Blog > Practice Management > 7 EHR Problems and How to Fix Them
7 EHR Problems and How to Fix Them in Mental Health Practices
EHRs are designed to streamline documentation, enhance coordination, and improve outcomes. But for behavioral health providers, the wrong system often creates more problems than it solves. Common issues include rigid workflows, missing templates, limited data sharing, and compliance risks. In this post, you’ll learn about seven common EHR problems in mental health settings and how to fix them with the right tools and strategies.

Last Updated: December 1, 2025

Behavioral health care involves complex documentation, collaboration across teams, and coordination with external providers. These demands can quickly reveal the limitations of an EHR not built for your specialty. By understanding where common systems fall short, you’ll be better equipped to identify challenges early, avoid disruptions, and make informed decisions about improving your practice’s workflow.
How to Address Common Challenges With Electronic Health Records
When an EHR isn’t built with behavioral health in mind, it can create more problems than it solves. The wrong system can slow down documentation, disrupt care coordination, and increase administrative burden. Below is a quick comparison of common issues with EHR systems and practical ways to resolve them.
| EHR Problem | How to Fix It |
|---|---|
| Workflows that don’t match mental health care | Adjust your EHR configuration to match clinical needs or choose a behavioral health platform. |
| Resistance from staff | Provide role-specific training and assign peer mentors to support adoption. |
| Integration failures | Choose an EHR with HL7, CCD, secure fax, and clearinghouse connections, and test all workflows. |
| Data gaps from migration | Involve clinical staff in data mapping and run validation checks after migration. |
| Inefficient documentation | Use structured templates, smart phrases, and auto-coding to reduce charting time. |
| Compliance concerns | Select an EHR with HIPAA and 42 CFR Part 2 features like access control and audit trails. |
| Rigid or missing templates | Build or select templates tailored for behavioral health documentation needs. |
1. Workflows That Don’t Match Mental Health Care
Many EHRs were originally built for general medicine and don’t align with the specific needs of behavioral health providers. This can make tasks like documenting therapy sessions, tracking group treatments, or managing psychiatric medications more difficult than they should be.
If your EHR cannot support these workflows, you may find staff using workarounds, storing information outside the system, or duplicating efforts across platforms. These inefficiencies add up quickly and can lead to inconsistent care.
How to fix it:
Review how your clinical team currently documents care and where their workflow breaks down. If your EHR allows configuration changes, adjust templates and settings to match behavioral health needs.
If limitations are built into the platform, consider transitioning to an EHR designed specifically for mental health, like ICANotes. This will mean your workflows are supported out of the box without relying on workarounds.
2. Resistance From Staff
Staff often resist using an EHR when training is too broad, support is limited, or the system doesn’t fit their workflow. Even experienced clinicians may become frustrated if the platform slows them down or makes routine tasks harder to complete.
This kind of frustration isn’t just anecdotal. A systematic review of recent research found that poor EHR usability is directly linked to increased clinician stress and burnout. When providers feel overwhelmed by inefficient systems, adoption suffers. Some revert to paper or external tools, leading to inconsistent documentation and added administrative work.
How to fix it:
Build your training plan around the specific responsibilities of each team member. Clinicians, front office staff, and billing teams each need to learn the parts of the system they’ll use most. Focus on hands-on practice that mirrors your actual workflows, and provide quick-reference guides to reinforce key steps.
After go-live, schedule follow-up sessions to address questions and support long-term success. ICANotes offers role-based training tailored to each user group, helping your team feel confident and capable from the start.
3. Integration Failures
Behavioral health practices often coordinate care with primary care providers, labs, referral networks, and billing clearinghouses. When an EHR doesn’t support smooth data exchange, teams fall back on faxing, scanning, or re-entering data manually. This increases the chance of delays, duplication, and communication errors.
How to fix it:
Make a list of all systems your EHR needs to connect with. Confirm whether your EHR supports integration standards like HL7, CCD, SFTP, or secure fax. Ask vendors to demonstrate these connections in action — not just promise them. Test each one before launch to ensure data flows as expected between systems.
4. Data Gaps from Migration
Switching from one EHR to another is rarely seamless. Important clinical data, like medications, diagnoses, or therapy history, can be lost or imported incorrectly. If clinicians cannot trust the system to hold accurate records, they may delay care, duplicate work, or miss critical details.
How to fix it:
Begin by identifying which data needs to be transferred, including active medications, diagnosis lists, and recent notes. Involve your clinical team in reviewing how that information should appear in the new system. Run a test import and validate a sample of records before moving forward.
After go-live, assign someone to monitor charts and address any inconsistencies in historical data. ICANotes supports this process with guided data migration, test imports for validation, and post-migration assistance to help ensure your records are complete, accurate, and ready for clinical use.
5. Inefficient Documentation
In behavioral health, providers often need to document several sessions a day for the same client. In fact, a recent study found that clinicians spend more than a third of their working week just on clinical documentation.
When documentation tools are poorly designed, with too many clicks, irrelevant fields, or hard-to-navigate layouts, clinicians lose valuable time. This can lead to late charting, reduced time with clients, and overall documentation fatigue.
How to fix it:
Improving documentation efficiency starts with using a system designed for the needs of behavioral health providers. ICANotes offers structured templates for progress notes, treatment plans, and assessments that minimize typing and reduce repetitive tasks.
Built-in smart text, auto-coding, and reusable content help clinicians complete notes faster and more consistently. These tools support timely documentation while maintaining the level of detail needed for quality care and compliance.
Related: How to Write Progress Notes
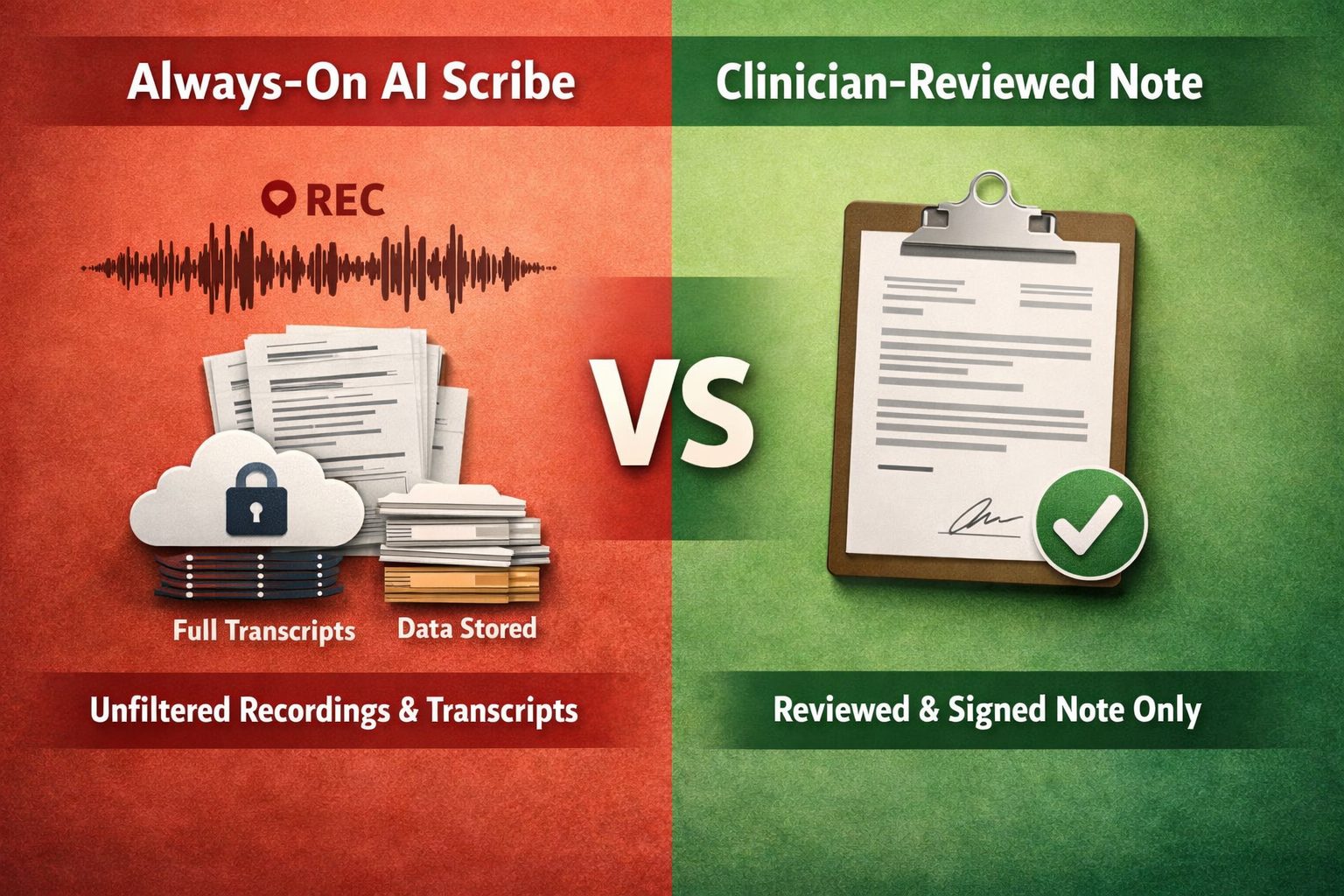
6. Compliance Concerns
Behavioral health data is subject to additional privacy regulations beyond HIPAA, including 42 CFR Part 2. Systems that lack built-in safeguards can expose your practice to legal risks or compromise patient trust.
How to fix it:
Choose an EHR that supports role-based access, audit logs, consent tracking, and data segmentation. Regularly audit permissions and document access settings. Make sure your team is trained on how to handle sensitive information and log disclosures when necessary to stay compliant with HIPAA and 42 CFR Part 2.
7. Rigid or Missing Templates
Generic templates rarely meet the documentation standards required for behavioral health. If templates are too rigid or missing key elements, clinicians must rely on free text, which slows them down and can lead to billing errors or inconsistent records.
How to fix it:
Look for an EHR that includes editable templates for therapy, psychiatry, intake assessments, crisis plans, and DSM-5 coding. Encourage staff to provide input on the layout and structure of templates, and standardize formats across your team to support high-quality documentation and compliance.
Frequently Asked Questions
Get Started with a Better EHR Experience
Choosing the right EHR can make a significant difference in how your practice manages documentation, shares information, and stays compliant. ICANotes is purpose-built for behavioral health, combining structured note templates, secure data exchange, and compliance-ready features in one easy-to-use system.
If you're ready to reduce documentation burden and improve care coordination, explore what ICANotes can do for your team.
Start your free trial, schedule a demo, or contact us for a custom quote at 443-347-0990.
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
- Complete Notes in Minutes - Purpose-built for behavioral health charting
- Always Audit-Ready – Structured documentation that meets payer requirements
- Keep Your Schedule Full – Automated reminders reduce costly no-shows
- Engage Clients Seamlessly – Secure portal for forms, messages, and payments
- HIPAA-Compliant Telehealth built into your workflow
Complete Notes in Minutes – Purpose-built for behavioral health charting
Always Audit-Ready – Structured documentation that meets payer requirements
Keep Your Schedule Full – Automated reminders reduce costly no-shows
Engage Clients Seamlessly – Secure portal for forms, messages, and payments
HIPAA-Compliant Telehealth built into your workflow
Related Posts

Sanjiv Patel
Vice President of Product
Sanjiv Patel is Vice President of Product at ICANotes, where he leads the strategic development of behavioral health EHR and billing solutions. With over 20 years of experience in healthcare technology, Sanjiv has spearheaded major product initiatives that enhance clinical efficiency and provider outcomes. He holds CSM and CSPO certifications and is a graduate of Drexel University.