflows. Clinicians can document crisis encounters efficiently, capture risk assessments, and track interventions across each stage of the crisis response. Structured templates, customizable assessments, and integrated progress notes help ensure critical details are recorded clearly and consistently.
For teams working across inpatient, outpatient, or mobile crisis settings, ICANotes supports continuity of care through integrated scheduling, ePrescribing, and billing tools. This allows clinicians to focus on stabilization and safety while maintaining complete, audit-ready records.
By reducing documentation friction, ICANotes helps clinicians stay present during crisis encounters while supporting accurate records, compliance, and follow-up care.
If you want to see how this workflow functions in practice, you can explore ICANotes with a free 30-day trial.
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
- Complete Notes in Minutes - Purpose-built for behavioral health charting
- Always Audit-Ready – Structured documentation that meets payer requirements
- Keep Your Schedule Full – Automated reminders reduce costly no-shows
- Engage Clients Seamlessly – Secure portal for forms, messages, and payments
- HIPAA-Compliant Telehealth built into your workflow
Complete Notes in Minutes – Purpose-built for behavioral health charting
Always Audit-Ready – Structured documentation that meets payer requirements
Keep Your Schedule Full – Automated reminders reduce costly no-shows
Engage Clients Seamlessly – Secure portal for forms, messages, and payments
HIPAA-Compliant Telehealth built into your workflow
Frequently Asked Questions: Six Step Crisis Intervention Model
Related Posts
About the Author
Dr. October Boyles is a behavioral health expert and clinical leader with extensive expertise in nursing, compliance, and healthcare operations. With a Doctor of Nursing Practice (DNP) and advanced degrees in nursing, she specializes in evidence-based practices, EHR optimization, and improving outcomes in behavioral health settings. Dr. Boyles is passionate about empowering clinicians with the tools and strategies needed to deliver high-quality, patient-centered care.









