Blog > Documentation > Counseling Notes Template and Documentation Guide: What to Include + Examples
What to Include in a Counseling Note (with Templates and Examples)
In behavioral health, clear and compliant counseling documentation is essential. Whether you're a therapist, counselor, or social worker, writing effective counseling notes helps track clinical progress, justify medical necessity, and improve continuity of care.

Last Updated: July 21, 2025


What You'll Learn
-
What a counseling note is (and what it’s not)
-
What to include in every counseling session note
-
Real-world sample counseling notes
-
How to use a counseling notes template to streamline documentation
What Is a Counseling Note?
A counseling note—also called a therapy progress note—is the official clinical documentation of a client session. It is part of the medical record and is used to:
-
Document symptoms, treatment goals, and interventions
-
Track client progress over time
-
Ensure compliance with insurance and legal requirements
-
Support coordination with other providers

Counseling notes are not psychotherapy notes
Psychotherapy notes (also known as process notes) are kept separate from the medical record and contain the therapist’s private reflections. Counseling notes (progress notes), by contrast, are formal, shareable records used for care, billing, and compliance.
What Should Be Included in Counseling Documentation?
A complete and effective counseling note typically includes:
-
Client name and clinician name
-
Date and time of the session (start/end)
-
Type of service (individual, group, family therapy)
-
Presenting problem or focus of the session
-
Client’s reported symptoms, mood, or behavior
-
Therapist observations (e.g., affect, speech, appearance)
-
Interventions provided (e.g., CBT techniques, grounding, motivational interviewing)
-
Client response to interventions
-
Clinical assessment or diagnosis-related updates
-
Plan (goals, homework, next steps)
-
Risk factors (e.g., suicidality, substance use)
-
Next appointment (if scheduled)
-
Clinician’s signature
Using a structured counseling notes template ensures consistency, saves time, and helps meet documentation standards across sessions.
Download Our Guide to Writing Better, Faster Clinical Notes
Streamline your progress notes, avoid documentation pitfalls, and stay compliant with practical templates, note formats (SOAP, DAP, BIRP), and time-saving tips to write high-quality, defensible notes faster.
Sample Counseling Notes (Examples in SOAP, DAP, and BIRP)
You can take notes in several ways during or after your counseling sessions. The format or method you use will depend on your personal preferences and your clinical setting. Let's take a look at three popular note formats and how each counseling note would look for a sample scenario.
Scenario Overview
Client presents with anxiety about social situations.
- “The patient was 15 minutes late and appeared disheveled and teary-eyed. She was upset about the effect her social anxiety had on interrupting her ability to be more independent.”
- “The patient expressed feelings of failure and guilt after she was unable to complete my assigned homework from last week, which included sitting in a coffee shop for 30 minutes and attempting to strike up a small conversation with a stranger.”
- “We discussed how we can further her treatment, and the patient seemed frustrated and irritated at her lack of progress. She stated, ‘I don’t think I’m ever going to fix this.’ I assured her we can adjust the treatment plan and start with more moderate exercises.”
- “We revisited medical interventions as a potential treatment adjustment, but she was uninterested in pharmaceutical options.”
- “The patient said she was having severe panic attacks related to anxiety-inducing situations, such as going grocery shopping or meeting up with friends in a crowded place. From her descriptions, I suspect she may potentially have agoraphobia in addition to her social anxiety.”
- “The patient revealed her desire to increase her sense of freedom by taking small steps toward these goals, including taking a trusted family member with her in these outings until she feels comfortable to go out on her own.”
- “We modified her treatment plan assignment to attempt a less extreme form of exposure therapy. The patient will spend no more than five minutes in a grocery store and attempt to purchase one item. I feel more confident about giving her lower intensity exercise and believe she will succeed.”
Counseling SOAP Note Example
Using the SOAP method, you will focus on structuring your notes by Subjective Data, Objective Data, Assessment, and Plan.
- Subjective data: Include the most pressing concerns from your patient and any important statements they make.
- Objective data: Note your patient’s body language, appearance and other factual, observable aspects about them. Do not include judgments or opinions.
- Assessment: Bring together your subjective and objective data and make a professional statement about what they mean. Include any goals, objectives and interventions addressed during the session or potential further investigation needed.
- Plan: Describe what will happen in your next session, the tasks or exercises you assign to your patient and whether they need a referral or revision of their treatment plan.
Here’s a simple example of how you can turn the detailed, informal notes from the scenario above into a SOAP note.
-
S (Subjective):
Client stated, “I feel like I’m never going to get better.” Missed homework due to panic attacks. Expressed fear of being judged in public spaces. -
O (Objective):
Client appeared tearful, fidgeted, and avoided eye contact. Arrived 10 minutes late. Speech slow but coherent. -
A (Assessment):
Increased social avoidance noted. Missed assignment suggests reduced motivation. Client verbalized hopelessness, but denied suicidal or self-harm ideation when assessed. Protective factors include strong family support and willingness to continue therapy. -
P (Plan):
Reframe exposure homework to reduce intensity and enhance success. Client will visit a quiet grocery store for 5 minutes accompanied by a trusted person. Therapist to reassess risk next session and consider safety plan review if hopelessness increases.
Counseling BIRP Note Example
The BIRP method is similar to the SOAP method, but you’ll focus more on behavior and interventions in this format.
- Behavior: Note the patient’s behavior, including statements they make during the appointment and factual observations you make.
- Interventions: Describe specific therapeutic interventions you used during the session, such as practicing mindfulness or identifying triggers.
- Response: List the client’s response and reaction to your intervention techniques and their general response to the overall treatment.
- Plan: Include future therapeutic techniques you’d suggest for following appointments and any follow-up work for the patient.
Here’s an example of how you can turn the informal notes from the scenario above into a BIRP note.
-
B (Behavior):
Client stated, “I feel like I’m going backward.” Tearful, slouched posture, limited verbal responses. Avoided eye contact and acknowledged skipping homework due to anxiety spikes. -
I (Intervention):
Therapist provided psychoeducation on anxiety avoidance cycles. Used motivational interviewing to explore ambivalence. Conducted suicide risk screening—client denied suicidal ideation, plan, or intent. -
R (Response):
Client appeared more engaged after risk screening. Expressed relief at discussing fears. Verbally committed to modified exposure activity. -
P (Plan):
Assign manageable exposure task (short store visit with support). Continue tracking anxiety and monitor suicide risk weekly. Re-evaluate in next session. Documented no current risk; safety plan discussed as preventative tool.
Counseling DAP Note Example
The DAP method is also similar to SOAP notes, except it combines your objective and subjective data into one category:
- Data: Combine your subjective and objective notes and any critical elements you observed during the session.
- Assessment: Assess the data and include your in-session intervention modalities and the patient’s response to them.
- Plan: Note future recommended therapeutic interventions or follow-up work for the patient.
Here’s an example of how you can turn the informal notes from the scenario above into a DAP note.
-
D (Data):
Client reported feeling “stuck” and fearful of going outside. Cried during session and stated, “What’s the point of trying?” No physical agitation noted. Denied thoughts of harming self or others when asked directly. -
A (Assessment):
Ongoing social anxiety with increased avoidance behaviors. Client appears emotionally overwhelmed but currently low risk for harm. Insight remains intact, and client engaged in problem-solving discussion. Safety was assessed and no red flags identified at this time. -
P (Plan):
Modify exposure task to smaller steps. Assign new homework involving 5-minute store visit with support person. Continue to monitor mood and suicidal ideation weekly. Schedule follow-up in 7 days.

Tips for Choosing the Right Note Format
-
Use SOAP if you need a clinical, highly structured format suitable for audits or multi-disciplinary care.
-
Use DAP if you prefer a concise, efficient format for solo practice or weekly therapy notes.
-
Use BIRP when documenting frequent sessions or interventions in community mental health, IOPs, or residential programs.
Counseling Notes Template
To streamline your documentation process, consider using a structured counseling notes template. Templates reduce time spent writing, improve compliance, and make it easier to track treatment over time.
A basic counseling notes template may include:
| Section | Example Content |
|---|---|
| Session Type | Individual Therapy – 60 minutes |
| Presenting Issue | Social anxiety; client reports difficulty initiating conversations |
| Subjective Report | Client stated, “I feel overwhelmed in public spaces.” |
| Observations | Tearful; anxious posture; poor eye contact |
| Interventions Used | Cognitive restructuring, goal setting, psychoeducation on avoidance cycles |
| Client Response | Open to trying new behavioral experiments; verbalized increased hope |
| Assessment | Symptoms consistent with social anxiety disorder; mild improvement noted |
| Plan | Assign brief exposure task; reassess in next session |
| Risk Assessment | Client denied suicidal ideation; low current risk; will monitor weekly |
| Next Appointment | Scheduled for next Thursday at 3 PM |
| Clinician Signature | Jane Doe, LCSW |
Why Structured Counseling Notes Matter
Using a standardized format for your counseling documentation helps you:
✅ Ensure accuracy and completeness
✅ Demonstrate medical necessity for insurance audits
✅ Maintain clinical focus across sessions
✅ Reduce documentation time with templates
✅ Protect your practice from legal risk
Final Thoughts: Make Counseling Notes Work for You
Your counseling notes don’t have to be lengthy to be effective. With the right format and a quality counseling notes template, you can document progress clearly, meet compliance standards, and stay focused on client care.
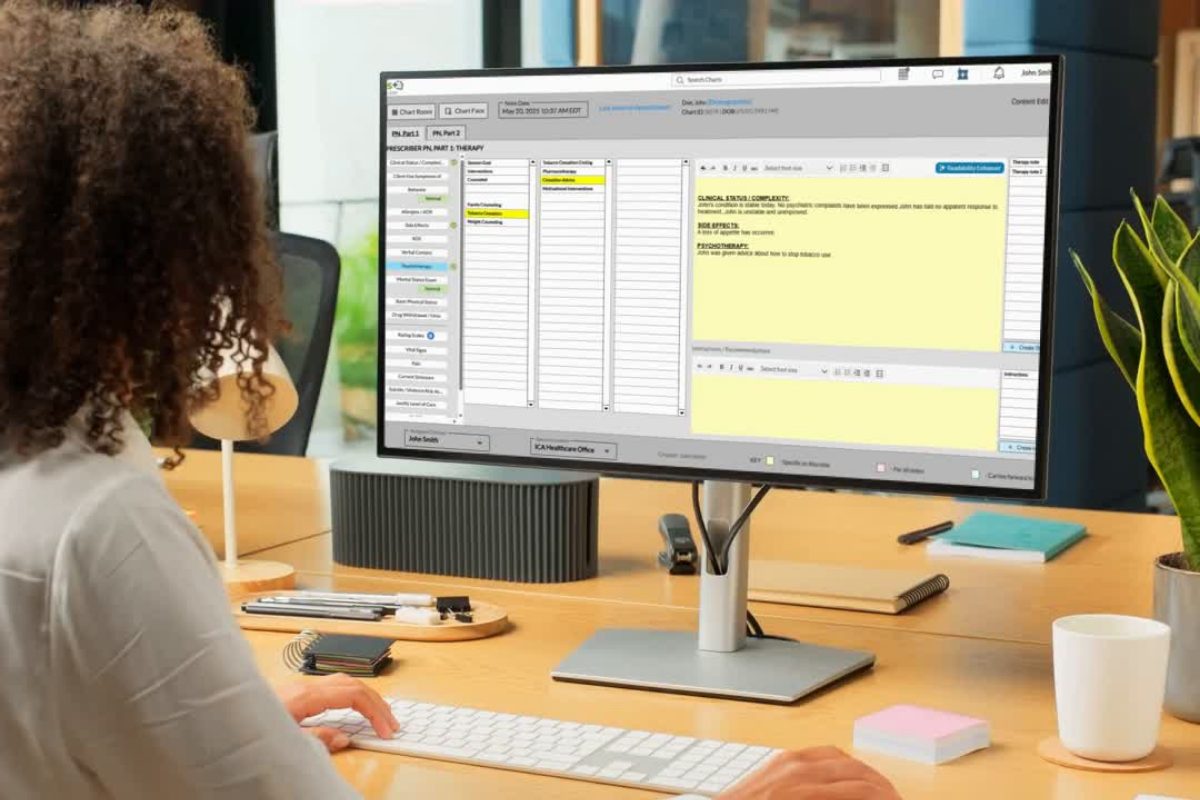
If you’re still writing your notes from scratch or struggling to keep up, consider using a behavioral health EHR like ICANotes. Our platform includes pre-configured counseling note templates and auto-generated narrative text to help you complete notes in minutes, without sacrificing quality.
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
- Complete Notes in Minutes - Purpose-built for behavioral health charting
- Always Audit-Ready – Structured documentation that meets payer requirements
- Keep Your Schedule Full – Automated reminders reduce costly no-shows
- Engage Clients Seamlessly – Secure portal for forms, messages, and payments
- HIPAA-Compliant Telehealth built into your workflow
Complete Notes in Minutes – Purpose-built for behavioral health charting
Always Audit-Ready – Structured documentation that meets payer requirements
Keep Your Schedule Full – Automated reminders reduce costly no-shows
Engage Clients Seamlessly – Secure portal for forms, messages, and payments
HIPAA-Compliant Telehealth built into your workflow
Frequently Asked Questions
Related Posts
Dr. October Boyles is a behavioral health expert and clinical leader with extensive expertise in nursing, compliance, and healthcare operations. With a Doctor of Nursing Practice (DNP) from Aspen University and advanced degrees in nursing, she specializes in evidence-based practices, EHR optimization, and improving outcomes in behavioral health settings. Dr. Boyles is passionate about empowering clinicians with the tools and strategies needed to deliver high-quality, patient-centered care.