Blog > Treatment Strategies > Mental Status Exam Cheat Sheet + Examples
Mental Status Exam Cheat Sheet + Examples and Templates
Accurate mental status exams (MSEs) are a core part of clinical documentation. This guide gives you a practical way to assess and record MSEs across all key domains, including mood, cognition, speech, insight, and more. You’ll get ready-to-use MSE examples, standardized phrases, and a downloadable cheat sheet you can apply in your notes right away.

Last Updated: December 4, 2025


What You'll Learn
-
The purpose and clinical value of the Mental Status Exam—and how it differs from cognitive screening tools like the MMSE.
-
How to assess and document each MSE domain, including appearance, behavior, speech, mood/affect, thought process, thought content, perception, and cognition.
-
Clinically useful descriptors, prompts, and examples you can use immediately in your notes.
-
How to identify red flags—such as psychosis, suicidal ideation, or cognitive decline—that require urgent intervention.
-
How to adapt the MSE for clients with cultural differences, language barriers, or low literacy.
-
Sample MSE write-ups for common clinical presentations, including depression and anxiety.
-
Practical tips to strengthen documentation clarity, accuracy, and defensibility.
-
How ICANotes streamlines mental status exam documentation using structured templates and automated narrative generation.
Clear and consistent MSE documentation supports better treatment decisions, continuity of care, and compliance with medical and insurance standards. As workloads grow and expectations increase, having a reliable method for charting mental status helps clinicians work more efficiently without missing essential details.
What Is a Mental Status Exam?
A Mental Status Exam (MSE) is a structured way to assess and document a client’s current cognitive and behavioral functioning. It captures key observations across areas like appearance, mood, speech, cognition, perception, and thought patterns.
Clinicians use the MSE to form diagnostic impressions, track changes over time, and support treatment planning. Unlike the Mini-Mental State Exam (MMSE), which focuses on cognitive screening, the MSE offers a broader view of a person’s psychological and emotional state during a specific encounter.
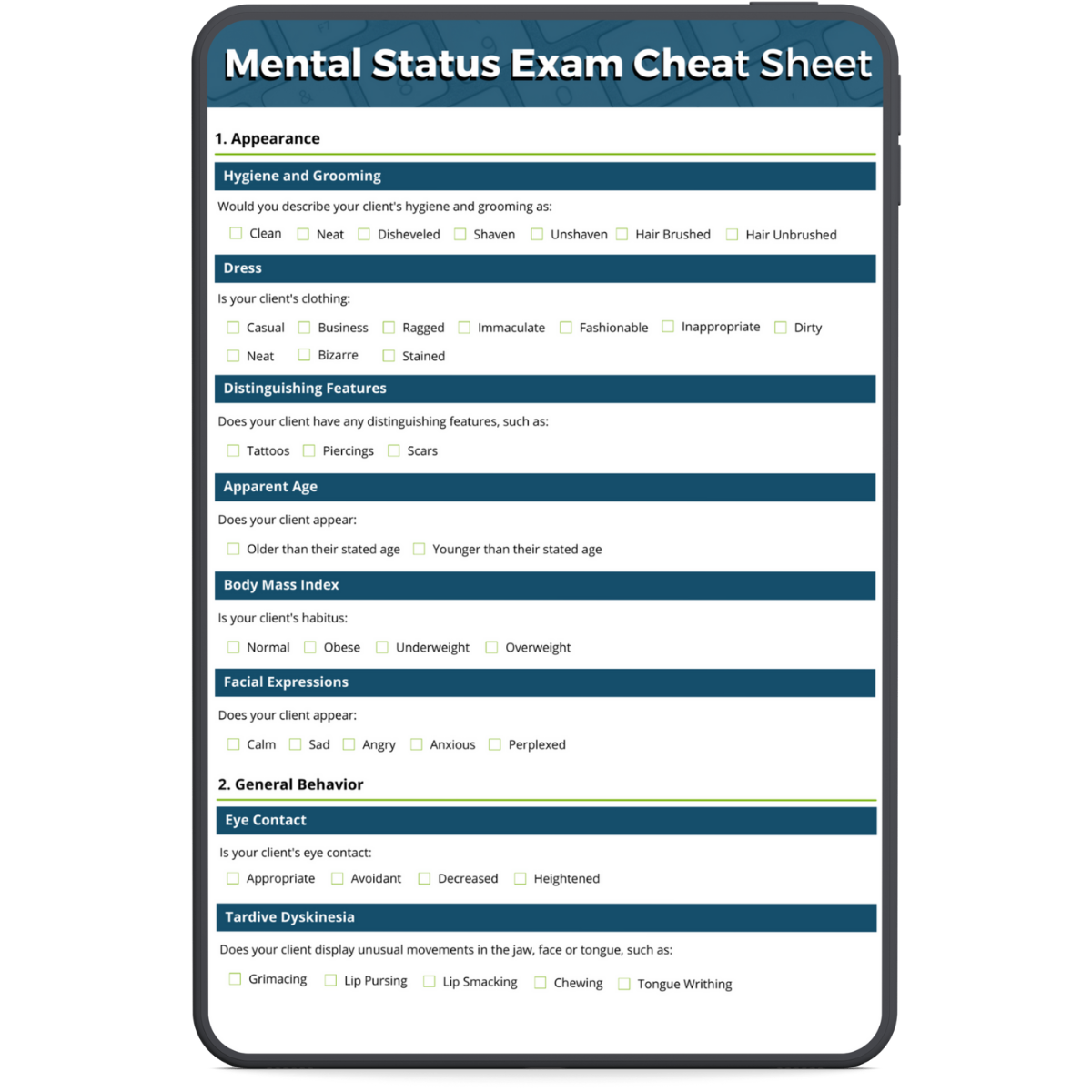
Download our
Mental Status Exam Cheat Sheet
Download our free mental health status exam cheat sheet to use as a handy reference when performing a mental status exam.
Why are Mental Status Exams Important?
The Mental Status Exam offers a structured snapshot of a client’s emotional and cognitive functioning at a specific moment. It’s a key part of every mental health assessment and supports clinical decision-making in several important ways:
- Establishes a baseline for the client’s current mental state
- Supports accurate diagnosis by identifying symptoms and patterns
- Tracks progress or deterioration over time
- Guides treatment planning by revealing areas that need intervention
- Improves care coordination through clear documentation shared across providers.
The MSE is especially valuable at intake, during clinical changes, or when coordinating care with other professionals. It helps ensure that both immediate concerns and long-term patterns are clearly understood and documented.
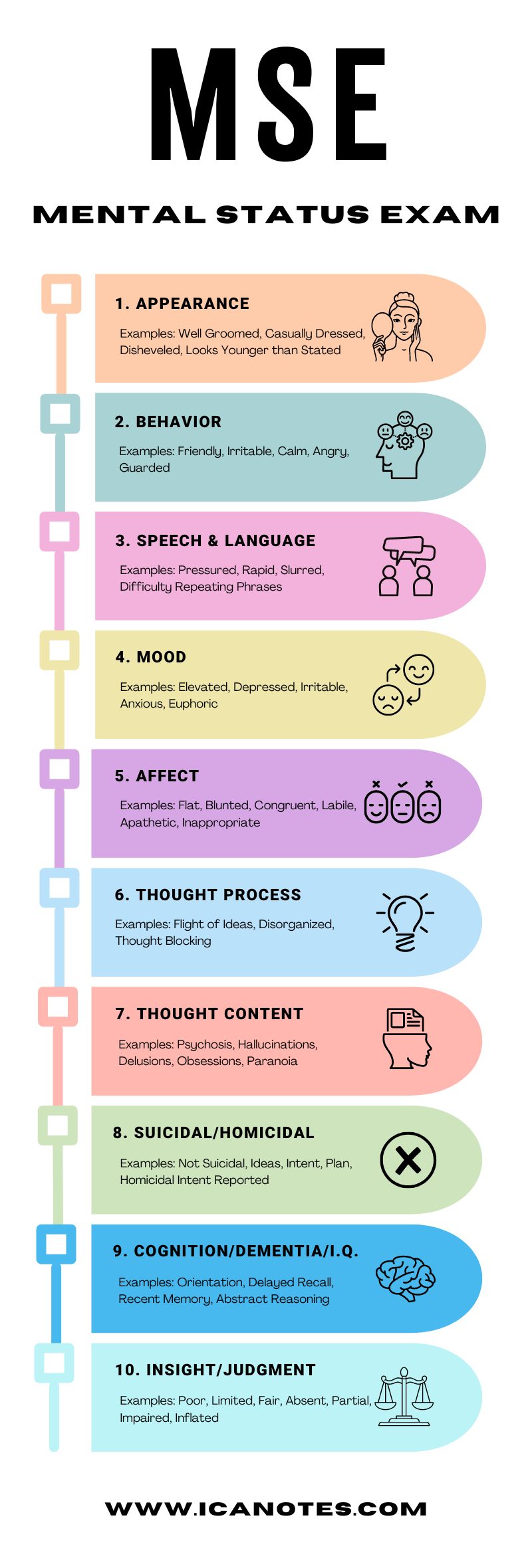
What are the Components of a Mental Status Exam?
- Appearance
- General behavior
- Speech and language
- Emotions
- Thought and perception
- Cognition
How to Perform a Mental Status Exam: MSE Checklist
A mental status exam checklist helps clinicians observe and document key areas of a client’s mental functioning. While each session is different, the checklist below covers the core elements typically assessed and serves as a quick reference during documentation.
1. Appearance
Appearance refers to how the client presents physically during the session. This includes hygiene, grooming, clothing, posture, facial expression, and overall physical state. These observations offer insight into the client’s level of functioning, mood, and potential psychiatric symptoms. Look for signs of self-neglect, disorganization, or distress, and document objectively.
Example:
The client appears older than their stated age. Disheveled, with stained clothing and poor hygiene. Avoids eye contact and sits with a slouched posture.
Assessment Prompts:
- “How do you usually get ready for the day?”
- “Have you noticed any changes in your daily routines or energy levels?”
2. General Behavior
General behavior refers to how the client moves, responds, and engages during the session. This includes their motor activity, eye contact, use of gestures, and overall cooperativeness. These observations can reflect a client’s emotional state, level of distress, neurological function, or possible side effects of medication. Note any signs of hostility, guardedness, or disinhibition.
Example:
The client sits rigidly, avoids eye contact, and displays frequent lip smacking. Motor activity is tense but controlled. Guarded attitude throughout the session.
Assessment Prompts:
- “How are you feeling about today’s session?”
- “Have you noticed any changes in your movement or body sensations lately?”
Share this graphic by copying the following HTML code
[copy] <p><strong>www.icanotes.com</strong><br /><br /><a href='https://www.icanotes.com/2021/03/31/mental-status-exam-cheat-sheet/?fl_builder&fl_builder_ui'><img src='https://www.icanotes.com/wp-content/uploads/2021/03/MSE-infographic-2024-1.jpg' alt='MSE infographic 2024 (1)' width='800' /></a></p>
3. Speech & Language
Speech patterns offer insight into a client’s cognitive and emotional state. Evaluate how clearly the client speaks, the speed and rhythm of their speech, and the quality of their verbal expression. Disruptions may indicate mood disorders, anxiety, thought disorganization, or neurocognitive impairment. Pay attention to fluency, articulation, tone, and vocabulary use.
Example:
Speech is slow and soft, with a delayed onset. Responses are brief but coherent. Tone flat, articulation clear.
Assessment Prompts:
- “Has anyone mentioned changes in the way you speak lately?”
- “Do you feel like it’s harder to find words or express yourself clearly?”
4. Emotions
Assess the client’s emotional state by combining what they report (mood) with what you observe (affect). Mood is the client’s subjective experience, while affect is the outward expression of that emotion. Take note of emotional range, stability, intensity, and whether their affect is congruent with what they describe. These cues help identify mood disorders, anxiety, or trauma-related symptoms.
Example:
The client reports feeling “fine.” Affect is flat, with minimal expression and a monotone voice. Mood and affect appear incongruent.
Assessment Prompts:
- “How have you been feeling over the past few days?”
- “Would you say your emotions have been steady or up and down lately?”
5. Thought & Perception
This section evaluates how a client’s thoughts are organized and what they focus on. Assess whether their thinking is logical and coherent or disorganized, scattered, or overly detailed. Also listen for signs of distorted content, such as delusions, obsessions, or suicidal ideation. Ask directly about hallucinations or unusual beliefs when needed, and document clearly if any safety concerns arise.
Example:
The client displays a tangential thought process, frequently veering off-topic. Reports obsessive worry and occasional visual hallucinations. Denies suicidal or homicidal ideation.
Assessment Prompts:
- “Do you find it easy to focus or follow through on your thoughts?”
- “Have you ever seen or heard things that others don’t?”
- “Do you ever have thoughts that feel intrusive or hard to stop?”
6. Cognition
Cognitive assessment helps determine how well a client processes information, recalls memories, and maintains awareness. It also provides insight into conditions like dementia, delirium, or trauma-related cognitive changes. Use this section to evaluate orientation, attention, memory, impulse control, insight, and judgment. If you suspect cognitive impairment, consider adding tools like the MMSE or MoCA.
Example:
The client is alert and oriented to person, place, and time. Their attention span is fair, but they are easily distracted. Recalls 2 out of 3 words after 5 minutes. Insight and judgment are limited regarding treatment needs.
Assessment Prompts:
- “Can you tell me where we are and what today’s date is?”
- “I’ll say 3 words — can you repeat them back to me and remember them for later?”
- “What would you do if you smelled smoke in a building?”
7. Environment
When conducting a mental status exam in the client’s home or residential setting, their physical surroundings can offer important clues about cognitive functioning, reality testing, and self-care capacity. Environmental observations often supplement findings related to thought content, judgment, and overall functioning.
Example:
The client’s apartment is cluttered with stacks of newspapers and unused items. Furniture is positioned to block the front door. Reports feeling safer with this arrangement.
Assessment Prompts:
- “Tell me about how you organize your home space. Has anything changed recently?”
- “Do you feel comfortable and safe where you’re living?”
- “Can you walk me through your typical day at home?”
Mental Status Exam Examples
The following mental status examination sample write-ups show how to document observations across key domains like mood, cognition, and behavior. Use these as templates to support clear, consistent MSE documentation in clinical practice.

Mental Status Exam Example #1: Major Depressive Episode
Client: Maria R., 38-year-old Hispanic female
Reason for Visit: Worsening depressive symptoms over several weeks
Appearance: Appears to be of stated age. Casually dressed, hair unkempt, minimal makeup. Mild body odor noted. Slouched posture.
Behavior: Psychomotor slowing observed. Avoids sustained eye contact but remains cooperative. No abnormal movements.
Speech: Low volume, slow rate, monotone tone. Answers are brief but coherent.
Mood and Affect: Reports feeling “empty” and “exhausted.” Affect is constricted and congruent with the stated mood.
Thought Process: Logical and goal-directed, but slowed. No flight of ideas or tangentiality.
Thought Content: Endorses passive suicidal ideation (“I sometimes think people would be better off without me”) without plan or intent. No delusions, obsessions, or phobias.
Perception: Denies hallucinations or perceptual disturbances.
Cognition: Alert and oriented to person, place, time, and situation. Attention mildly impaired; difficulty with serial 7s. Immediate and recent recall intact (3/3 words). Remote memory intact.
Insight and Judgment: Insight is fair. Acknowledges need for treatment. Judgment intact for daily decisions.
Reliability: Considered reliable. Responses were consistent and plausible.
Summary: Presentation consistent with a moderate depressive episode. No imminent safety risk, but requires treatment planning and follow-up.

Mental Status Exam Example #2: Acute Anxiety with Panic Disorder
Client: Derrick W., 29-year-old White male
Reason for Visit: Episodes of intense anxiety and difficulty concentrating
Appearance: Appears slightly younger than stated age. Clean, casually dressed. Frequent fidgeting noted.
Behavior: Restless, frequently shifts in seat. Good eye contact. No tics or involuntary movements.
Speech: Rapid rate with normal volume and articulation. Occasional pressured quality when describing symptoms.
Mood and Affect: Describes mood as “on edge” and “wired.” Affect anxious, with quick shifts in expression when discussing panic attacks.
Thought Process: Linear but occasionally distractible. No evidence of thought blocking or loose associations.
Thought Content: Reports excessive worry, rumination, and fear of future panic episodes. Denies suicidal or homicidal ideation. No delusional themes.
Perception: Denies hallucinations. Reports occasional derealization during panic episodes (“feels unreal”).
Cognition: Alert and oriented x4. Attention intact; performs serial 7s without difficulty. Memory intact. Abstract thinking is appropriate.
Insight and Judgment: Insight is good; recognizes symptoms as anxiety-related. Judgment intact.
Reliability: Reliable historian. Descriptions are detailed and consistent.
Summary: Findings support generalized anxiety with panic symptoms. No acute safety concerns; appropriate for outpatient treatment and monitoring.
Mental Status Exam Template and Cheat Sheet (Free PDF)
To make your MSE documentation easier, we’ve created a free mental status exam cheat sheet you can download and use during sessions or chart reviews.
What’s Inside:
- Complete MSE categories, from appearance to cognition and environment.
- Clinically relevant descriptors for quick point-and-click use.
- Prompts and examples to guide your assessments and improve chart clarity.
- A structured format that mirrors ICANotes' built-in documentation tools.
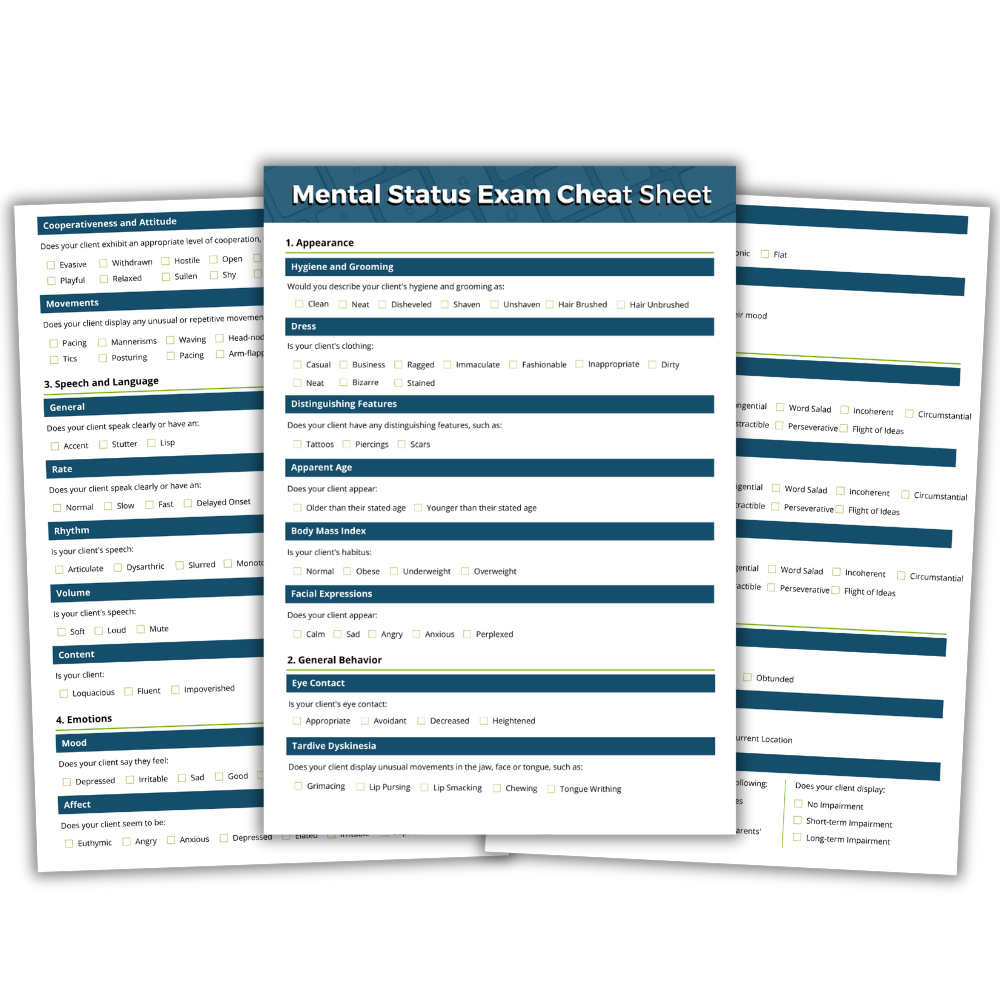

Download our
Mental Status Exam Cheat Sheet
Download our free mental health status exam cheat sheet to use as a handy reference when performing a mental status exam.
Tips for Documenting a Mental Status Exam
Effective documentation of a mental status exam ensures that clinical observations are clear, useful, and defensible. These tips will help you document each session with greater accuracy and efficiency.
Observe Before Documenting
Begin by quietly observing the client’s behavior, appearance, and communication before asking structured questions or checking boxes.
First impressions are often the most revealing. Noting things like posture, clothing, grooming, and energy level during the first few minutes can give you an authentic baseline that scripted questions might not capture.
Use Objective and Descriptive Language
Your documentation should reflect what you can directly observe or what the client explicitly says. Avoid vague or subjective terms like "seems sad" or "looks anxious." Instead, describe the behavior: "Client avoided eye contact, sat hunched over, and spoke in a low tone." This type of language is clearer to other providers and strengthens the clinical value of your note.
Include Direct Quotes When Appropriate
Using the client’s exact words can provide valuable insight into their mental state, especially when describing mood, thought content, or delusions. For example, “I think I’m being followed” gives a clearer picture than a paraphrased summary. Use quotes selectively and sparingly to highlight key expressions that are clinically significant.
Customize Your Documentation
Templates and checklists are helpful for structure, but overusing them can make notes feel generic or inaccurate. Always tailor the note to reflect the specific client’s presentation and behavior during the session. This ensures the documentation aligns with what actually occurred and avoids errors from autopopulated language.
Clearly Document Any Safety Concerns
Always take special care when documenting risk factors such as suicidal ideation, homicidal ideation, or psychotic symptoms. Be specific about what the client reported, how you assessed risk, and what actions you took. For example, “Client endorsed passive thoughts of suicide without plan or intent. Denied current suicidal or homicidal ideation. Safety plan reviewed and discussed.”
Be Concise But Thorough
Aim to write notes that are easy to read but include all essential information. A well-organized mental status exam doesn’t need to be long, but it should touch on each major domain. Bullet points and structured subheadings can help organize the note while keeping it readable.
Consider Cultural Context
A client’s behavior and communication are influenced by cultural background, language, and life experience. What appears to be a lack of eye contact, restricted affect, or guardedness may be culturally appropriate or trauma-informed behavior. When in doubt, ask clarifying questions and avoid making assumptions based solely on presentation.
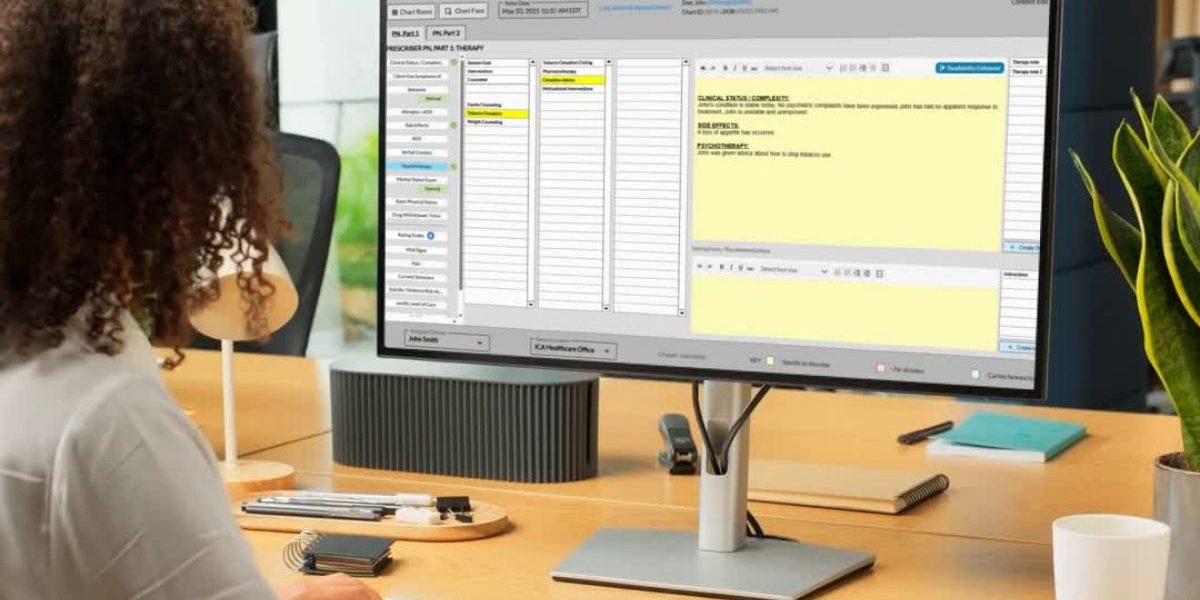
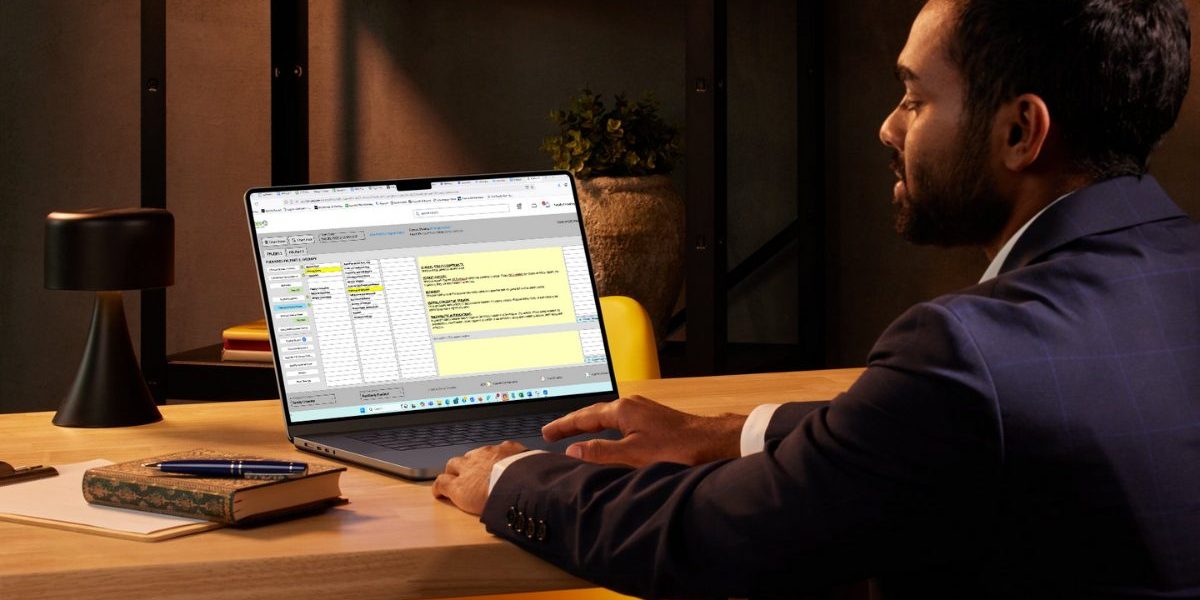
Using ICANotes to Document Mental Status Exams
ICANotes makes mental status exam documentation fast and accurate with built-in tools designed for behavioral health.
Pre-Built MSE Template: Choose from clinical descriptors for appearance, mood, cognition, and more.
Instant Narrative Generation: Automatically creates a complete MSE note from your selections.
Customizable Format: Add, remove, or adjust sections to fit your workflow.
Integrated and Secure: Document directly in your EHR with HIPAA-compliant data protection.
Start your free trial today and simplify your MSE documentation with ICANotes.
Start Your Free Trial of ICANotes
Accurate and efficient documentation is essential for delivering quality behavioral health care. ICANotes simplifies the process with a clinically robust EHR software designed specifically for mental health professionals.
Our intuitive system comes preloaded with comprehensive templates for every setting and discipline, allowing you to create:
✅ Discharge summaries
✅ Group therapy notes
✅ Initial assessments
✅ Progress notes
✅ Treatment plans
Experience the EHR that thinks like a clinician. Try ICANotes for free today!
Frequently Asked Questions
Dr. October Boyles is a behavioral health expert and clinical leader with extensive expertise in nursing, compliance, and healthcare operations. With a Doctor of Nursing Practice (DNP) from Aspen University and advanced degrees in nursing, she specializes in evidence-based practices, EHR optimization, and improving outcomes in behavioral health settings. Dr. Boyles is passionate about empowering clinicians with the tools and strategies needed to deliver high-quality, patient-centered care.