Blog > Practice Management > Mental Health Practice Management Software: What Vendors Won't Tell You
Mental Health Practice Management Software: What Most Vendors Won't Tell You
Mental health practice management software is designed to streamline scheduling, billing, documentation, and client communication — but many platforms fall short in ways vendors rarely explain upfront. From hidden costs and rigid workflows to compliance gaps and poor fit across care models, the wrong behavioral health practice management software can increase administrative burden instead of reducing it. This guide helps therapists, psychiatrists, and group practices evaluate therapy practice management software and psychiatry practice management software with clarity, exposing what most vendors leave out so you can choose a system that truly supports how behavioral health care is delivered.

Last Updated: January 2, 2026


What You'll Learn
-
What mental health practice management software is actually designed to do — and where its limitations begin
-
The key differences between behavioral health practice management software built for therapy, psychiatry, or mixed practices
-
Why “all-in-one” platforms often fail therapists and psychiatrists in different ways
-
Where hidden costs appear in therapy and psychiatry practice management software, including add-ons, migration, and support tiers
-
How scheduling, billing, telehealth, and client portals quietly break down in real-world behavioral health workflows
-
What meaningful customization looks like — and how to spot cosmetic flexibility vs true workflow support
-
How compliance and security responsibilities are often shifted onto practices despite “HIPAA compliant” claims
-
How to evaluate practice management software using real-world trials instead of relying only on vendor demos
Contents
- What Mental Health Practice Management Software is Really Designed To Do
- Why Therapists and Psychiatrists Need Fundamentally Different Software Features
- The Features Vendors Highlight — and What They Leave Out
- The Hidden Costs of Behavioral Health Practice Management Software
- Compliance and Security: What "HIPAA Compliant" Really Means — and What It Doesn't
- How to Choose the Right Software for Your Mental Health Practice
- Conclusion: Choose Software That Works the Way You Do
- FAQ: Mental Health Practice Management Software
- How ICANotes Supports the Real-World Needs of Mental Health Practices
Mental health practice management software is supposed to make running a practice easier. For many clinicians, it does the opposite.
Platforms promise efficiency, automation, and “all-in-one” simplicity — yet therapists and psychiatrists often find themselves spending more time clicking, correcting, and chasing down billing issues than they did before switching systems.
The problem isn’t that clinicians choose poorly. It’s that vendors rarely explain what their software is actually designed to do — and where its limitations begin.
Therapists already spend an estimated 10–15 hours each month on administrative work instead of patient care. At the same time, demand for mental health services continues to rise, putting pressure on practices to operate more efficiently without sacrificing quality or compliance.
Practice management software can help — but only when it truly fits how behavioral health care is delivered. There’s a significant difference between tools that simply schedule appointments and systems designed to support recurring care, nuanced documentation, and complex billing realities.
This guide breaks down what mental health practice management software is really built to handle, what most vendors leave out of the conversation, and how to evaluate platforms without locking yourself into costly tradeoffs later.
What Mental Health Practice Management Software is Really Designed to Do
Mental health practice management software is often marketed as a tool to “improve care.” In reality, most systems are designed first to standardize and streamline administrative operations — not to enhance clinical decision-making or therapeutic outcomes.
That distinction matters more than vendors usually acknowledge.
At its core, practice management software is built to help practices:
-
Schedule appointments
-
Manage calendars and provider availability
-
Handle billing and claims
-
Track payments and basic reporting
These tools can absolutely reduce paperwork and administrative friction — when they align with how a practice actually operates. But improved administration does not automatically translate into improved care.
Most platforms optimize for efficiency at scale: standard workflows, repeatable processes, and generalized healthcare assumptions. Behavioral health care, however, is not standardized in the same way as most medical services.
That design gap explains why software can feel polished in demos yet frustrating in daily use.
EHR vs. Practice Management Software: Why the Difference Matters
One reason confusion persists is that vendors often blur the line between mental health EHR software and practice management software, even though they serve different purposes.
-
Practice management software focuses on operations — scheduling, billing, client communication, and revenue tracking.
-
Electronic Health Record (EHR) systems manage clinical documentation — assessments, treatment plans, progress notes, and health records.
Many modern platforms combine both into a single system, which can be helpful — but only if each component is designed with behavioral health in mind. When either side is underdeveloped, practices feel the strain quickly: documentation becomes rigid, billing becomes disconnected, or workflows fragment.
The issue isn’t integration itself — it’s what the integration prioritizes.
Designed for Healthcare in General — Not Behavioral Health Specifically
Most practice management systems are built around general medical workflows:
-
Short, episodic visits
-
Limited narrative documentation
-
Infrequent follow-ups
-
Highly standardized coding
Behavioral health operates differently. Therapy and psychiatry rely on:
-
Ongoing, recurring care
-
Longitudinal documentation
-
Nuanced clinical narratives
-
Complex payer and compliance requirements
When software is designed for the business of healthcare rather than the practice of behavioral health, clinicians are left adapting their work to fit the system — instead of the system supporting their work.
The Downstream Effects of This Design Bias
This administrative-first design approach helps explain why so many practices later encounter problems with:
-
Scheduling and billing workflows that don’t stay connected
-
Telehealth tools that feel bolted on

- Client portals that frustrate rather than engage
-
“Customization” that doesn’t meaningfully change workflows
-
Compliance responsibilities that quietly shift onto clinicians
These aren’t isolated feature gaps — they’re predictable outcomes of how the software was designed from the start.
Understanding what mental health practice management software is actually built to do makes it easier to spot where vendor promises end — and where operational tradeoffs begin.
Evaluate Practice Management Software Before You Commit: Don't Rely on Demos Alone
Choosing mental health practice management software shouldn’t require guesswork. This vendor-neutral evaluation checklist helps you identify workflow gaps, hidden costs, and long-term risks before you sign a contract.
Use it during demos and free trials to assess scheduling, billing, telehealth, client portals, customization, compliance, and total cost of ownership — all in one place.
Why Therapists and Psychiatrists Need Fundamentally Different Software Features
Although therapists and psychiatrists both deliver behavioral health care, their clinical responsibilities, documentation requirements, and regulatory exposure are not the same — and their software should reflect that reality. Many vendors gloss over these differences, marketing a single platform as “ideal for all behavioral health providers,” when in practice, that approach creates friction, inefficiency, and risk.
Psychiatrists: Medication-Driven, High-Risk, Compliance-Heavy Workflows
Psychiatrists manage complex medical decision-making that extends well beyond session notes. Their software must support:
-
Medication management and e-prescribing, including controlled substances
-
Medication history tracking, dose changes, and adverse effect monitoring
-
Clinical decision support related to diagnoses, labs, and comorbid conditions
-
Stronger audit trails and documentation defensibility due to higher liability exposure
Generic documentation tools often fall short here. If medication workflows feel bolted on rather than core to the system, psychiatrists end up relying on workarounds, separate tools, or manual tracking — all of which increase risk and administrative burden.
Therapists: Narrative-Driven, Session-Based, Outcome-Focused Care
Therapists, on the other hand, rely heavily on qualitative documentation and therapeutic continuity. Their software needs to support:
-
Flexible, narrative progress notes aligned with modalities like CBT, ACT, EMDR, or psychodynamic therapy
-
Customizable templates that reflect how therapy actually unfolds, not rigid medical models
-
Outcome measurement tools (e.g., PHQ-9, GAD-7) that integrate naturally into sessions
-
Recurring appointment scheduling and long-term treatment planning
When therapy documentation is forced into overly medicalized or inflexible formats, clinicians spend more time translating their work into the system than focusing on the client.
| Workflow Area | Therapists (Counseling / Psychotherapy) | Psychiatrists (Medication Management) |
|---|---|---|
| Core documentation | Flexible narrative notes aligned to modality (CBT, ACT, EMDR, etc.) | Structured clinical decision-making + defensible med-management documentation |
| Key “must-have” tools | Customizable templates, treatment plan continuity, outcomes measures | Medication list management, prescribing workflows, audit-ready history |
| Scheduling reality | High volume of recurring weekly/biweekly sessions | Shorter, periodic follow-ups (often with higher risk/comorbidity complexity) |
| Risk & compliance pressure | Documentation sensitivity + client access/readability considerations | Higher liability exposure + stricter controls around meds and clinical rationale |
Where “All-in-One” Platforms Often Fail
The problem isn’t that vendors try to serve both audiences — it’s that many systems optimize for neither. Instead, they offer shallow versions of critical features:
-
Medication tools that lack depth for psychiatry
-
Templates that are too rigid for therapy
-
Billing workflows that don’t reflect behavioral health complexity
-
Scheduling models designed for episodic medical visits, not weekly therapy
Physical healthcare software assumes infrequent visits and short encounters. Behavioral health is different. Therapy and psychiatry involve ongoing relationships, frequent sessions, evolving treatment goals, and heightened documentation sensitivity. Software that doesn’t account for this reality quietly creates inefficiency and burnout.
Many practices end up stitching together multiple tools because their “all-in-one” system doesn’t fully support both therapy and psychiatry workflows. Purpose-built platforms (like ICANotes) are designed around behavioral health realities — recurring sessions, modality-driven documentation, outcomes tracking, and (when needed) robust psychiatric workflows — so practices aren’t forced into workarounds just to get through a normal day. The result is a smoother admin experience and documentation that better reflects the actual care being delivered.
The Takeaway for Practice Owners
Before committing to a platform, practices should ask a simple but critical question:
Was this software truly designed for how we practice — or are we expected to adapt our care to fit the system?
Therapists and psychiatrists don’t just prefer different features — they require them to work efficiently, document defensibly, and deliver quality care. Any vendor that treats those differences as minor is overselling simplicity and underserving clinicians.
The Features Vendors Highlight — and What They Leave Out
Mental health software vendors showcase impressive features in their marketing materials. They conveniently skip critical limitations that you'll only discover after implementation. These gaps in functionality can help you make better decisions when selecting a platform for your practice.
Scheduling and Billing: What Works and Where Systems Quietly Break Down
Scheduling and billing are often the first features vendors showcase — and for good reason. Most mental health practice management systems handle basic appointment booking reasonably well. But once you move beyond surface-level scheduling, cracks begin to show, especially in billing workflows designed more for medical offices than behavioral health practices.
What usually works well
Most platforms can reliably:
-
Schedule single and recurring appointments
-
Send automated reminders via email or text
-
Handle basic provider availability and room assignments
For solo providers or small practices with straightforward schedules, these features may feel “good enough” at first. The problems tend to surface as volume increases, clinicians specialize, or payers enter the picture.
Where scheduling starts to fray
Behavioral health scheduling isn’t episodic — it’s relationship-based and ongoing. Weekly or biweekly sessions, frequent reschedules, and long-term treatment plans are the norm. Many systems struggle with:
-
Managing recurring appointments without manual cleanup
-
Handling provider substitutions or coverage changes cleanly
-
Tracking cancellations, no-shows, and attendance patterns over time
-
Supporting different session lengths and documentation requirements in the same day
When scheduling tools aren’t built for this reality, staff end up maintaining parallel systems or relying on manual fixes that quietly erode efficiency.
Where billing breaks — and revenue leaks begin
Billing is where the real damage happens.
Vendors often claim their software “handles billing,” but in practice, many platforms fall short of what true behavioral health billing software needs to support. Common breakdowns include systems that:
-
Separate clinical documentation from billing workflows
-
Require duplicate data entry between notes and claims
-
Lack behavioral health–specific coding logic
-
Fail to flag missing or non-billable documentation in real time
In these systems, a completed session does not automatically become a clean, billable claim. Claims get delayed, rejected, or never submitted at all. Once filing deadlines pass, that revenue is permanently lost — often without the practice realizing it until months later.
Behavioral health–specific platforms like ICANotes are designed to reduce this risk by tightly linking clinical documentation and billing, so sessions move from note completion to claim submission without manual reconciliation or guesswork.
The hidden cost of disconnected workflows
When scheduling, documentation, and billing don’t work as a single system:
-
Sessions fall through the cracks
-
Staff spend hours reconciling encounters with claims
-
Clinicians are pulled into administrative follow-ups
-
Practices lose revenue without clear visibility into why
These aren’t edge cases — they’re common failure points that vendors rarely demonstrate during sales demos.
Some behavioral health–specific platforms, such as ICANotes, are intentionally designed to close these gaps by linking scheduling, clinical documentation, and billing into a single, continuous workflow — so completed sessions don’t stall, disappear, or require manual reconciliation just to get paid.
What practices should demand instead
A behavioral health-ready system should:
-
Tie each scheduled session directly to documentation and billing
-
Generate claims automatically once notes are completed
-
Reflect behavioral health coding and payer rules
-
Provide clear visibility into what has been billed, rejected, or missed
If scheduling and billing feel like separate worlds inside your software, that’s not a workflow issue — it’s a design flaw.
Telehealth: What Vendors Promise — and What Practices Actually Experience
Telehealth is often marketed as a built-in convenience: secure, seamless, and fully integrated. In reality, many mental health practices discover that telehealth for mental health practices is one of the most fragmented parts of their software experience.
The promise: “fully integrated telehealth”
Most vendors advertise telehealth as:
-
Included with scheduling
-
Secure and HIPAA compliant
-
Easy for both clinicians and clients
-
Fully connected to notes and billing
On paper, this sounds ideal. In practice, the details matter — and that’s where many systems fall short.
The reality: add-ons, friction, and extra costs
Many platforms treat telehealth as a paid add-on, not a core feature. Practices often encounter:
-
Additional per-provider or per-session fees
-
Usage limits that trigger surprise charges
-
Separate login experiences for clients
-
Video tools that don’t fully sync with scheduling or documentation
This forces clinicians and staff to juggle multiple systems just to complete a single encounter — scheduling in one place, meeting in another, and documenting elsewhere.
Client experience is where problems surface first
Even when telehealth technically “works,” usability issues can quietly undermine care:
-
Complicated client onboarding and account setup
-
Poor mobile performance or browser compatibility
-
Unclear instructions for joining sessions
-
Limited support when something goes wrong mid-session
These issues don’t always show up during vendor demos, but they surface quickly in real-world use — and they directly impact attendance, engagement, and continuity of care.
Security claims vs. practical data control
Vendors frequently emphasize encryption and HIPAA compliance, but those claims don’t always address:
-
How telehealth session data is stored or retained
-
Whether metadata or usage data is shared with third parties
-
What happens to telehealth data after contract termination
In some widely reported cases across the digital mental health space, sensitive behavioral health information has been shared in ways users never expected — a reminder that “secure” doesn’t always mean “transparent.”
The hidden workflow cost
When telehealth isn’t truly integrated:
-
Sessions may not automatically link to notes
-
Documentation can lag behind care delivery
-
Billing workflows become manual or delayed
-
Clinicians spend time troubleshooting instead of treating
Telehealth should simplify care delivery — not introduce another layer of administrative work.
What to look for instead
A behavioral health-ready telehealth solution should:
-
Be included as part of the core platform, not gated behind add-ons
-
Link sessions directly to documentation and billing
-
Offer a simple, client-friendly experience
-
Provide clear answers about data handling and retention
If telehealth feels bolted on rather than built in, that’s a signal worth paying attention to.
Some behavioral health–specific platforms, including ICANotes, approach telehealth as an extension of the clinical workflow — not a separate tool — helping practices avoid the fragmentation that often appears once virtual sessions become a routine part of care delivery.
Client Portals: Secure in Theory, Frustrating in Practice
Client portals are often presented as a win for everyone — secure messaging, easy scheduling, digital intake, and access to records. In reality, the quality of a portal can either reduce administrative work or quietly create more of it.
Why portals matter more than vendors admit
The mental health client portal is often the primary point of interaction outside the session. It directly affects:
-
Intake completion and first-session readiness
-
Appointment confirmations and no-show rates
-
Payment collection and billing transparency
-
Secure communication between visits
When portals work well, they reduce staff workload. When they don’t, practices revert to email, phone calls, and manual follow-ups — undermining the very efficiencies the software promised.
The open notes reality
With widespread adoption of Open Notes, clients increasingly have access to their clinical documentation. This makes portal design and functionality especially important in mental health settings.
Portals influence:
-
How easily clients can view notes and summaries
-
How clinicians balance transparency with therapeutic sensitivity
-
How misunderstandings are identified and addressed
-
Whether disputes escalate into formal complaints
Vendors rarely discuss how their portals support clinicians in navigating this reality — or how much extra time poorly designed portals can create.
Where client portals commonly fall short
Despite strong marketing claims, many portals struggle with:
-
Complicated account setup that discourages client adoption
-
Limited mobile usability or inconsistent browser performance
-
Rigid workflows that don’t match behavioral health intake needs
-
Messaging tools that feel more like email than secure clinical communication
When adoption is low, it’s often blamed on clients — but the real issue is usually portal design.
| Portal Area | A Portal That Helps Your Practice | A Portal That Creates Hidden Work |
|---|---|---|
| Getting started | Simple invite + login; easy password reset; works on mobile | Confusing setup; failed invites; inconsistent mobile experience |
| Intake & forms | Behavioral health–friendly intake, consents, and questionnaires that flow into the chart | Rigid forms, add-on fees, or manual re-entry into clinical documentation |
| Scheduling | Clear reschedule/cancel rules; supports recurring care and provider availability | Inflexible scheduling; recurring care becomes manual cleanup |
| Payments & statements | Clients can view balances, pay easily, and access statements/superbills | Limited payment options; confusing invoices; more billing calls |
| Messaging | Organized, secure threads with clear routing/triage and chart linkage | Message chaos; poor triage; staff need broad access to respond |
| Transparency controls | Clear visibility settings by document type; easy amendment workflows | Unclear what clients see and when; higher misunderstanding risk |
The hidden cost of low portal adoption
A portal that clients avoid doesn’t just sit unused. It creates downstream consequences:
-
Incomplete or rushed intake information
-
Increased administrative follow-up
-
More missed appointments
-
Delayed payments and billing questions
-
Added documentation stress for clinicians
Over time, these inefficiencies compound, contributing to staff burnout and reduced practice scalability.
What practices should look for instead
A behavioral health–ready client portal should:
-
Be intuitive for clients of varying tech comfort levels
-
Support behavioral health–specific intake and consent workflows
-
Facilitate secure, organized communication
-
Integrate seamlessly with scheduling, documentation, and billing
If a portal feels like an afterthought, it will become one in daily use — with real operational consequences.
Some behavioral health–focused platforms, including ICANotes, treat the client portal as a core part of the care experience — designed to support intake, documentation transparency, and communication without adding friction for clinicians or staff.
Customization: Marketed as Flexible, Delivered as Rigid
Customization is one of the most overused — and misunderstood — selling points in mental health practice management software. Vendors frequently advertise “highly customizable” systems, but in practice, customization often means little more than choosing from a limited set of predefined templates.
For behavioral health practices, that gap matters.
Cosmetic customization vs. real workflow flexibility
Many platforms allow superficial changes:
-
Renaming fields
-
Hiding unused sections
-
Selecting from preset note formats
What they don’t allow is meaningful control over how work actually flows:
-
How notes are structured by modality or provider type
-
How documentation ties to billing logic
-
How assessments, treatment plans, and progress notes connect over time
-
How different payers or programs require different documentation standards
When customization stops at the surface level, clinicians are forced to adapt their practice to the software — not the other way around.
Why behavioral health needs deeper customization
The hidden cost of limited customization
When software can’t adapt to real-world workflows:
-
Notes take longer to complete
-
Documentation quality becomes inconsistent
-
Billing errors and denials increase
-
Audits become harder to defend
-
Clinician frustration and burnout rise
These costs accumulate quietly. Vendors rarely frame limited customization as a risk — but practices feel it daily.
What meaningful customization actually looks like
A behavioral health–ready platform should allow practices to:
-
Customize documentation by role (therapist vs psychiatrist)
-
Align templates with therapeutic modalities
-
Integrate assessments naturally into clinical notes
-
Support payer- and program-specific documentation needs
-
Maintain consistency without forcing rigidity
If “customization” only changes how a form looks — not how work gets done — it’s not customization. It’s decoration.
Behavioral health–focused platforms like ICANotes are designed with clinical flexibility in mind, allowing practices to adapt documentation and workflows to their modalities, provider roles, and payer requirements — without forcing clinicians into rigid, one-size-fits-all templates.
The Hidden Costs of Behavioral Health Practice Management Software
The biggest risk with behavioral health practice management software isn’t the subscription price — it’s everything that comes after you’ve signed the contract.
Vendors often present pricing as predictable and straightforward. In reality, many costs are delayed, fragmented, or framed as optional — even when they’re essential to running your practice day to day.
1. Implementation Isn’t “Included” — It’s Inevitable
Even cloud-based systems require meaningful setup. Practices routinely encounter:
-
One-time onboarding or implementation fees
-
Workflow configuration costs
-
Limited “free” training followed by paid advanced support
These expenses surface once a practice commits — when switching feels harder. For growing or multi-provider practices, implementation costs can rival several months (or more) of subscription fees.
2. Data Migration Costs More Than Vendors Admit
Moving from an existing EHR or paper system is rarely simple. Behavioral health data is complex, longitudinal, and often unstructured.
Common hidden migration costs include:
-
Charges based on record volume, not just number of clients
-
Partial migrations that exclude notes, attachments, or historical data
-
Manual cleanup to correct formatting, duplicates, or missing fields
When migration isn’t handled well, practices pay twice: once in fees, and again in staff time spent fixing problems after go-live.
3. Feature Gating Turns “Nice to Have” Into “Pay to Operate”
Many platforms advertise attractive base pricing — then gate core functionality behind add-ons.
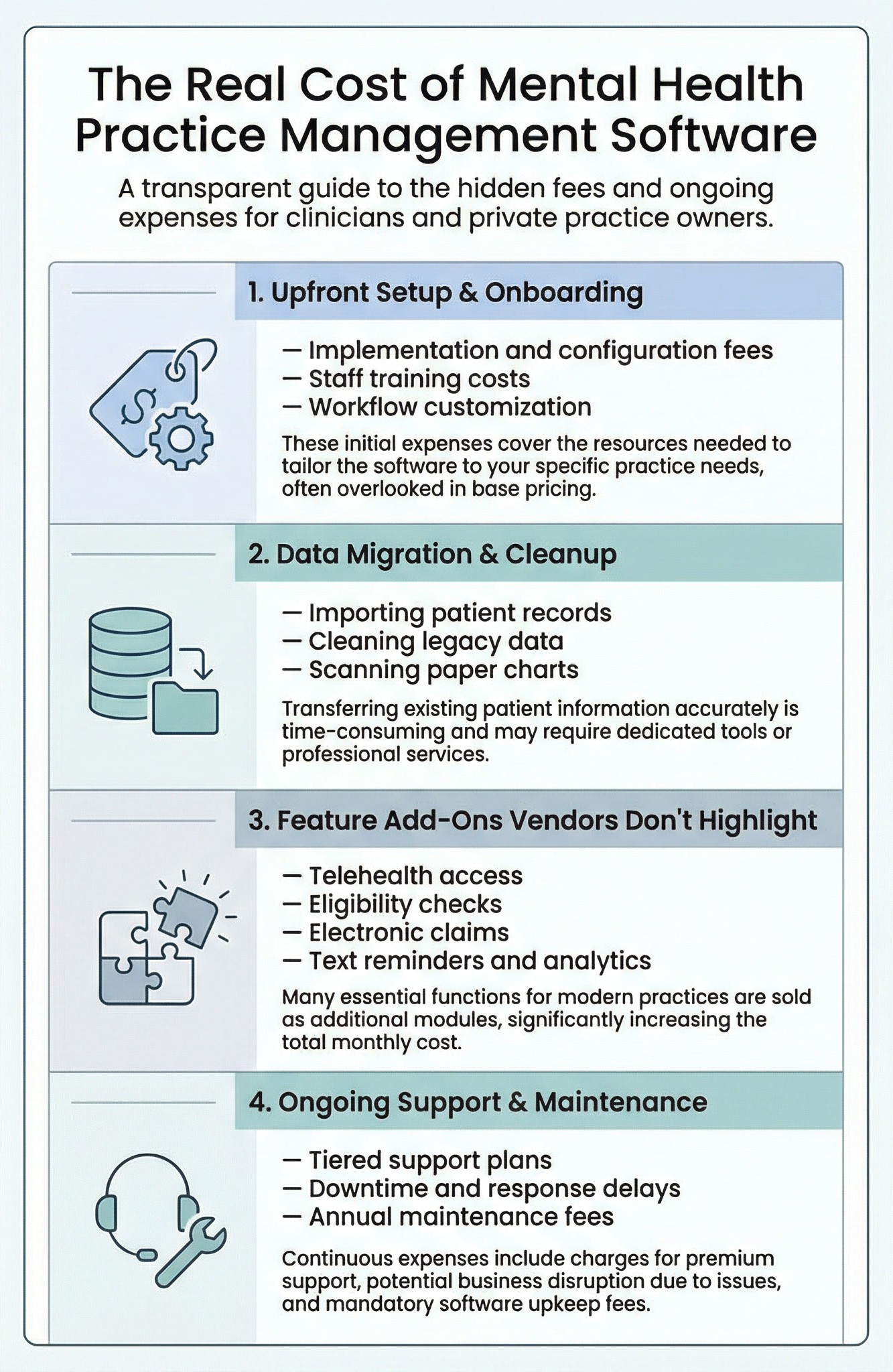
- Eligibility checks beyond minimal usage
-
Electronic claim submission
-
Reporting, analytics, or outcome tracking
What looks affordable at first can become unpredictable as usage grows. Over time, practices lose clarity on what they’re actually paying for — and why.
4. Support Tiers Determine How Much Downtime You Can Afford
Not all support is equal. Lower-priced plans often come with:
-
Slower response times
-
Limited live support
-
Self-service expectations during system issues
For a behavioral health practice, downtime doesn’t just delay work — it delays care and revenue. Many vendors quietly monetize reliability through premium support tiers.
The Cost Vendors Rarely Acknowledge: Lost Time
Beyond invoices and fees is the most expensive cost of all:
-
Clinicians spending more time documenting than treating
-
Staff reconciling data across systems
-
Missed or delayed claims
-
Burnout driven by inefficient workflows
These costs don’t show up on a pricing page, but they compound over time.
What Vendors Won’t Tell You Up Front
Most hidden costs aren’t accidental — they’re structural. Pricing models are designed to look simple at the start and expand quietly as practices rely more deeply on the system.
That doesn’t make vendors dishonest — but it does make transparency rare.
What Practices Should Do Instead
Rather than asking, “What does it cost per month?” practices should ask:
-
What will this cost us to implement, use fully, and grow with?
-
Which features are essential — and which cost extra?
-
What happens when something breaks?
A system that appears cheaper upfront can quickly become more expensive — financially and operationally — if hidden costs aren’t uncovered early. Behavioral health–specific platforms like ICANotes tend to be more transparent about total cost because they’re built to support core clinical and administrative workflows from day one.
- Low monthly subscription price
- “All-in-one” feature lists
- Free trials or demos
- Basic onboarding included
- HIPAA compliance claims
- Implementation and workflow configuration
- Data migration and cleanup
- Telehealth, billing, and reporting add-ons
- Premium support tiers
- Staff time spent managing inefficiencies
- Revenue lost to delays, denials, or missed claims
Compliance and Security: What “HIPAA Compliant” Really Means — and What It Doesn’t
Most behavioral health practice management vendors prominently advertise that their platforms are “HIPAA compliant.” While that claim sounds reassuring, it often masks a more complicated reality. HIPAA compliance for mental health practices is an ongoing, shared responsibility that extends beyond encryption and cloud hosting — and much of the risk ultimately sits with the practice, not the software vendor.
Compliance Is More Than Encryption
Vendors frequently highlight technical safeguards such as:
-
Encrypted data storage
-
Secure servers
-
Password protection
These measures are necessary — but they are not sufficient.
True compliance also depends on:
-
Role-based access controls
-
Audit logs and activity tracking
-
Clear data retention and deletion policies
-
Staff training and internal procedures
Many platforms provide the technology but leave the operational burden entirely on the practice.
The Compliance Illusion
Phrases like “HIPAA compliant” and “bank-level security” are often used as shorthand for safety. In reality, they usually indicate that a system meets baseline technical requirements, not that it supports compliance in real-world clinical workflows.
Vendors rarely volunteer answers to questions such as:
-
Who beyond your practice can access patient data?
-
How is access logged and reviewed?
-
What happens to your data after contract termination?
-
How quickly are breaches disclosed — and who bears responsibility?
These gaps don’t show up during demos, but they matter during audits, disputes, or incidents.
| What You’ll Hear in a Demo | What You Should Verify | Why It Matters in Practice |
|---|---|---|
| “We’re HIPAA compliant.” | Clear shared-responsibility breakdown + BAA scope and exclusions | Compliance risk often stays with the practice, even when the vendor says “compliant.” |
| “Your data is encrypted.” | Granular access controls, export restrictions, and auditability | Encryption doesn’t prevent inappropriate access or accidental disclosure. |
| “We have a BAA.” | Data ownership, retention, offboarding/export process, and fees | A BAA sets minimum obligations but may not protect you the way you assume. |
| “We have role-based permissions.” | True role-based controls (not all-or-nothing), by feature and by document type | Behavioral health teams need nuanced access to avoid overexposure of PHI. |
| “We have audit logs.” | Searchable, exportable logs + note version history (edits vs amendments) | Audit defensibility depends on proving who accessed or changed what, and when. |
| “We take security seriously.” | Breach response plan, notification timelines, third-party audits (e.g., SOC 2 summary) | When something goes wrong, your ability to respond quickly limits damage and liability. |
BAAs: Necessary, but Limited Protection
Business Associate Agreements (BAAs) are essential — but they are not a safety net.
Most BAAs:
-
Define minimum handling requirements for protected health information
-
Limit vendor liability in the event of a breach
-
Allow use of de-identified data for internal purposes
-
Exclude responsibility for practice-level errors or misconfigurations
In other words, a BAA helps establish legal boundaries — it does not eliminate risk. Practices remain responsible for how data is accessed, documented, shared, and secured.
Behavioral Health Has Higher Stakes
Mental health data carries additional sensitivity:
-
Detailed narrative notes
-
Substance use and trauma histories
-
Psychiatric diagnoses and medications
-
Increased client access through Open Notes
Software that doesn’t support granular access controls, clear documentation boundaries, and transparent data handling creates more than compliance risk — it creates clinical anxiety.
When clinicians aren’t confident in how information is stored or shared, documentation becomes more defensive, time-consuming, and stressful.
What Practices Should Look For Instead
A security-conscious behavioral health platform should:
-
Make access and permissions easy to understand and control
-
Provide clear audit trails for clinical and administrative activity
-
Be transparent about data use, retention, and exit processes
-
Support compliance as part of daily workflow — not just as legal language
If compliance feels like something you’re expected to “figure out later,” the software is shifting risk onto your practice.
Behavioral health–specific platforms like ICANotes tend to be more workflow-aware about compliance — pairing strong security controls with practical features (permissions, audit trails, documentation workflows) that help practices stay defensible without turning clinicians into compliance officers.
How to Choose the Right Software for Your Mental Health Practice
After reviewing what vendors rarely disclose, the goal isn’t to find “perfect” software — it’s to find a system that supports how you actually practice without creating hidden work, risk, or cost over time.
Start With Fit, Not Features
Before comparing platforms, get clear on how your practice operates:
-
Solo or group?
-
Therapy, psychiatry, or both?
-
High-frequency recurring sessions or episodic care?
-
Private pay, insurance, or mixed?
Software that looks impressive on a feature list can still be a poor fit if it forces you to change established workflows.
Demand Transparency Up Front
Given the hidden costs and compliance gaps common in this market, transparency matters as much as functionality. During evaluations, look for vendors who can clearly explain:
-
Total cost of ownership (not just monthly pricing)
-
Which features are included vs. add-ons
-
How data is handled, retained, and exported
-
Where compliance responsibility sits
If answers feel vague or deferred, assume the burden will land on your practice later.
Use Trial Periods to Eliminate, Not Explore
Free trials aren’t about learning the software — they’re about finding reasons not to choose it.
During a trial, simulate real work:
-
Schedule and reschedule recurring sessions
-
Complete documentation and follow it through billing
-
Use telehealth and the client portal as a client would
-
Test permissions, audit logs, and reporting
If workflows break under normal use, they won’t improve after implementation.
Prioritize Workflow Integration Over Customization Claims
Many platforms advertise customization, but what matters is integration:
-
Do scheduling, notes, billing, and telehealth function as one system?
-
Do completed sessions reliably become billable claims?
-
Can staff and clinicians work without duplicating effort?
Smooth integration reduces burnout and protects revenue — even if the interface looks less flashy.
Choose the System That Reduces Cognitive Load
The right software should:
-
Make documentation easier, not more defensive
-
Reduce administrative follow-ups
-
Support compliance without constant vigilance
-
Free clinicians to focus on care, not clicks
If a system requires constant workarounds, it’s not saving time — it’s shifting labor.
Behavioral health–specific platforms like ICANotes tend to stand out during real-world trials because they’re designed around recurring care, documentation defensibility, and integrated billing — not just surface-level features.
Conclusion: Choose Software That Works the Way You Do
Mental health practice management software is often sold as a simple operational upgrade. In reality, it’s a long-term infrastructure decision that shapes how you document care, manage risk, interact with clients, and sustain your practice.
Vendors aren’t necessarily misleading — but they are selective about what they emphasize. Feature lists highlight convenience. Pricing pages spotlight monthly fees. Demos show best-case scenarios. What’s rarely discussed are the cumulative effects of rigid workflows, gated features, unclear compliance boundaries, and hidden operational costs.
The practices that struggle most with software aren’t those that “chose wrong” — they’re the ones that were never given the full picture.
The key takeaway is that the right system should adapt to your clinical reality, not force you to adapt your care to the software.
Before committing, look beyond surface features by:
- Testing how real sessions move from scheduling to documentation to billing
- Asking uncomfortable questions about cost, data control, and compliance
- Paying attention to where workarounds appear — they rarely disappear later
Purpose-built behavioral health platforms, such as ICANotes, tend to stand out during this process not because they promise everything, but because they’re designed around how mental health practices actually operate — recurring care, documentation defensibility, and integrated workflows that reduce friction over time.
The true value of mental health practice management software isn’t measured in features or flashy dashboards. It’s measured in time reclaimed, risk reduced, and energy redirected back to patient care.
Choose accordingly.
Frequently Asked Questions: Mental Health Practice Management Software
How ICANotes Supports the Real-World Needs of Mental Health Practices
After evaluating what most practice management platforms promise — and where many fall short — it’s clear that mental health practices need software built around recurring care, defensible documentation, and integrated workflows, not generalized healthcare assumptions.
ICANotes was designed specifically for behavioral health, supporting the day-to-day realities of therapy and psychiatry without forcing clinicians to adapt their care to rigid systems.
ICANotes brings together scheduling, documentation, billing, client engagement, and compliance support into a single workflow — reducing duplicate work, missed claims, and administrative friction as practices grow.
Practical Telehealth and Client Engagement Without Tiered Barriers
Telehealth is available as an optional add-on at any subscription plan level, giving practices the flexibility to offer virtual care without upgrading to higher tiers. Client engagement tools, including scheduling support and a client portal, are integrated into the broader workflow so communication, documentation, and billing stay connected rather than fragmented.
Real Support — Without Extra Fees
Selecting software is only half the challenge. ICANotes includes 24×7 support and virtual training at no additional cost, so practices aren’t forced into premium tiers just to get help when questions arise or workflows need adjustment.
In addition, ICANotes offers free monthly educational webinars focused on compliance, documentation best practices, and evolving treatment considerations — helping clinicians stay informed long after implementation.
A Low-Risk Way to Evaluate Fit
Because many limitations don’t surface until real workflows are tested, ICANotes offers a 30-day free trial with no credit card required. Practices can schedule sessions, complete notes, use telehealth, and evaluate client engagement tools before making a commitment.
Ready to See if ICANotes is the Right Fit?
Taken together, ICANotes reflects a practice-centered philosophy: transparent evaluation, integrated workflows, accessible support, and continued education — all aligned with how behavioral health care is actually delivered.
For most mental health practices, that combination matters more than flashy features or aggressive pricing — because the true value of practice management software is measured over time, in reduced friction, clearer billing outcomes, and sustained clinical focus.
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
- Complete Notes in Minutes - Purpose-built for behavioral health charting
- Always Audit-Ready – Structured documentation that meets payer requirements
- Keep Your Schedule Full – Automated reminders reduce costly no-shows
- Engage Clients Seamlessly – Secure portal for forms, messages, and payments
- HIPAA-Compliant Telehealth built into your workflow
Complete Notes in Minutes – Purpose-built for behavioral health charting
Always Audit-Ready – Structured documentation that meets payer requirements
Keep Your Schedule Full – Automated reminders reduce costly no-shows
Engage Clients Seamlessly – Secure portal for forms, messages, and payments
HIPAA-Compliant Telehealth built into your workflow
Related Posts

Sandy Crowley
Chief Marketing Officer
About the Author
Sandy Crowley is the Chief Marketing Officer at ICANotes, a leading EHR platform purpose-built for behavioral health. Sandy has over two decades of experience bridging healthcare, marketing, and software innovation. Formerly the company’s CEO, she guided ICANotes through a period of rapid growth and product expansion. With a background in communications from Stanford University and a passion for helping clinicians streamline documentation and improve outcomes, Sandy continues to drive ICANotes’ mission to make behavioral health software smarter, more efficient, and clinician-focused.