Dual Diagnosis:
Fentanyl Addiction and Mental Health
Exploring the Connection and Importance of Addressing Co-Occurring Conditions in Treatment
Linked to devastating fentanyl addiction symptoms and unparalleled numbers of overdoses, fentanyl has been receiving high levels of attention for being a powerfully addictive and deadly substance. Fentanyl has plenty of legitimate medical uses, but the drug’s tendency to be illicitly manufactured and added to other drugs increases the dangers.
Fentanyl is connected to numerous negative consequences of use, including addiction, physical dependence, withdrawal, and overdose death. Fentanyl is also associated with a variety of psychological harms. People who use fentanyl may be more likely to have other mental health disorders, and people with mental health disorders may be more likely to use fentanyl.
When someone has a mental health disorder as well as a substance use disorder, they have co-occurring or concurrent mental health and addictions concerns. Clinicians must do their best to accurately assess and appropriately treat any and all co-occurring disorders in a collaborative and comprehensive way. Otherwise, the client’s health and well-being will be compromised.
Instant Download: Comprehensive Dual Diagnosis Assessment Checklist
Download this screening for fentanyl use disorder and co-occurring mental health conditions.
Fentanyl Addiction: An Overview
Despite its notoriety on the news and the fact it has been produced since the 1960s, many people do not fully understand fentanyl and how it came to be responsible for a huge proportion of drug overdose deaths. As a therapist, understanding what fentanyl is and how your client is consuming it will be essential to accomplish treatment goals.
Fentanyl is an extremely powerful opioid. As an opioid, fentanyl shares many similarities to everything from heroin and opium to morphine, hydrocodone, and methadone.(1) There is one major difference between fentanyl and these other drugs - power. Fentanyl is about 100 times more potent than morphine and 50 times more powerful than heroin.2
Fentanyl is legal and widely-prescribed to treat severe, chronic pain, especially pain caused by cancer. The substance is available in a variety of forms including:1
- Fentanyl lollipops
- Buccal tablets
- Under-the-tongue tablets
- Mouth sprays
- Nose sprays
- Patches to place on skin
- Injectable liquid
In 2021, fentanyl was prescribed 2.4 millions times, which is more than a 50% reduction from the drug’s height in 2016.(1) Fentanyl, like other opioids, may be abused by taking more of the drug and or using it in ways other than prescribed. It may also be stolen from individuals, doctors, and pharmacies, leading to fentanyl addiction symptoms.
Legal fentanyl is a concern, but the major issue fueling fentanyl’s role in the opioid epidemic is illicitly made versions of the drug. Because the drug is so powerful, drug traffickers will press pills with fentanyl or add it to other substances to increase or alter the high.(2) As mentioned, fentanyl’s problem is its power, so a miscalculation in amount can trigger a dangerous overdose and death. The power is also responsible for high levels of fentanyl addiction symptoms, dependence, and a very uncomfortable fentanyl withdrawal process when use stops.
Changing Patterns of Fentanyl Use in the Opioid Epidemic
Even mental health and addiction professionals who are familiar with fentanyl may be surprised to know that the face of fentanyl use in the U.S. is changing. Fentanyl use and changes continue to occur in waves with the fourth wave happening now.
The four waves of opioid and fentanyl use in America are:3
- Wave one: Prescription opioids. Medications like oxycodone, hydrocodone, and fentanyl prescribed at high levels for both acute and chronic pain.
- Wave two: Heroin overdoses. As citizens were addicted to and dependent on opioids, they encountered issues when doctors began to reduce prescriptions. Without the same ready access to prescriptions, many turned to heroin to achieve the wanted effects of opioids.
- Wave three: Illicit fentanyl. As the market for illegal forms of opioid increased, the production of illicitly manufactured fentanyl exploded. These substances are challenging to identify and extremely powerful with the ability to trigger an overdose to unsuspecting users. In addition to fentanyl, there are other drugs that have a similar structure to the drug including acetylfentanyl, furanylfentanyl, and carfentanil.4
- Wave four: Fentanyl, cocaine, and methamphetamine. Using opioids like fentanyl or heroin in combination with stimulants like cocaine is nothing new, but the landscape has shifted recently. Rather than someone choosing to mix the two substances, fentanyl is being mixed into the cocaine and meth without the person knowing what they are consuming. The result is higher rates of overdose.
It’s likely that the evolution of the opioid crisis will continue for sometime, and it seems apparent that fentanyl will play a significant role.
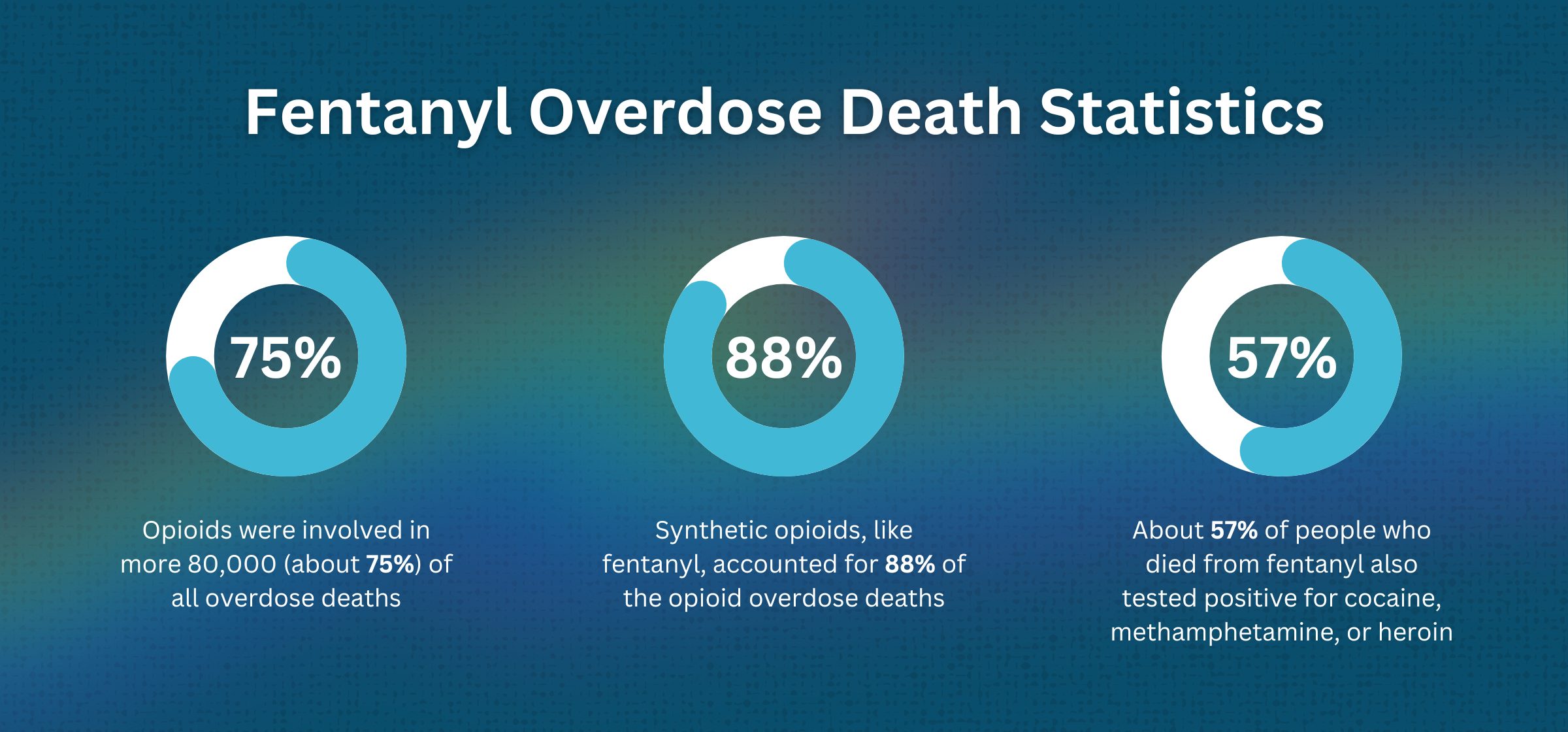
Fentanyl Overdose Death Statistics
In 2021, there were about 107,000 deaths connected to drug overdoses. Fentanyl and other opioids carried a lot of responsibility.4
- Opioids were involved in more 80,000 (about 75%) of all overdose deaths
- Synthetic opioids, like fentanyl, accounted for 88% of the opioid overdose deaths
- Overdose deaths involving fentanyl and stimulants greatly increased in recent years
- About 57% of people who died from fentanyl also tested positive for cocaine, methamphetamine, or heroin5
Because of the high risk of death from fentanyl overdose, it is valuable for therapists to understand the use of naloxone and other life-saving medications and have ready access to the opioid blockers when working with people dealing with opioid addictions.2 Learning how to treat fentanyl addiction symptoms is necessary to begin reducing deaths.
Mental Health Disorders: A Complex Landscape
Therapists understand that mental health disorders are complex and difficult to accurately identify, especially when co-occurring conditions are present. Someone with bipolar disorder may present completely differently than a person with bipolar disorder and an opioid use disorder. Working to appropriately assess, diagnose, and treat someone with concurrent mental health and substance use conditions is an essential part of therapy.
Common Mental Health Disorders Linked to Fentanyl Addiction
When a person uses fentanyl, they are at greater risk of certain medical and mental health conditions. Being aware of these connections can put people in a better position to evaluate and treat the individual.
Some medical conditions that are frequently connected to fentanyl addiction and opioid use disorders include:9
- Viral infections like HIV and hepatitis C
- Bacterial infections
- Sexually transmitted infections from risky drug use
- Frequent bumps, bruises, and injuries from poor coordination
- Insomnia
Though these medical conditions can be serious, the risk of mental health conditions linked to fentanyl use can be even more impactful. Someone using fentanyl can experience mental health conditions like:9
- Other substance use disorders, including alcohol, stimulants, cannabis, and sedative use disorders
- Persistent depressive disorder, formerly called dysthymia
- Major depressive disorder
- Bipolar disorders
- Post-traumatic stress disorder (PTSD)
- Antisocial personality disorder
- Borderline personality disorder
- Schizotypal personality disorder
- Conduct disorder in children and teens
Symptoms of these mental health conditions may present at different points of use. For example, when someone is under the influence of fentanyl, they could appear very depressed with low mood, low energy, low motivation, and increased sleeping. During withdrawal, they could show symptoms of bipolar disorder by presenting with irritability, insomnia, and high energy.
The ability of fentanyl to trigger a range of mental health symptoms at different phases of use speaks to the importance of clear assessments and conceptualizations of the client. Just because they are showing some symptoms in some situations does not mean there is an obvious mental health issue. Substance use always complicates the clinical picture.
Fentanyl Addiction and Mental Health: A Bidirectional Relationship
The link between fentanyl and psychological conditions leads professionals to wonder which came first and if one of the issues created the other issue. These questions are common when two conditions have a bidirectional relationship - fentanyl use makes mental health conditions worse and mental health conditions makes fentanyl use worse. Patterns like this are common throughout mental health and physical health conditions.
For some clients, fentanyl use is an effect of poor mental health. A person who is depressed, dealing with PTSD symptoms, or managing the impact of a personality disorder may see fentanyl as a way to manage feelings. When used for self-medication, fentanyl can produce a calming and euphoric state where the person feels relaxed, sleepy, and happy.(1) Of course, fentanyl abuse in these situations is a negative coping skill and use will only lead to additional concerns in time.
Other clients will see fentanyl use create new symptoms of mental health conditions. A person who is functioning well before fentanyl use may quickly develop serious mental health symptoms associated with depression or other mental health conditions. These opioid-induced disorders may be challenging to detect and diagnose, especially as time goes by. Even though fentanyl created these symptoms, the symptoms will remain long after use ends. A period of fentanyl use can create unwanted effects that last a lifetime.
Understanding the Connection
Every person has their own motivation to use substances, but no one ever sets out with the goal of becoming addicted to a drug like fentanyl. No one wants to experience an overdose of the drug, but their mental state can substantially interfere with their decision making.
Substance use is appealing in the short-term for various reasons with people using drugs to:
- Feel good. They want to experience the pleasurable effects of the drug.
- Feel better. Self-medicating their uncomfortable physical or mental health symptoms.
- Experiment. A number of teens and adults will become curious and try fentanyl to have the experience.
- Perform better. Some will look at the performance-enhancing effects of a drug and imagine situations and scenarios where using the substance will help them perform a task at a higher level.
People may be drawn to substance use for one of the reasons above, or they could be influenced by a combination of two or more factors.
Common Risk Factors Leads to Dual Diagnosis
Another aspect creating a connection between fentanyl use and mental health conditions are the shared risk factors for each. If a person has experienced a significant life event or has some type of genetic predisposition, it could trigger an addiction, a mental health condition, or both.6
Some of the most common risk factors that contribute to substance use and mental health disorders include:6
- Genetic vulnerabilities. A person’s heredity accounts for about 50% of their risk to substance use and mental health conditions. These genetic differences are complex and can dramatically impact the way the brain responds to stress as well as alcohol and other drugs. Neurotransmitter action may be controlled by genes that influence levels of serotonin and dopamine in the brain.
- Brain region changes. Several parts of the brain have a huge influence on both addiction and mental health concerns. Substance use disorders, depression, schizophrenia, and other psychiatric conditions can become more likely if these regions are disrupted or damaged.
- Trauma and other adverse childhood experiences (ACEs). High rates of trauma, whether acute or chronic, puts people at high risk for substance use and mental health conditions, like depression and PTSD. For example, recent studies show 16% of military service members had an untreated substance use disorder and 8% had serious psychological distress. These rates are much higher than the general population.
- Environmental experience. Living in a situation that lacks safety, financial security, and educational or employment opportunities puts people in a vulnerable situation, which frequently leads to addiction and psychological problems.
Stress is a theme in the risk factors for dual diagnosis. When people experience high levels of stress, they are prone to co-occurring disorders. Unfortunately, much of this stress is outside of the individual’s control. They may have limited ways to decrease their stress effectively.
Accurate Dual Diagnosis Assessment
Without accurate evaluation of dual diagnosis conditions, effective treatment is impossible. The situation becomes more complicated when the client is not open and honest about their mental health symptoms and the frequency, intensity, and duration of their opioid use. Since fentanyl is routinely mixed with other substances, the client may not even realize they have consumed the drug.
The best tool a therapist has to screen opioid use and mental health symptoms is the ability to quickly build trust and rapport with their client. If the client feels uncomfortable, judged, or intimidated, they may deny, minimize, or deflect from their symptoms.
A simple interview can expose signs and symptoms of mental health and substance use disorders. All screenings should include information about prescription or illicit opioid use. Consider asking:7
- What drug was used?
- How was it used?
- What was the dose and frequency of use?
- What was the desired outcome of use?
- Was the drug combined with alcohol or other drugs?
- How do you feel when you don’t use the drug?
The answers can help direct the next line of questioning and determine the need for a more structured screening tool. The National Institute on Drug Abuse offers a list of helpful screening tools for clinicians to assess for mental health and substance use disorders. The group also offers the ASSIST brief screening tool to identify substance use concerns.
Clinicians may also consider using objective screenings like blood or urine tests to assess
Treatment Approaches for Dual Diagnosis
Knowing how to treat fentanyl addiction is essential, and treatment for dual diagnosis conditions must take place in a comprehensive way that accounts for the whole person, not only their disorders. Though there may be a desire to move treatment along quickly, better outcomes are linked to longer courses, so therapists should offer or refer clients to differing levels of aftercare to continue the recovery process.
Medication Assisted Treatment
With opioid addictions and opioid use disorders, Medication Assisted Treatment (MAT), sometimes called Medications for Opioid Use Disorders (MOUD), could be essential. MAT or MOUD focus on providing opioid agonists or opioid antagonist to aid the recovery process by:7
- Limiting withdrawal symptoms
- Reducing cravings
- Create periods of symptom stability
MAT is not trading one addiction for another. The medications used help break the pattern of extreme highs and lows linked to substance use disorders. They create consistency and predictability that make recovery more likely.
Some medications used include:7
- Methadone
- Buprenorphine
- Naltrexone
The best Medication Assisted Treatment programs will offer therapeutic interventions that address underlying contributors of addiction and mental health concerns. Additionally, in an effort to treat all symptoms, the client may be offered medications to alleviate the symptoms of depression, anxiety, and any other mental health conditions.
Integrated Dual Diagnosis Treatment (IDDT)
Integrated dual diagnosis treatment (IDDT) surrounds the individual with services to establish a period of recovery and well-being. With a team of providers using stage-wise interventions and comprehensive mental and physical health services, IDDT aims to reduce the unwanted outcomes of co-occurring disorders like homelessness, incarceration, hospitalizations, disease, and death.8
IDDT can help:8
- Establish appropriate continuity of care that allows for a range of needs to be met
- Tangible quality of life outcomes
- Stable house
- Stable employment
- The ability to live independently
- Longer periods of recovery
- Decreased psychiatric symptoms
Integrated dual diagnosis treatment is focused on short-term solutions to quickly put the client on a path to opportunity and sobriety.
Psychotherapy and Behavioral Interventions
No matter the form of treatment or level of care, psychotherapy and behavioral interventions will be a key feature of dual diagnosis treatments. Some of the commonly used, effective treatments include:7
- Cognitive behavioral approaches. Cognitive behavioral therapy (CBT) is regarded as a leading treatment for a range of substance use and mental health conditions. It can help clients build awareness of their thoughts, feelings, and behaviors.
- Contingency management (CM). CM helps treat dual diagnosis conditions by offering clients real-life rewards for participating in treatment and completing recovery-focused activities.
- Motivational interviewing (MI). MI aims to build the client’s internal motivation for change, rather than relying on outside pressures to create change.
- Structured family treatment. Family therapy options acknowledge that a person’s mental health symptoms don’t exist in a vacuum. Family and friend influences affect symptoms, so bringing family members into session can shift the dynamics and improve communication skills to lower symptoms.
Therapists may utilize a combination of behavioral interventions or stick to their preferred intervention.
Challenges in Dual Diagnosis Treatment
Dual diagnosis conditions are complex, intrusive, and at times unpredictable. Treating these conditions poses many challenges, but therapists who are aware of these obstacles put themselves in a position better able to manage the difficulties.
Some of the most significant challenges to treating co-occurring disorders are:
- Stigma. Sometimes, getting the client to acknowledge their conditions is the biggest challenge. Clients who feel stigmatized by admitting their issues may avoid or resist treatment.
- Limited access. The availability of therapists who are adept at managing dual diagnosis clients may be poor. More therapists are needed to meet the demand.
- Compliance and relapse. Clients in early recovery are going to be at risk of relapse. Triggers, urges, and cravings can lead to poor compliance and lapses that threaten treatment.
- Few aftercare programs. Treatment must be available on a continuum, so people with intense symptoms can receive intense care and other options are available to people with other symptoms. Gaps in care can lead to relapse.
Lack of trauma-informed care. Trauma is a major driver of mental health and addiction issues, so treatment should consider the impact. Without addressing the role of trauma, therapists might find the client misconceptualized.
Final Thoughts
The combination of fentanyl use disorder and another mental health condition poses a challenge to even the most seasoned mental health clinician. Understanding the combination, where it originates, and appropriate treatment options can put the professional in a better position to effectively treat symptoms.
About the Author

Eric Patterson, MSCP, NCC, LPC
Eric Patterson, MSCP, NCC, LPC, is a professional counselor who has been working for over a decade to help children, adolescents, and adults in western Pennsylvania reach their goals and improve their well-being.
Along the way, Eric worked as a collaborating investigator for the field trials of the DSM-5 and completed an agreement to provide mental health treatment to underserved communities with the National Health Service Corp.
Sources
- Drug Enforcement Administration. (2023). Fentanyl.
- American Psychiatric Association. (2022). Opioid Use Disorder.
- Ahmed, S., Sarfraz, Z., Sarfraz, A. (2022). Editorial: A Changing Epidemic and the Rise of Opioid-Stimulant Co-Use. Frontiers in Psychiatry.
- Centers for Disease Control and Prevention. (2023). Drug Overdose Deaths.
- National Institute on Drug Abuse. (2020). Common Comorbidities with Substance Use Disorders Research Report.
- American Psychological Association. (2018). The Opioid Guide: A Resource for Practicing Psychologists.
- Case Western Reserve University. (n.d.). Integrated Dual Disorder Treatment.
- American Psychiatric Association. (2022). Diagnostic and Statistical Manual of Mental Disorders (5th ed., text rev.).