Blog > Treatment Strategies > Mental Health Safety Plan: A Critical Clinical Intervention in 2025
Mental Health Safety Planning: Why It’s No Longer Optional for Clinicians
A mental health safety plan is more than documentation, it’s an evidence-based clinical intervention that reduces suicidal behavior and strengthens therapeutic alliance. This guide explains what a safety plan is, why the Stanley-Brown Safety Planning Intervention is considered the gold standard, and how clinicians can integrate structured safety planning into everyday practice. Learn the essential steps, documentation best practices, and how tools like ICANotes streamline safety-focused workflows.
Last Updated: December 8, 2025


What You'll Learn
- What a mental health safety plan is and why it is essential for suicide prevention.
- How the Stanley-Brown Safety Planning Intervention (SPI) is structured and why it is evidence-based.
- The clinical and documentation benefits of implementing written safety plans over verbal agreements.
- How safety planning strengthens the therapeutic alliance and improves crisis-time decision-making.
- Key research findings demonstrating the effectiveness of safety planning interventions.
- How to incorporate structured safety plans, especially the Stanley-Brown model, into ICANotes workflows.
- Best-practice language for documenting safety planning in clinical notes.
Contents
- The Stanley-Brown Safety Planning Intervention
- What the Research Shows About Safety Planning
- Why Safety Planning is Clinical Work, Not Paperwork
- Why the Stanley-Brown Model Stands Out
- Bringing the Stanley-Brown Safety Plan Into Everyday Workflow
- Making Safety Planning a Standard of Care
- FAQs: Mental Health Safety Plans
In 2022, an estimated 49,476 people died by suicide in the United States and self-harm was the primary reason for over 600,000 emergency room visits in a single year. [1].
Each of these deaths is preventable. Together we can save lives through more efficient workflows and safety planning. Safety planning saves lives and helps prevent suicide events. Safety planning is a clinical intervention, an intervention that is now more accessible through your electronic health record.
Behind each of these deaths are family, friends, and community members — making each loss all the more tragic. We know that many of the individuals we care for think about suicide. In fact, about 20% of high school students seriously consider suicide each year [2], and some of those individuals will try to die by suicide.
Behind every one of those numbers is a patient you have sat with. The one who says “I’m fine” with flat affect. The one who shrugs when you ask about tomorrow. The one who has a plan, access to means, and a very small window where your intervention actually matters.
In that window, what you put on paper matters.
This is where safety planning stops being a checkbox and becomes a core treatment intervention.
What is a Mental Health Safety Plan?
A mental health safety plan is a brief, personalized, and collaborative document that outlines exactly what a client will do when suicidal thoughts or self-harm urges intensify. Unlike outdated verbal “no-harm contracts,” a safety plan provides concrete, step-by-step strategies that help clients recognize their unique warning signs, use internal coping skills, reach out to supportive people, access professional and crisis resources, and reduce access to lethal means. A well-constructed safety plan becomes a lifeline during moments of acute distress — offering structure when executive functioning is compromised and decision-making is impaired. It is both a therapeutic tool and an evidence-based intervention that has been shown to reduce suicidal behavior and increase engagement in treatment.
Why Written Safety Plans Are More Effective Than Verbal No-Harm Contracts
Many of us were trained in an era of “no-suicide contracts.” We asked patients to promise they would not harm themselves and documented that they agreed.
The evidence has not been kind to that practice.
No-suicide contracts do not reliably reduce suicidal behavior, and they do little to teach a patient how to survive the next wave of suicidal intensity. They also do not demonstrate that you have given your patient a usable, skills-based tool when risk is high [3].
A collaborative, written safety plan is different.
Safety planning interventions teach patients to:
- Notice escalating warning signs
- Use internal coping strategies first
- Reach out to safe people and places
- Access professional and crisis resources
- Reduce access to lethal means
- Anchor themselves in reasons to live
In other words, a safety plan is not “don’t do it.” It is “here is exactly what you will do when the urge spikes.”
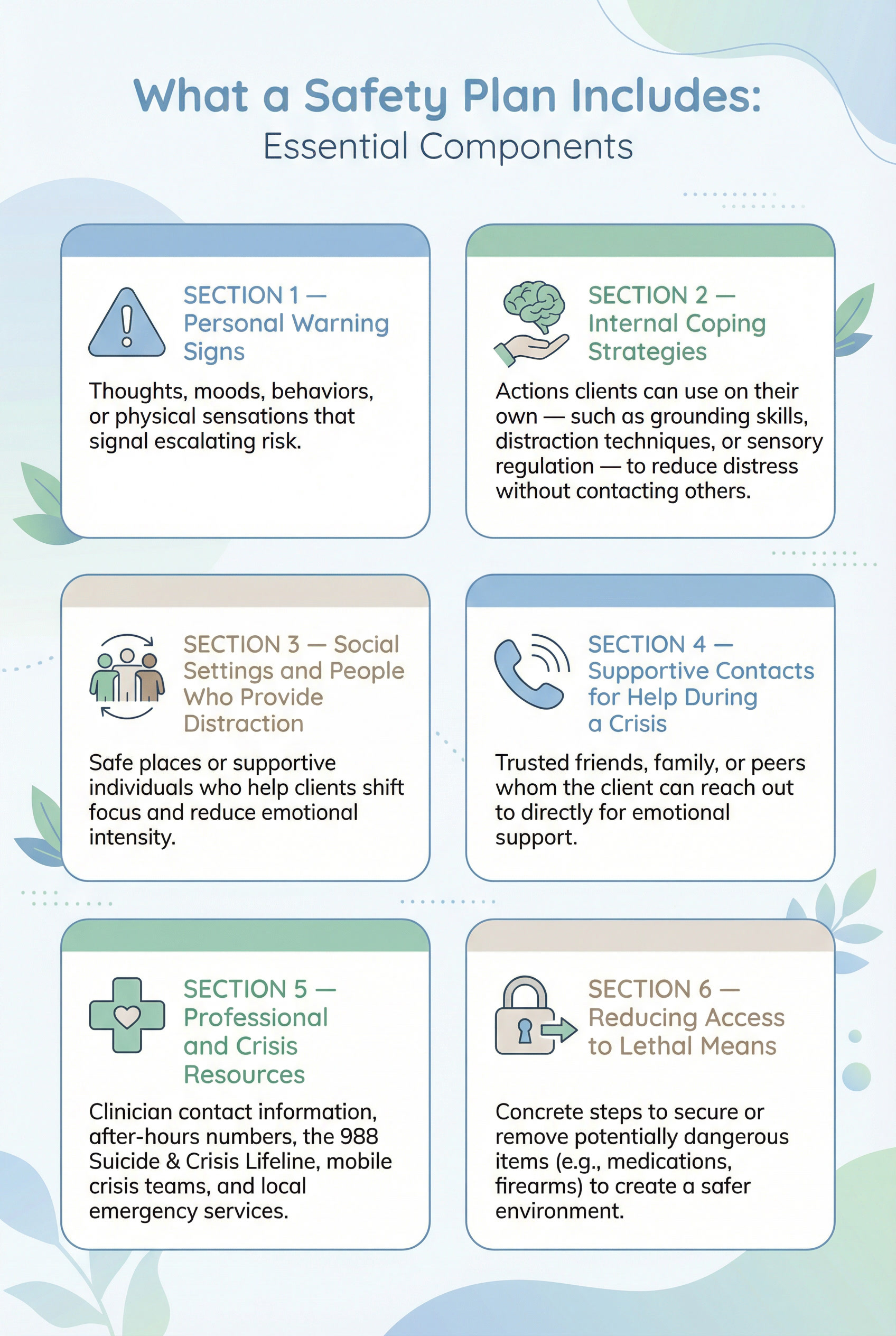
What a Safety Plan Includes: Essential Components
A well-designed mental health safety plan is structured, practical, and easy for clients to follow during moments of heightened distress. While formats may vary, evidence-based models like the Stanley-Brown Safety Planning Intervention consistently include six core components. These elements help clients recognize early warning signs, apply coping strategies, stay connected to support, and limit access to potentially lethal means. These components work together to create a written roadmap clients can rely on when their ability to problem-solve is impaired. By walking through each step collaboratively, clinicians can tailor the plan to the client’s strengths, environment, and real-world needs — making it far more likely to be used effectively in a crisis.
The Stanley-Brown Safety Planning Intervention (SPI): A Gold-Standard, Evidence-Based Model
The Stanley-Brown Safety Planning Intervention (SPI), developed by Dr. Barbara Stanley and Dr. Gregory Brown, is considered the gold standard in suicide safety planning. It is one of the most widely implemented and rigorously studied approaches worldwide, used across Veterans Health Administration systems, hospitals, crisis centers, outpatient clinics, and community mental health programs [4]. SPI stands out because it is structured, collaborative, and practical — giving clients a clear, usable plan to follow when suicidal thoughts escalate. Rather than relying on verbal assurances or vague agreements, SPI provides a step-by-step roadmap that clients can hold in their hands and apply in moments when problem-solving skills are impaired.
The Six Core Steps of the Safety Planning Intervention
SPI is organized around six essential components that work together to reduce risk and increase client safety:
1. Recognizing personal warning signs
Clients identify the thoughts, feelings, behaviors, or environmental triggers that signal risk is rising, allowing early intervention before a crisis peaks.
2. Using internal coping strategies
These are skills clients can use independently — such as grounding, paced breathing, physical activity, or distraction techniques — to lower emotional intensity.
3. Engaging social contacts and safe places for distraction
Clients identify people or environments that help them feel connected or distracted without immediately disclosing their crisis, which can interrupt harmful thought patterns.
4. Contacting supportive family or friends who can help in a crisis
This step involves identifying trusted individuals who can provide emotional support, help increase safety, or assist in accessing additional resources.
5. Reaching out to professionals and crisis resources
The plan includes specific clinician contact information, after-hours instructions, crisis hotlines, mobile crisis teams, and emergency services such as the 988 Suicide & Crisis Lifeline.
6. Making the environment safer by reducing access to lethal means
This crucial step involves identifying firearms, medications, sharp objects, or other means—and creating a clear strategy to secure, lock, or remove them.
Together, these steps guide clients from early detection to concrete action, improving their ability to stay safe during high-risk moments.
Why the Stanley-Brown Model Works
The strength of SPI lies in how it is designed and delivered:
- Brief: It can be completed within 20–30 minutes in most clinical settings.
- Collaborative: It is built with the client, not imposed on them, enhancing engagement and therapeutic alliance.
- Concrete: The final plan is a concise, one-page document in clear language, making it easy to reference during moments of distress.
- Portable: Clients leave the session with a physical or digital copy, ensuring support is available when they are outside the clinician’s office.
Because the intervention is straightforward, evidence-based, and adaptable to diverse practice environments, it has been widely implemented across the U.S. and internationally. Studies within the VA and other large systems show that SPI can significantly reduce suicidal behaviors, improve treatment adherence, and support safer care transitions.
Strengthen your suicide prevention workflow
Get your free Safety Planning Toolkit and learn how to build collaborative, evidence-based plans using the Stanley-Brown model — complete with worksheets, checklists, and sample documentation.
What the Research Shows About Safety Planning
This is where the conversation shifts from “good idea” to evidence-based intervention. Over the last decade, a growing body of evidence has confirmed what clinicians often observe in practice: a structured, collaborative safety plan can significantly reduce suicidal behavior and improve clinical outcomes.
Large VA Study: 45% Reduction in Suicidal Behaviors
One of the most influential studies comes from the Veterans Health Administration, where researchers compared usual care to the Stanley-Brown Safety Planning Intervention combined with follow-up contacts (SPI+)
In a large cohort comparison study of 1,640 suicidal patients seen in Veterans Health Administration emergency departments, clinicians used the Stanley-Brown Safety Planning Intervention plus structured follow-up calls (SPI+).
The findings were striking:
- 45% fewer suicidal behaviors in the 6 months after discharge
- About double the odds of attending at least one outpatient mental health visit in that period [5]
This is not a small effect. For every 44 patients who received SPI+ instead of usual care, one suicidal behavior event was prevented [6]. These improvements occurred across a large, diverse sample of high-risk individuals, demonstrating the intervention’s scalability and real-world impact.
Meta-Analyses Supporting Safety Planning Interventions
Meta-analyses and systematic reviews reinforce these results. A meta-analysis of safety planning type interventions (SPTIs) found that these approaches were associated with a 43% reduction in suicidal behavior, even when delivered as relatively brief interventions [7].
Another systematic review of 22 studies concluded that suicide safety planning interventions are generally effective at reducing suicidal behavior and ideation, and can also improve mental health symptoms, resilience, and service use [8].
The pattern is consistent:
When you actually sit down with patients, co-create a plan, write it out, practice it, and revisit it ... suicidal behavior goes down and engagement in treatment goes up.
Even when delivered as a brief intervention, a well-constructed safety plan increases a client’s ability to regulate distress, access support, and choose safer behaviors during a crisis. The evidence is clear: safety planning is not a symbolic gesture — it is an effective, actionable clinical tool.
How Safety Planning Improves Treatment Engagement
Safety planning does more than reduce immediate risk, it strengthens the therapeutic process in ways that directly improve treatment adherence and engagement. Because the plan is created collaboratively, clients experience the intervention as something done with them instead of to them. This strengthens rapport and signals that the clinician understands the client’s lived reality, fears, strengths, and struggles. When clients feel heard and empowered, they are more likely to remain engaged in therapy, attend follow-up sessions, and reach out before a crisis escalates.
Safety planning also increases engagement by giving clients a sense of agency and mastery. Instead of feeling overwhelmed by suicidal thoughts, clients gain a structured set of tools they can use independently. This fosters hope and self-efficacy, two essential drivers of continued treatment participation. Additionally, because the plan identifies specific people, places, and professional supports, it naturally builds a network of engagement beyond the therapy session. Clients know whom to call, what to do, and how to access care between sessions, reducing dropout and promoting continuity.
Finally, using a structured model like the Stanley-Brown SPI signals clinical consistency and reliability. Clients benefit when they see that their clinician follows an evidence-based process and revisits the safety plan regularly. This routine instills predictability and reinforces the idea that safety is part of the ongoing treatment, not only something addressed in moments of crisis. As a result, clients often become more open, cooperative, and proactive in therapy, leading to better outcomes over time.
Why Safety Planning Is Clinical Work, Not Paperwork
Clinically, a strong safety plan does several things at once.
1. It Extends the Session Into the Crisis Moment
The reality is that you are not in the room when the suicidal urge peaks. The plan is.
A well-constructed safety plan “borrows your brain” for the moment when executive functioning collapses and the patient cannot think clearly. Instead of needing to remember coping skills, they can follow the steps you built together.
2. It Strengthens the Therapeutic Alliance
Safety planning is inherently collaborative. You are asking:
- “What actually helps you, not in theory but on Tuesday night at 1:00 a.m.?”
- “Who do you genuinely feel safe calling?”
- “What do you need removed from your environment to get through this alive?”
Done well, the conversation itself is therapeutic. Patients experience you as an ally, not a gatekeeper. That alliance is protective.
3. It Improves Your Suicide Risk Formulation and Liability-Safe Documentation
From a documentation and liability perspective, a plan like Stanley-Brown lets you show:
- You assessed risk
- You engaged the patient in concrete, evidence-based safety planning
- You addressed means safety
- The patient received a copy and practiced key steps
- You arranged follow-up and coordination of care
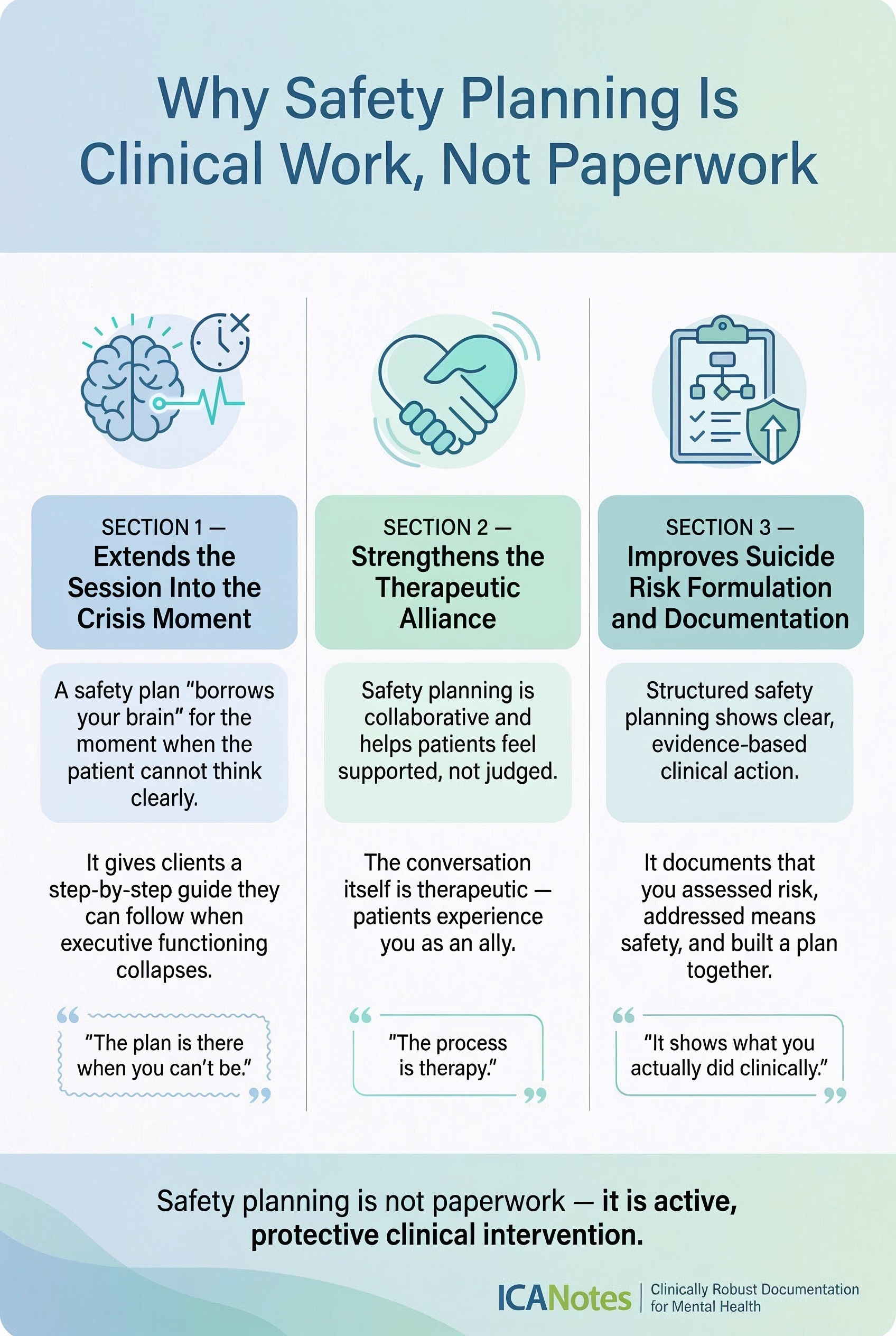
In fact, best-practice suicide documentation often includes language such as:
“Safety plan: Completed Stanley-Brown with patient; reviewed Steps 1–3 in session; patient received a copy; lethal means safety addressed.” [9]
That is not just defensive charting. It is a record that you did meaningful, evidence-aligned work.
For deeper legal context on liability considerations when suicidal ideation or imminent risk is present, see Legal Liability Issues in Suicide Care.
Why the Stanley-Brown Model Stands Out From Other Safety Plans
Many safety plans used in clinical practice today are pieced together from older templates, borrowed from outdated “no-harm contract” formats, or created informally within agencies. While well intentioned, these versions often lack essential components, do not follow an evidence-based protocol, and fail to address lethal means safety in a structured way. The Stanley-Brown Safety Planning Intervention (SPI) stands apart because it is grounded in research, clinically rigorous, and designed to be applied consistently across settings. Below are the key reasons this model remains the gold standard.
A Structured, Evidence-Based Clinical Protocol
Unlike generic safety plan templates, the Stanley-Brown model is tied directly to a clearly defined clinical protocol: the Safety Planning Intervention (SPI) [10]. This protocol outlines how clinicians should introduce, develop, and rehearse the safety plan collaboratively with clients. The process is explicit, evidence-based, and designed to support clinical reasoning rather than rely on intuition alone. Because SPI is standardized, clinicians across disciplines and settings can deliver the intervention in a way that is consistent, measurable, and grounded in best practices.
Proven Effective in High-Risk, Real-World Settings
One of the strongest arguments for the Stanley-Brown model is its extensive research base. SPI has been tested at scale in some of the most high-risk clinical environments, including Veterans Health Administration emergency departments — settings where patients often present with acute suicidal crises [11]. Studies show that when SPI is implemented, clients experience significant reductions in suicidal behaviors and increased engagement with outpatient care. This level of empirical support is rare among safety planning tools and is a major reason the model has become standard practice across large health systems.
Endorsed by National Organizations and Integrated with Lethal Means Counseling
The Stanley-Brown plan is recognized and disseminated by national suicide prevention organizations, crisis services, public health agencies, and hospital systems throughout the U.S. [12] Its widespread adoption reflects both its clinical effectiveness and its alignment with national guidelines for suicide prevention.
A distinguishing feature of the model is its explicit integration of lethal means counseling — a critical component often overlooked or minimized in other safety plans [13]. By embedding means safety directly into the step-by-step structure, SPI ensures that clinicians proactively address access to firearms, medications, and other potentially lethal items as part of the intervention, not as an optional add-on.
Together, these strengths mean that when clinicians use the Stanley-Brown model, they are not simply filling out a form — they are applying a validated, research-backed intervention with a clear lineage, defined procedures, and documented outcomes.
Bringing the Stanley-Brown Safety Plan Into Everyday Workflow with ICANotes
Here is the part that matters for your day to day practice:
You can believe in safety planning and still feel like you do not have the time or structure to do it well, especially if your documentation system makes it clunky.
ICANotes has made a different choice.
Built-In Safety Plan Template for Mental Health
Within ICANotes, the Stanley-Brown Safety Plan is available as a built-in safety plan template form, alongside other risk and self-harm tools. [14]
That means you can:
- Pull up the standardized Stanley-Brown layout inside the record
- Walk through each step collaboratively in session
- Capture patient-specific warning signs, coping strategies, supports, professional contacts, and means safety actions
- Save the plan in the chart and provide a copy to the patient (printed or via portal, depending on your configuration)
- Reference the plan directly in your progress notes, crisis notes, and discharge summaries
It moves safety planning from “extra work” to a natural extension of your clinical workflow. This approach closely parallels Step 6 of the crisis intervention process, where clinicians and clients collaborate to develop an actionable plan that promotes safety, stability, and continuity of care after a crisis.
How Clinicians Use the Safety Plan Inside ICANotes
Clinicians often pair the Stanley-Brown form with:
- A structured suicide risk assessment
- A clear risk formulation statement
- Follow-up plans (phone check, early return visit, outreach after no-show)
- Documentation that specific steps of the safety plan were practiced in session
The result is a chart that tells a coherent story:
We identified risk. We used an evidence-based safety plan. We addressed means safety. We provided a written plan. We arranged and documented follow-up.
That story matters to patients, to families, to payers, and to regulators. Most importantly, it can matter to whether your patient survives the week.
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
- Complete Notes in Minutes - Purpose-built for behavioral health charting
- Always Audit-Ready – Structured documentation that meets payer requirements
- Keep Your Schedule Full – Automated reminders reduce costly no-shows
- Engage Clients Seamlessly – Secure portal for forms, messages, and payments
- HIPAA-Compliant Telehealth built into your workflow
Complete Notes in Minutes – Purpose-built for behavioral health charting
Always Audit-Ready – Structured documentation that meets payer requirements
Keep Your Schedule Full – Automated reminders reduce costly no-shows
Engage Clients Seamlessly – Secure portal for forms, messages, and payments
HIPAA-Compliant Telehealth built into your workflow
Bringing It All Together: Making Safety Planning a Standard of Care
You cannot control every variable in a patient’s life. You cannot single-handedly reverse national suicide trends, although I am sure you wish you could.
But you can control this:
- You can stop relying on outdated “no-harm contracts.”
- You can make safety planning a standard part of care for patients at elevated risk.
- You can use a model that has actual data behind it ... the Stanley-Brown Safety Planning Intervention.
- You can embed that work directly in your documentation system so it is repeatable, reviewable, and easy to teach across your team.
In a world where suicide deaths continue to climb, doing the “bare minimum” is not enough. Safety planning is not busywork. It is suicide prevention in real time.
If you are already using ICANotes, the Stanley-Brown Safety Plan is ready for you inside the system. If you are not using it yet, this is the moment to decide that every patient you identify as at risk will leave your care with more than a warning ... they will leave with a plan.
Frequently Asked Questions: Mental Health Safety Plans
Related Posts
About the Authors
Dr. October Boyles is a behavioral health expert and clinical leader with extensive expertise in nursing, compliance, and healthcare operations. With a Doctor of Nursing Practice (DNP) and advanced degrees in nursing, she specializes in evidence-based practices, EHR optimization, and improving outcomes in behavioral health settings. Dr. Boyles is passionate about empowering clinicians with the tools and strategies needed to deliver high-quality, patient-centered care.
Dr. Virna Little is a distinguished leader in behavioral health integration. She is the co-founder of Concert Health, a behavioral health medical group that provides Collaborative Care to organizations across 21 states. Dr. Little is also the Co-Founder and CEO of Zero Overdose, a national non-profit focused on overdose safety planning to reduce unintentional overdose events and deaths. Dr. Little has served as a member of the national Zero Suicide faculty and a consultant who fostered the development of integrated delivery systems nationally in all 50 states and internationally. Dr. Little holds a Doctoral degree in Psychology and a Master's in Social Work. A nationally and internationally recognized speaker, Dr. Little has presented on suicide prevention strategies at the White House. She has received numerous awards for her work in integrating primary care and behavioral health and serves on multiple boards.










