Credentialing Is Not Clerical: Why Compliance Failures Stop Payment
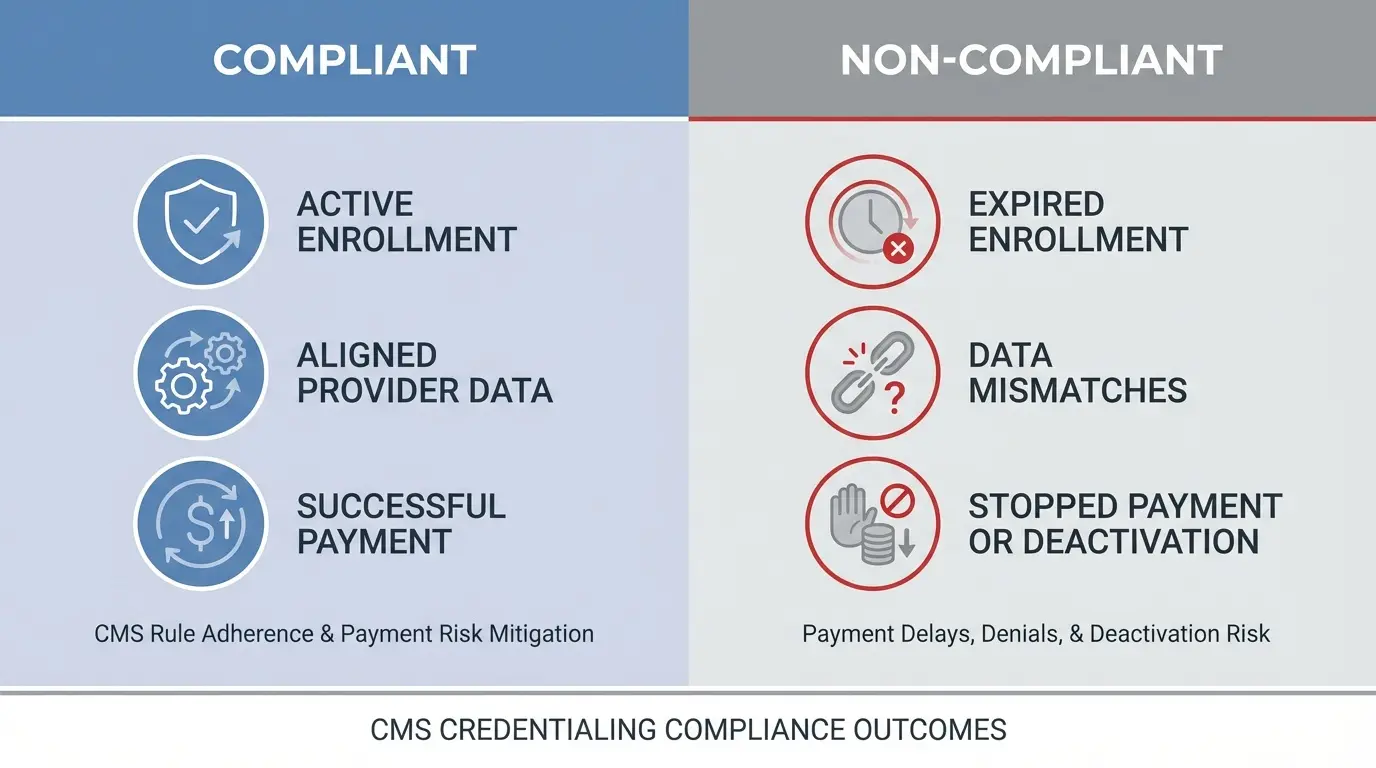
Credentialing failures are one of the most common — and least understood — reasons clinicians lose payment, panel status, and billing privileges. This article explains why CMS, NCQA, and payers treat credentialing as a strict compliance requirement, and how even small data mismatches can trigger denials, deactivations, and long-term revenue disruption.

Last Updated: February 13, 2026
Credentialing is a Compliance Gatekeeper, Not Paperwork
If you have ever wondered why highly trained clinicians can deliver excellent care and still end up unpaid, unpaneled, or suddenly deactivated, the answer is rarely clinical.
It is credentialing.
Credentialing lives in that uncomfortable space between government systems, payer logic, and human error. It is not glamorous. It is not intuitive. And it is absolutely unforgiving.
From a regulatory perspective, credentialing and enrollment are not optional back-office tasks. They are safety, quality, and payment gatekeepers. Miss a step, miss a deadline, or let your data drift across systems, and the consequences arrive fast … and usually without mercy.
Let’s talk about why.
CMS Is Clear — and Unforgiving — About Credentialing Rules
Medicare Enrollment, PECOS, and Deactivation Risk
The Centers for Medicare & Medicaid Services (CMS) does not hide the rules. They publish them in clean, bureaucratic language that reads polite but carries real consequences.
“Medicare enrollment requires providers to keep their enrollment records up to date in PECOS, including ownership and practice location changes, to avoid billing interruptions.”
Translation …
If you move offices, change ownership structure, add locations, or update legal details and you do not report it correctly in PECOS, Medicare does not owe you payment. Full stop.
CMS doubles down on this point.
“Failing to revalidate your Medicare enrollment by the assigned due date can result in deactivation of billing privileges.”
Deactivation does not mean claims are delayed.
It means claims are rejected.
Retroactively.
Why “Updating One System” Is Never Enough
One of the most common traps clinicians fall into is assuming that updating one system updates them all.
It does not.
“Providers must ensure consistency between their NPI information and their Medicare enrollment records to prevent processing delays.”
NPPES, PECOS, CAQH, and payer portals do not magically sync. If your address, taxonomy, ownership, or practice details differ even slightly, you have just created your own delay.
CMS expects you to manage that alignment continuously, not when it becomes a problem.
Audit Your Insurance Credentialing Before It Costs You Revenue
Credentialing gaps often go unnoticed until claims are denied or payments stop. Use this free Insurance Credentialing Audit Worksheet to review CAQH accuracy, payer status, effective dates, and recredentialing risk — before small issues turn into lost revenue.
Why Credentialing Is a Patient Safety and Legal Risk
Credentialing as a Quality and Safety Process
Academically, credentialing is not framed as paperwork. It is framed as risk prevention.
StatPearls is blunt about this.
“Credentialing and privileging are foundational quality and safety processes that verify a provider’s qualifications before granting clinical authority.”
Credentialing answers a simple but high-stakes question…
Should this clinician be allowed to treat patients here?
How Credentialing Failures Create Malpractice Exposure
When credentialing fails, the consequences are not theoretical.
“Inadequate credentialing exposes organizations to malpractice risk, regulatory penalties, and reputational damage.”
This matters because payer enrollment, hospital privileges, and malpractice coverage are all interconnected. A gap in credentialing can ripple outward into denied claims, uncovered services, and legal exposure.
Credentialing protects patients.
But it also protects clinicians from practicing without a safety net they assumed existed.
NCQA Standards Leave No Room for Informal Processes
Primary Source Verification Requirements
If CMS is rigid, NCQA is exacting.
NCQA credentialing standards require documentation, structure, and proof… not good intentions.
“NCQA credentialing standards require organizations to use primary source verification and to document a structured review of each practitioner’s credentials.”
Primary source verification means exactly what it sounds like.
Licenses are verified at the licensing board.
DEA registrations are verified with the DEA.
Education is verified at the issuing institution.
Screenshots, assumptions, or “we’ve always done it this way” do not pass.
Common NCQA Credentialing Deficiencies
And NCQA sees the same mistakes over and over.
“Common NCQA deficiencies include missing documentation of peer review, incomplete verification, and failure to follow the organization’s own written policies.”
This is where practices quietly fail audits. Not because care was poor, but because documentation was incomplete or inconsistent.
NCQA does not penalize you for being small.
They penalize you for being sloppy.
The Same Credentialing Errors Keep Killing Cash Flow
Data Inconsistency Across CAQH, NPPES, and Payers
Across credentialing vendors, MSOs, and payer guides, the pitfalls are painfully consistent.
- “One of the most frequent credentialing pitfalls is inconsistent data across CAQH, payer applications, and NPPES, which triggers avoidable delays.”
- “Expired licenses, DEA registrations, or malpractice coverage are classic reasons payers suspend or deny network participation.”
- “Practices that wait to start credentialing until just before opening often face months of uncompensated visits while applications are still pending.”
- “Not monitoring enrollment and recredentialing dates leads to accidental lapses that disrupt cash flow and patient care.”
Data Inconsistency Across CAQH, NPPES, and Payers
This is how clinicians end up seeing patients for months and realizing none of it will be paid. Not because they were unqualified… but because the system was.
Credentialing does not forgive optimism.
Expired Credentials and Silent Network Disruptions
Data mismatches are not the only way credentialing failures drain revenue. Expired licenses, lapsed malpractice coverage, missed recredentialing deadlines, or outdated attestations can quietly remove a clinician from a payer network without any immediate warning.
In these cases, nothing appears “wrong” operationally. Scheduling continues. Care continues. Claims are submitted as usual. The failure only becomes visible when payments stop — or when claims begin denying weeks or months later for reasons that seem disconnected from the original lapse.
These silent disruptions are especially dangerous because they are often discovered after the window for retroactive correction has closed. At that point, the care has already been delivered, but reimbursement is permanently lost.
“CMS assumes your data is aligned. NCQA assumes your documentation is complete. Payers assume both. If any of those assumptions are wrong, payment stops.”
Understanding why credentialing rules are unforgiving matters — but knowing where practices actually fail is what prevents revenue loss.
The Hard Truth Clinicians Are Rarely Told About Credentialing
Credentialing is not clerical busywork.
It is not something to “circle back to.”
It is not a one-time task.
It is a living compliance obligation that sits at the intersection of patient safety, legal authority, and revenue.
CMS assumes you are monitoring PECOS.
NCQA assumes your documentation is airtight.
Payers assume your data matches everywhere.
If any of those assumptions are wrong, the system does not slow down to help you fix it.
It simply stops paying you.
And that is why credentialing is hard. Not because clinicians are incapable… but because the margin for error is essentially zero.
If no one ever explained that to you, now you know.
At ICANotes, we work closely with behavioral health practices navigating credentialing, enrollment, and billing every day. Our perspective comes from supporting clinicians through the real-world consequences of credentialing failures — and helping practices build systems that reduce risk, protect compliance, and keep payment flowing. Book a free Credentialing Consult with us today.
Need a Second Look at Your Credentialing Setup?
Credentialing failures rarely announce themselves until payment stops. ICANotes works with behavioral health practices every day to identify enrollment gaps, compliance risks, and credentialing issues that can quietly disrupt reimbursement. Our team understands the CMS, NCQA, and payer requirements that govern credentialing — and how those rules play out in real clinical and billing workflows.
Book a Free Credentialing Consult
No obligation. Designed for mental health clinicians and practice leaders.
Related Posts
About the Author
Dr. October Boyles is a behavioral health expert and clinical leader with extensive expertise in nursing, compliance, and healthcare operations. With a Doctor of Nursing Practice (DNP) and advanced degrees in nursing, she specializes in evidence-based practices, EHR optimization, and improving outcomes in behavioral health settings. Dr. Boyles is passionate about empowering clinicians with the tools and strategies needed to deliver high-quality, patient-centered care.