Blog > Documentation > EMDR Therapy Note-Writing Tips
EMDR Progress Note-Writing Tips
Accurate and consistent documentation is critical for effective EMDR therapy. Whether you're tracking progress through each of the eight phases or preparing for audits and continuity of care, using a structured EMDR note template can streamline your workflow. A well-written EMDR progress note captures essential clinical details from each session, helping ensure that EMDR session notes reflect both therapeutic interventions and client response across treatment.

Last Updated: June 05, 2025


What You'll Learn
- How EMDR therapy works and differs from traditional talk therapy approaches
- The eight phases of EMDR treatment and what happens during each stage
- Essential documentation techniques and note-taking strategies for each therapy phase
- Key EMDR assessment tools like VOC and SUD scales used to measure patient progress
EMDR therapy helps clients process past trauma that may be affecting their present-day functioning. Unlike cognitive-behavioral therapy (CBT) or traditional talk therapy, EMDR is a highly structured, phased approach designed to target disturbing memories using bilateral stimulation such as guided eye movements.
Typically completed in 6 to 12 sessions, EMDR requires precise documentation to monitor client response and treatment progress. If you're a trained clinician offering this modality, having a consistent EMDR note template and using structured EMDR worksheets can improve both efficiency and outcomes. If you're exploring whether to incorporate EMDR into your practice, reviewing EMDR progress note examples and other clinical resources can help you assess its fit with your therapeutic approach.
What EMDR Therapy Is and How It Works
Created by psychologist Francine Shapiro, EMDR therapy dates back to the late 1980s. Dr. Shapiro developed EMDR to treat post-traumatic stress disorder (PTSD). One of the keys to EMDR therapy is the Adaptive Information Processing model, also developed by Dr. Shapiro.
The model operates under the framework that PTSD symptoms and the symptoms of similar disorders stem from a person's past experiences that the brain has not yet fully processed. The memories connected to the experiences are full of beliefs, emotions and physical sensations that occurred simultaneously to the triggering event. Recalling the experience unleashes the unpleasant emotions, thoughts and sensations, bringing on PTSD symptoms.
EMDR therapy is notably different from other treatment modalities. The therapist doesn't ask a client to reflect on or discuss the traumatic experience during EMDR. Instead, the client focuses on the memory and aims to change their brain's relationship with it. An EMDR therapist leads the client through eye movements whenever the client recalls the triggering experience. Once the EMDR therapy has successfully altered the memory in the brain, a client's symptoms should dissipate.
EMDR is an example of short-term therapy. Sessions typically take place once or twice a week. Clients often have between six and 12 sessions. Some clients get the full benefit of the therapy from fewer sessions. The American Psychological Association (APA) conditionally recommends EMDR therapy as a PTSD treatment.
EMDR therapy consists of eight phases:
- History Taking and Planning
- Preparation
- Assessment
- Treatment: Desensitization
- Treatment: Installation
- Treatment: Body Scan
- Treatment: Closure
- Re-evaluation
What to Include in EMDR Progress Notes for Each Phase
The session notes you write when working with a client depend on the phase of EMDR you're focusing on. Although there are eight phases, the typical length of EMDR therapy is anywhere from six to 12 sessions. That means you might spend one session on a client's history and two or more sessions on preparation. The last two phases, closure and re-evaluation, occur during every session.
While CBT and other types of therapy typically have 45-minute sessions, the average EMDR session is about 90 minutes.
EMDR Phase 1 - History Taking and Planning
A clinician doesn't immediately jump into performing EMDR therapy on a client. Instead, it's critical to get a complete history from them first. EMDR History Taking and Planning is the first phase. This phase can take between one and two sessions to complete.
As you gather the client's history, take notes on what they tell you. An EMDR history taking session usually takes a three-pronged approach. You'll ask the client about:
- Memories from the past
- Issues and disturbances in the present
- Future goals and actions
During the EMDR history taking sessions, you'll work with the client to determine which memory is the most distressing to them. You'll then focus on that memory or experience first.
It's important to remember that one feature that sets EMDR apart from other treatment models is that your client doesn't have to dwell on or go into detail about their most challenging memory. You can ask them questions about the issue and take notes on it, but you don't need to get a complete picture of exactly what happened for the treatment to be effective.
To start EMDR history taking, ask the client what problem they want to address. Once they respond, you can ask for more details, such as:
- When it happens
- Who's involved
- When did it first start
- What about it upsets the client
Also, part of the client's history is identifying disturbing events in their past. You can ask the client to describe these events and give you a general age or year when they occurred. In your progress notes, lay out the events on a timeline so you can easily visualize what happened when.
Once you have a general history, examine how past events affect the client's present. Some questions to ask include:
- When was the last time you experienced the issue?
- How did you feel when it happened? What did you experience in your body when it took place?
- What was the worst part of the situation (an image, smell, noise, emotion or sensation)?
- What negative beliefs do you have about that situation?
The history should also include the client's thoughts on the future. Two questions to ask and make a note of the answers to are:
- When do you see the situation happening again in the future?
- How do you want to respond if the situation were to occur again?
EMDR Phase 2 - Preparation
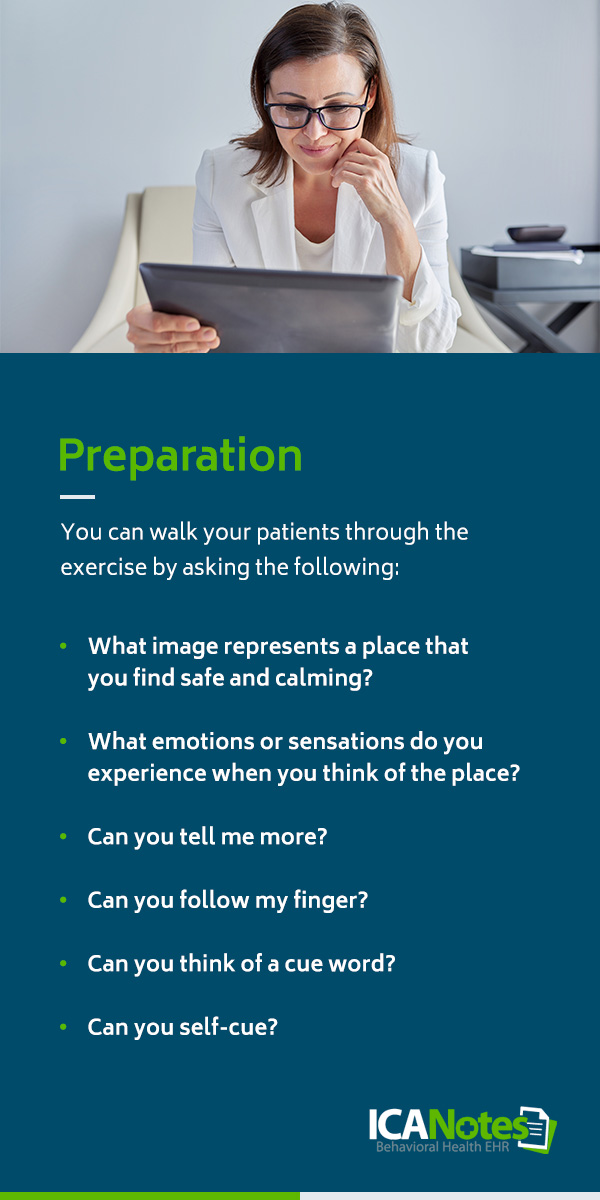
After gathering the client's history, it's essential to prepare them for EMDR treatment. During the preparation stage, you'll explain what will happen in EMDR.
Another way to look at the preparation phase is as the trust-building stage. Your clients must trust you, or their therapy won't be effective. One way to establish trust is to show them ways to calm themselves or relax when they start to feel uncomfortable or stressed during a session. You can use the Safe/Calm Place exercise to help them do this.
The Safe/Calm Place exercise allows clients to establish a calm place in their minds before processing their trauma or experience. You can walk your clients through the exercise by asking the following:
- What image represents a place that you find safe and calming? Ask the client to describe the place. Document their response.
- What emotions or sensations do you experience when you think of the place? Record any images, sounds or smells the client describes in their response.
- Can you tell me more? Ask the client to delve deeper into the emotions and sensations they feel.
- Can you follow my finger? Have the client think of their calm place and the sensations it creates, then ask them to follow your finger with their eyes. You might need to repeat this several times until the client feels better.
- Can you think of a cue word? Ask the client to summarize the image of their calm/safe place with a single word. Write this word down, as it is their cue word.
- Can you self-cue? Ask the client to think of their cue word and note how they feel.
Phase 3 - EMDR Assessment
After preparing the client by teaching them the eye movements and walking them through the Safe/Calm place exercise, you're ready to begin the EMDR Assessment phase. When assessing a client, you'll use two scales: the validity of cognition scale (VOC) and the subjective units of disturbance scale (SUD).
Before applying either scale, the client needs to identify a particularly distressing image from the experience you're targeting. Ask your client to describe a mental picture or image from the event. Note the image, then ask them to state a negative self-belief, or negative cognition, about the experience. Examples include, "I am bad," "I can't be loved," "I am weak."
Note the client's negative self-belief, then ask them to choose a positive cognition or belief. The goal here is to give the client a sense of control, so ideally, the positive cognition will be the reverse of the negative belief. For example, "I am good," "I am loveable," "I am strong."
Assess the client's stance on the positive belief by asking them to rate it on a VOC scale of one to seven. One is entirely false, and seven is entirely true. Next, ask them to rate how disturbing the negative emotion is on a scale of zero to 10. Zero is no disturbance, while 10 is the most disturbance.
The VOC and SUD scales let you assess how a client progresses once you begin the treatment phases. Document their responses from session to session. Ideally, the SUD will become lower, and the VOC will increase as they progress.
EMDR Treatment Planning
EMDR treatment spans four phases, which may occur in a single session. As you begin a treatment session with a client, it's important to document the following:
- The issue: What the client is focusing on in the session today.
- The positive cognition: Record the client's positive belief.
- The negative cognition: Record the client's negative belief.
- The treatment session: Record the EMDR session number, such as 1, 2 or 3.
- The prong you're addressing: Note whether you're addressing a past concern, present issue or future goal.
- Interventions used: Note any interventions used in the session, such as the Safe/Calm place exercise.
- Outcome of session: Record the session's outcome: Is the client finished with treatment, or should they return?
- Client status: How is the client at the end of the session? Do they seem unstable, stable or excellent?
- Other planned treatments: Are you using other therapies to treat the client in addition to EMDR?
The fourth phase of EMDR and the first part of treatment is desensitization. The goal of desensitization is to transform the memory from something distressing into something that no longer bothers the patient. To do this, you ask the patient to perform bilateral stimulation, such as eye movements, while thinking of the memory. Ask the patient to follow your finger with their eyes while concentrating on the negative cognition and the image. Ask them to pay attention to how they feel in their body while this is happening.
Phase 4 - Desensitization
The goal of desensitization is to bring the SUD down to zero if possible. For some clients, 1 or 2 on the SUD scale might be acceptable. Record the client's SUD as they move through the desensitization stage. Also, note the focus of the eye movements and the planned focus for the next session, if relevant.
Phase 5 - Installation
Phase five of EMDR is installation. While desensitization focuses on reducing SUD, installation aims to increase VOC.
Check in with the client about their positive cognition for the session. Ask them if it's still relevant. If not, ask them what positive belief is more appropriate. Document any changes they've made.
Next, ask them to rate the positive cognition on a scale from one to seven, completely false to entirely true. Tell them to keep that rating in their mind, then perform eye movements with them.
Ask them to rate the positive cognition again. Continue the installation process until the client reaches a seven.
If they are having trouble getting there, ask them to reflect on what's keeping them from fully believing the positive cognition. You might have to stop installation for the session if the client consistently responds with the same rating.
Phase 6 - Body Scan
Only move on to the sixth phase of EMDR, body scan, when the client has completed desensitization and installation. That means the client's SUD should be zero, and their VOC should be seven.
Have the client think of the image and their positive belief during the body scan. Then, ask them to note any remaining distress they feel. Note the distress, then use eye movements or other bilateral stimulation to help them process it.
Phase 7 - Closure
The seventh phase, closure, happens at the end of every session, whether the client made it through the sixth phase or not. If the EMDR therapy is incomplete, you might need to perform a containment exercise as part of closure to help stabilize the client and calm them.
If the session is complete and the client has reached SUD zero and VOC 7, focus on debriefing. Let them know that they might continue to process what went on in the session after they leave and encourage them to record any thoughts or feelings that come up. If you have more sessions remaining, make a plan for the next one and record it in the EMDR progress note for the session.
Phase 8 - EMDR Re-Evaluation
Re-evaluation, the eighth phase of EMDR, occurs at the beginning of the next session. During this phase, touch base with the client to see what has come up between the last session and this one. Make a plan for the new session based on the client's experience.
EMDR Progress Note Example
Below is a sample EMDR progress note that illustrates how to document a typical desensitization session. This example includes key elements such as the target memory, SUD and VoC ratings, client responses, and clinical impressions. Using a structured EMDR note template like this can help ensure consistency, support medical necessity, and improve treatment planning.
Date: 06/06/2025
Client Name: Jane Doe
Session #: 5
Phase: Phase 4 – Desensitization
Target Memory: Childhood car accident (age 10)
Negative Cognition: “I am not safe.”
Positive Cognition: “I can protect myself.”
VoC (Validity of Cognition): 3 (pre-processing)
SUD (Subjective Units of Distress): 8 (pre-processing)
Intervention Summary:
Client was guided through bilateral stimulation (eye movements) focused on the target memory. Processing included three full sets with brief assessments of cognition and affect in between. Client displayed signs of distress during initial sets (increased breathing rate, tearfulness) but remained within the therapeutic window of tolerance.
Client Response:
Client reported a shift in imagery mid-session, describing a sense of “watching the scene from above” rather than reliving it. Emotional intensity decreased steadily across sets. SUD reduced to 4 by end of session. VoC remained at 3 but client verbalized greater connection to the positive cognition.
Clinical Impressions:
Client is engaging well in the desensitization process and demonstrating affect tolerance and increasing cognitive restructuring. Continued focus on this target is recommended for next session to further reduce SUD and reinforce adaptive belief.
Plan:
Resume desensitization on same target in next session. Monitor for emerging related material. Prepare for transition to Phase 5 (Installation) once SUD reaches 0 or 1.
How ICANotes Can Help With EMDR Progress Notes
Accurate EMDR session notes are essential for tracking a client’s progress through each phase of treatment. ICANotes simplifies the process with intuitive, structured EMDR note templates that guide you in documenting key clinical details, including targets, triggers, SUD/VoC ratings, and client responses. These templates help ensure your EMDR progress notes are both comprehensive and compliant—without interrupting the flow of your sessions. Schedule a demo to see how ICANotes can support your EMDR documentation needs.
Schedule a Live Demo
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals—built to streamline documentation, improve compliance, and enhance patient care.
- Simplify clinical charting
- Stay organized with appointment scheduling
- Reduce no-shows with automated reminders
- Improve client engagement with a secure patient portal
- Provide flexible care with HIPAA-compliant telehealth
Simplify clinical charting
Stay organized with appointment scheduling
Reduce no-shows with automated reminders
Improve client engagement with a secure patient portal
Provide flexible care with HIPAA-compliant telehealth
Dr. October Boyles is a behavioral health expert and clinical leader with extensive expertise in nursing, compliance, and healthcare operations. With a Doctor of Nursing Practice (DNP) from Aspen University and advanced degrees in nursing, she specializes in evidence-based practices, EHR optimization, and improving outcomes in behavioral health settings. Dr. Boyles is passionate about empowering clinicians with the tools and strategies needed to deliver high-quality, patient-centered care.