Blog > Documentation > How to Write Psychotherapy Notes: What to Include & Skip
How to Create a Psychotherapy Note (Step-by-Step Guide)
Mental health professionals have many details to remember about many different clients. Some therapists might see over 20 clients a week, yet they need to know each person as if they didn't have a full schedule. Writing psychotherapy notes allows counselors to grasp their clients' conditions to provide optimal care.
This guide will help you learn how to write psychotherapy notes using modern tools like ICANotes. We’ll explain the difference between psychotherapy and progress notes, what to include and exclude in a psychotherapy note, and how HIPAA rules apply to psychotherapy notes.

Last Updated: August 22, 2025

What You'll Learn
-
The true definition of psychotherapy notes and how they differ from progress notes (private/optional vs. legal/required), including why they’re exempt from the Cures Act when kept separate.
-
Exactly what to include (reflections, hypotheses, therapist reactions) and what HIPAA says must be excluded (e.g., diagnosis, meds, session times, treatment plan) to keep them distinct from the medical record.
-
Practical safeguards and policies: separation from the chart, confidentiality, retention/disposal best practices, and APA record-keeping guidance.
Contents
- What’s New in 2025
- What Is a Psychotherapy Note?
- How Are Psychotherapy Notes Different From Progress Notes?
- How Do You Write a Psychotherapy Note?
- What Shouldn't Be Included in a Psychotherapy Note?
- Are Psychotherapy Notes Covered Under HIPAA?
- How Long Do I Keep Psychotherapy Notes?
- How Should I Dispose of Psychotherapy Notes?
- Essential Considerations for Writing Psychotherapy Notes
What's New in 2025?
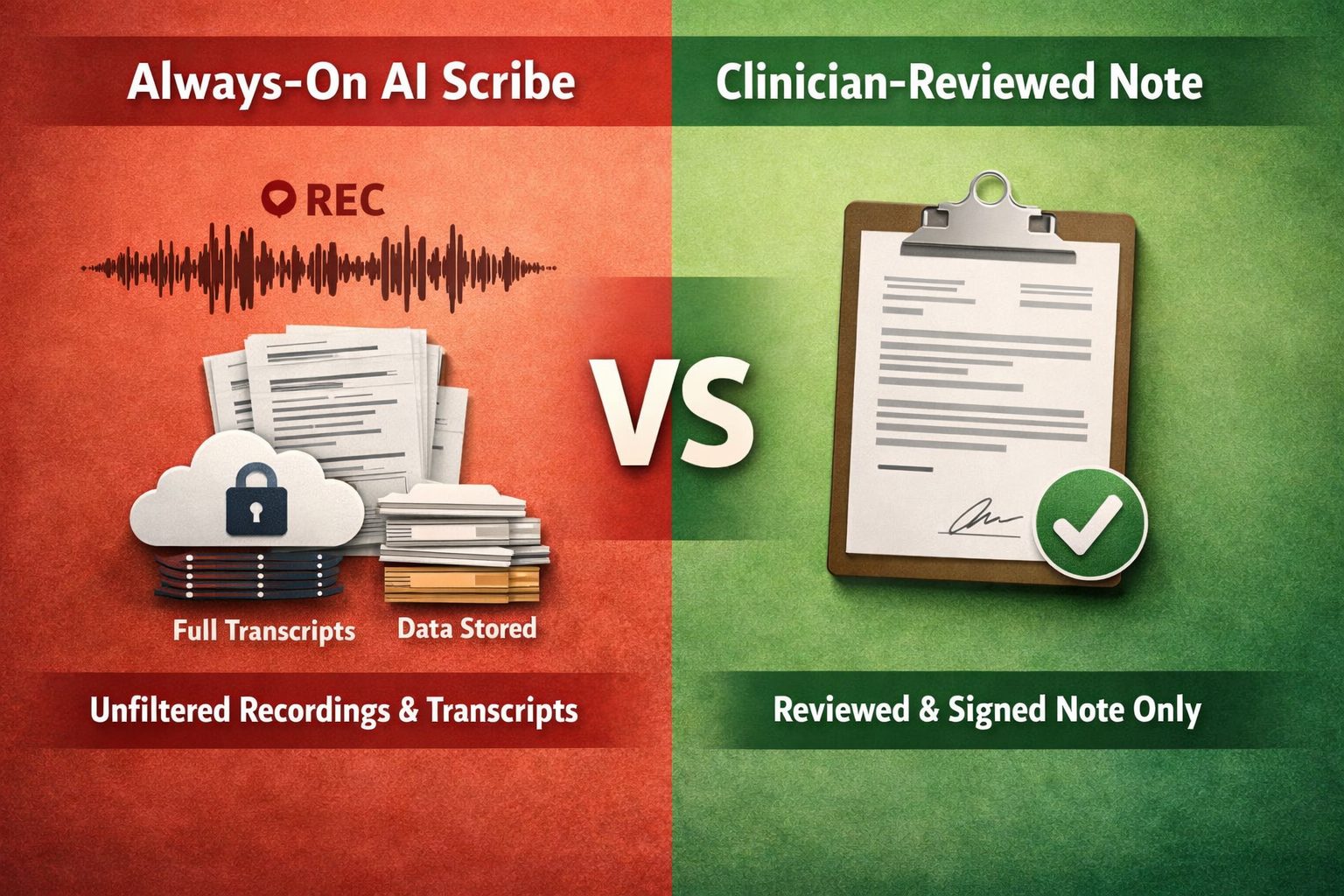
The way clinicians create psychotherapy notes and progress notes has evolved. In 2025, leading behavioral health platforms like ICANotes provide:
- AI-enhanced note-writing tools: ICANotes now offers an AI Scribe that generates editable drafts from live or recorded sessions.
- Built-in readability optimization: Notes can be cleaned, clarified, and standardized with a single click, improving privacy and accuracy.
- Group telehealth support: ICANotes telehealth now supports group sessions, virtual waiting rooms, and screen sharing — all launched directly from appointment calendars or patient charts — for seamless therapy continuity.
Advanced privacy safeguards: All AI features in ICANotes are fully HIPAA-compliant and do not share data with external models. ICANotes encrypts patient data, offers audit logs, and ensures HIPAA and ONC-ATCB certification. No session data is used for external AI training—your records stay private.
What Are Psychotherapy Notes?
Psychotherapy notes are a counselor's private notes written during or after a counseling session. Unlike other forms of clinical documentation, psychotherapy notes are optional. They may be used to help a therapist analyze a session's content, form an impression, or explore their thoughts and feelings about a client and their condition.
These notes can:
- Help therapists reflect on client dynamics.
- Capture ideas for future sessions.
- Record therapist reactions and hypotheses.
They’re typically stored separately from the EHR’s main chart and are never shared with clients or third parties without consent (except under court order).
If you decide to write psychotherapy notes, you may find them helpful in gaining a clearer understanding of your clients and the treatment they need. You can record the notes in any medium you prefer, such as a notepad or laptop, as long as you keep the notes separate from clients' medical records.
How Are Psychotherapy Notes Different from Progress Notes?
Progress notes are clinical documents used to track diagnosis, symptoms, and treatment. Psychotherapy notes are excluded from the client’s chart as long as they remain separate and distinct.
Psychotherapy notes are not meant to be shared with others, unlike progress notes. Progress notes are legal documents that belong in a client's medical records and can be read by clients and other clinicians involved in a patient's treatment. Progress notes are also required for ethical and legal purposes.
| Category | Psychotherapy Notes Private | Progress Notes Medical Record |
|---|---|---|
| Primary purpose | Therapist’s personal analysis of session content (reflections, hypotheses, countertransference). | Clinical, billing, and care-coordination documentation of the episode of care. |
| Where they live | Kept separate from the designated medical record. | Part of the designated medical record/Designated Record Set (DRS). |
| Patient right of access | Generally not subject to the HIPAA Right of Access when kept separate. | Subject to HIPAA Right of Access and information-blocking rules. |
| Typical inclusions |
|
|
| Required exclusions (for psych notes) | Must exclude: diagnosis, meds, session time, modalities, test results, plan, progress, etc. | These items belong here (objective, clinically necessary content). |
| Sharing/disclosure | Generally require patient authorization; limited TPO uses. | May be used/disclosed for TPO (treatment, payment, operations) per HIPAA. |
| Billing & utilization review | Not used for claims or routine utilization review. | Used to support claims, medical necessity, audits. |
| Legal status | Optional/private record maintained by the therapist. | Part of the official medical record; retention rules apply. |
| Examples | “Client’s story about father evokes protective schema; consider parts-work next session.” | “CBT cognitive restructuring; client identified 3 distortions; PHQ-9 ↓ from 17→12; next: exposure hierarchy.” |
| Best practice | Keep brief, reflective, and stored separately; limit access. | Document clearly, objectively, and sufficiently for continuity of care and reimbursement. |
Therapists keep progress notes to plan and document treatment and determine if therapy is helping a client improve. Counselors also keep progress notes to protect themselves legally, get reimbursed by insurance companies, and coordinate care with other healthcare providers.
Progress notes are brief and typically follow a standard format to communicate them easily to clients, clinicians, and insurance companies. For example, behavioral health professionals often use the subjective, objective, assessment, and plan (SOAP) format to write thorough and well-organized progress notes.
Unlike psychotherapy notes, progress notes must be easy to read so clinicians can quickly understand a client's medical history and current condition. Also, with the 21st Century Cures Act's information blocking rule, healthcare providers are required to give clients access to their medical records in the electronic health record (EHR) system, including their progress notes. Psychotherapy notes are exempt from the information-blocking rule as long as they are kept separate from clients' medical records.
How Do You Write a Psychotherapy Note?
Since psychotherapy notes are optional, there is no specific format you need to follow, nor do these notes need to be legible to others. For example, you can write notes in shorthand or create brainstorming diagrams if you wish. Regarding what you should write about, here's what you might include:
- Your observations about a client
- Your hypotheses or ideas
- Questions to ask your supervisor
- Topics you want to research
- Any thoughts or feelings you have about a therapy session and a client.
In 2025, many clinicians use ICANotes’ private psychotherapy note feature to compose these reflections in a secure, segregated space.
What Shouldn't Be Included in a Psychotherapy Note?
Even though psychotherapy notes are not legal documents like progress notes, there are still a few rules to consider. These rules establish your psychotherapy notes as your private notes and not medical records. According to the Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule, psychotherapy notes must exclude the following information to be considered personal documents and not part of a client's medical record:
- Medications
- Medication monitoring
- Session start and stop times
- Clinical test results
- Treatment methods and frequencies
- Diagnosis
- Treatment plan
- Symptoms
- Functional status
- Prognosis
- Progress.
Are Psychotherapy Notes Covered Under HIPAA?
Yes, psychotherapy notes are covered under HIPAA, and there are protections for both therapists and clients. First, therapists are not required to share their private notes with clients, insurance companies, other healthcare providers, or anyone else. However, if a client requests to see a counselor's psychotherapy notes, the counselor can choose to share the notes if they wish.
Regarding clients' rights, counselors cannot share their psychotherapy notes without first obtaining the client's consent, with a few exceptions. Therapists may not need a client's authorization if they receive a court order.
How Long Do I Keep Psychotherapy Notes?
Because psychotherapy notes are optional, no rule states you must keep them for a specific amount of time. With that said, you may want to get rid of notes that are no longer helpful to you to eliminate the risk of someone else reading them. However, older psychotherapy notes may help you treat a particular client at a later time, depending on their needs. It's up to you to decide whether they are worth keeping.
The American Psychological Association (APA) provides general record-keeping guidelines you can apply to your psychotherapy notes if you prefer. According to the APA's guidelines, psychologists might retain an adult client's complete records for seven years after the last session or until three years after a minor reaches adulthood.
How Should I Dispose of Psychotherapy Notes?
If you decide to dispose of your psychotherapy notes, you'll want to implement the same safeguards you'd use for any client record to keep the information confidential. For instance, if you write psychotherapy notes on paper, consider shredding the notes when you no longer need them before throwing them away. Regardless of the disposal method you choose, it's essential that your notes are unreadable and cannot be reconstructed before placing them in the trash.
If you store your psychotherapy notes electronically, ensure your system is secure before deleting files. HIPAA provides examples of proper disposal methods for both paper records and electronic media.
Essential Considerations for Writing Psychotherapy Notes
In general, you're free to include your ideas, opinions, feelings, and other information that's not appropriate for medical records in your personal notes. But there are still a few things you'll want to keep in mind:
- Someone might read your psychotherapy notes: You can include thoughts and feelings you would not put into a client's progress notes. Still, you'll want to be careful with incriminating information because someone might read your notes under specific circumstances. Your private notes can be subpoenaed if there's a concern about public safety. So it's best not to include anything in your notes you wouldn't want a judge to see.
- You should keep them separate: It's a good practice to keep psychotherapy notes separate from a client's medical records. If your psychotherapy notes are not distinguishable from a client's progress notes or general chart, they will be considered part of their medical record. They can then be disclosed to other healthcare providers or insurance companies without the client's authorization.
- You still need to maintain confidentiality: Even though psychotherapy notes are your private notes, you still need to keep them confidential without a client's consent. If you write in a notebook, make sure you do not leave it out in the open for others to read. If you use a computer to write and store psychotherapy notes, ensure the notes are password-protected.
Frequently Asked Questions about Psychotherapy Notes
Writing Psychotherapy Notes with ICANotes EHR
Using a HIPAA-compliant EHR system to write psychotherapy notes can help you maintain confidentiality effortlessly and efficiently. With ICANotes, you can write psychotherapy notes directly in your EHR and keep them separate and private. You can also rest assured that your psychotherapy notes are secure and HIPAA-compliant.
To try ICANotes behavioral health EHR and see how it works, request your free trial or contact us today for more information.
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
- Complete Notes in Minutes - Purpose-built for behavioral health charting
- Always Audit-Ready – Structured documentation that meets payer requirements
- Keep Your Schedule Full – Automated reminders reduce costly no-shows
- Engage Clients Seamlessly – Secure portal for forms, messages, and payments
- HIPAA-Compliant Telehealth built into your workflow
Complete Notes in Minutes – Purpose-built for behavioral health charting
Always Audit-Ready – Structured documentation that meets payer requirements
Keep Your Schedule Full – Automated reminders reduce costly no-shows
Engage Clients Seamlessly – Secure portal for forms, messages, and payments
HIPAA-Compliant Telehealth built into your workflow
Related Posts
Dr. October Boyles is a behavioral health expert and clinical leader with extensive expertise in nursing, compliance, and healthcare operations. With a Doctor of Nursing Practice (DNP) and advanced degrees in nursing, she specializes in evidence-based practices, EHR optimization, and improving outcomes in behavioral health settings. Dr. Boyles is passionate about empowering clinicians with the tools and strategies needed to deliver high-quality, patient-centered care.