Blog > Compliance > Joint Commission Compliance Roadmap for Behavioral Health
How Joint Commission Compliance Protects Patient Safety
This article offers a clear, practical roadmap to understanding and achieving Joint Commission compliance, specifically tailored for behavioral health clinicians. It explains why accreditation matters not just for regulatory approval and reimbursement, but for improving patient safety, reducing risk, and building a culture of continuous quality improvement. You will learn what surveyors actually look for, how to prepare staff and documentation, and why accreditation can be a strategic advantage rather than a burden. If you're a behavioral health professional aiming to strengthen safety standards, reduce liability, and boost your organization's credibility, this guide is a must-read.

Last Updated: August 15, 2025


What You'll Learn
- What The Joint Commission is and why it matters.
- How accreditation improves patient safety, with real-world evidence and stats you can share with leadership.
- The standards and requirements you’ll actually need to meet.
- Practical, professional strategies for preparing for an unannounced survey.
- The business case for accreditation—why it’s not just about checking boxes but about building a sustainable, trusted practice.
Contents
- What is The Joint Commission?
- How Joint Commission Compliance Improves Patient Safety
- Why Joint Commission Compliance Matters to Your Organization
- Common Joint Commission Compliance Requirements: What You Need to Meet
- How to Prepare for a Joint Commission Survey
- Final Thoughts: Joint Commission Compliance is an Investment in Safety
Healthcare is one of the most highly regulated industries in the world, and for good reason. When people come to us, they’re trusting us with their health, their safety, and often their lives. That’s why Joint Commission compliance isn’t just bureaucracy. It’s a commitment. It’s an outward sign to patients, payers, and our own teams that we prioritize quality and safety in every interaction.
The Joint Commission is one of the most recognized, respected, and widely adopted accreditation bodies. Over 22,000 organizations in the U.S. hold Joint Commission accreditation, from major hospital systems to outpatient clinics, behavioral health providers, ambulatory surgery centers, and home health agencies.
What is The Joint Commission?
The Joint Commission is an independent, nonprofit organization that accredits and certifies healthcare organizations and programs in the United States. Founded in 1951, it has become the gold standard for healthcare quality, safety, and continuous improvement.
Joint Commission accreditation is not a government program, but CMS (Centers for Medicare & Medicaid Services) has granted it “deeming authority.” This means that accredited hospitals are considered to meet Medicare Conditions of Participation, making it practically essential for organizations that want to bill Medicare or Medicaid.
Here’s why that matters:
- CMS accounts for over 20% of U.S. healthcare spending. Without accreditation, many facilities simply cannot survive financially.
- Many commercial insurers also require accreditation as part of their network agreements.
- State licensing agencies often look to Joint Commission accreditation as evidence of meeting minimum standards.
Beyond the regulatory side, Joint Commission accreditation has become a signal of quality to patients and families. When someone sees that seal, they know you’re committed to meeting recognized, evidence-based standards. A 2017 study published in JAMA Internal Medicine found that 30-day mortality rates dropped by 1.7% during unannounced Joint Commission accreditation surveys — from 7.21% to 7.03%. This suggests that hospitals may function at a higher level of vigilance and care when they are being actively evaluated, reinforcing the link between accreditation and patient safety.
How Joint Commission Compliance Improves Patient Safety
Let’s be clear: the real value of accreditation isn’t in the survey itself. It’s in the standards and the process of continuous readiness that reduce harm and save lives.
Healthcare is complex. Mistakes don’t just happen because someone is sloppy, they happen because systems fail. Accreditation pushes organizations to examine those systems with rigor and humility.

Joint Commission Compliance Matters
Accreditation is a powerful differentiator in competitive markets, with many hospitals featuring their Joint Commission Gold Seal prominently in marketing materials.
Joint Commission accreditation also attracts quality staff who want to work in organizations committed to best practices.
National Patient Safety Goals (NPSGs)
A cornerstone of The Joint Commission’s approach is the National Patient Safety Goals, which focus on key, high-risk areas. Every accredited organization has to demonstrate how it meets these goals in daily practice.
Examples of NPSGs include:
- Accurately identifying patients to prevent errors.
- Improving communication among caregivers.
- Using medications safely, with clear labeling and reconciliation.
- Reducing healthcare-associated infections through proven protocols.
- Identifying safety risks, such as suicide risk, in behavioral health settings.
Stat: Healthcare-associated infections (HAIs) affect 1 in 31 hospital patients on any given day in the U.S. The CDC estimates 687,000 HAIs occur annually, contributing to 72,000 deaths. Implementing evidence-based infection prevention strategies—including those mandated by Joint Commission standards—can reduce these infections by up to 30%.
Joint Commission standards force organizations to build systems that mitigate these risks.
Evidence-Based Standards, Not Guesswork
The Joint Commission doesn’t make up rules arbitrarily. Its standards reflect:
- CDC guidelines for infection prevention.
- American Society of Health-System Pharmacists (ASHP) best practices for medication management.
- OSHA requirements for environmental safety.
- CMS Conditions of Participation for quality and safety.
This alignment ensures that accreditation isn’t just a hoop to jump through, it’s about applying the best available evidence to prevent harm.
Real-World Impact of Joint Commission Compliance
It’s easy to be cynical about regulatory compliance until you see what happens without it.
Consider:
- Medication errors are the most common medical error in hospitals. The FDA estimates 1.3 million people are injured by medication errors annually in the U.S.
- A 2019 study in BMJ Quality & Safety found that better hospital safety ratings correlated with significantly lower 30-day mortality rates for conditions like heart failure and pneumonia.
- Joint Commission-accredited behavioral health programs reduce suicide risk by implementing standardized screening and assessment protocols.
Accreditation requirements force organizations to systematize these safety practices, not leave them to individual discretion.
Why Joint Commission Compliance Matters to Your Organization
If you’re in leadership or management, you already know accreditation is “important.” But let’s be frank—it’s expensive, time-consuming, and sometimes frustrating.
So why invest in it?
Regulatory and Payer Requirements
- CMS requires “deemed status” accreditation for hospitals billing Medicare/Medicaid.
- Many private payers won’t contract with non-accredited facilities.
- Accreditation often substitutes for state licensing inspections or requirements.
If you want to get paid and stay open, accreditation is often non-negotiable.
Legal Protection and Risk Reduction
Accreditation demonstrates that you’re meeting nationally accepted standards of care. This can be critical in malpractice or liability cases.
- Plaintiffs’ attorneys often argue that facilities deviated from accepted standards. Accreditation is evidence you didn’t.
- Risk management programs tied to accreditation reduce the frequency and severity of incidents.
Stat: The average cost of a malpractice claim in the U.S. is over $300,000. Proactive risk management reduces claim frequency by up to 30%.
Marketing and Patient Trust
Patients are savvier than they used to be. Patients care deeply about where they receive care, and reputation matters. In a national evaluation of hospital-choice factors published in 2020, 61.9% of patients identified hospital reputation as a key driver in their decision-making, followed by physician experience (51.5%).
Healthcare professionals universally recognize that reputation is often built on trusted, rigorous standards — like those upheld by The Joint Commission.
- For decades, The Joint Commission has set the gold standard in healthcare quality and safety, and its accreditation is a strong signal of clinical excellence and organizational accountability. While patients may not always know the term “accreditation,” they often feel its impact — in safer care, better systems, and stronger clinical outcomes.
- Accreditation is a powerful differentiator in competitive markets.
- Many hospitals feature their Joint Commission Gold Seal prominently in marketing materials.
It’s not just about patients, either. Joint Commission accreditation attracts quality staff who want to work in organizations committed to best practices.
Continuous Quality Improvement
Accreditation isn’t a one-time audit, it’s a framework for ongoing improvement.
Organizations that embrace Joint Commission accreditation as a tool (rather than a burden) often see:
- Better clinical outcomes.
- Higher staff satisfaction.
- Improved operational efficiency.
- Fewer sentinel events.
Joint Commission compliance forces organizations to ask the hard questions: Are we doing what we say we do? Are our policies followed? Is our training adequate?
Common Joint Commission Compliance Requirements: What You Need to Meet
Let’s get practical. What will surveyors actually look for?
Joint Commission standards cover dozens of domains, but here are the big buckets:
Documentation and Policy Management
- Written policies and procedures that reflect current practice and best standards.
- Staff must know and follow these policies consistently.
- Medical record documentation must be accurate, timely, complete, and legible.
Surveyors will spot-check records and quiz staff on policy details.
Tip: Policies in a binder don’t help if staff have never read them.
Environment of Care
- Fire safety compliance, including drills and extinguisher checks.
- Hazardous materials management.
- Emergency preparedness for natural disasters, active shooters, and utility failures.
- Life safety code compliance.
Stat: NFPA estimates that U.S. healthcare facilities experience over 5,000 fires per year, many preventable through basic compliance.
Medication Management
- Safe storage, security, and temperature controls.
- High-alert medication protocols.
- Medication reconciliation at transitions of care.
- Pharmacist oversight where required.
Surveyors often “trace” a medication order from prescribing to administration to ensure safety at every step.
Infection Prevention and Control
- Robust hand hygiene program.
- Standard and transmission-based precautions.
- Sterilization and disinfection processes.
- Surveillance and tracking of infection rates.
- Staff training on infection control.
Stat: Proper hand hygiene alone can reduce HAIs by up to 40%.
Leadership and Governance
- Clear lines of accountability for safety and quality.
- Leadership commitment to a culture of safety.
- Reporting systems for staff to share safety concerns without fear.
- Evidence of continuous quality improvement efforts.
Staff Training and Competency
- Thorough onboarding and orientation for new hires.
- Annual mandatory training (fire safety, infection control, NPSGs).
- Competency validations for clinical roles.
- Continuing education opportunities.
Staff at every level must understand their role in maintaining safety standards.
Tip: Surveyors often interview housekeeping, dietary, and maintenance staff about safety goals. Everyone is accountable.
How to Prepare for a Joint Commission Survey
One of the most stressful parts of accreditation is the unannounced nature of surveys.
Joint Commission surveys typically occur every three years, but the exact date isn’t shared in advance. This approach is deliberate, it ensures facilities maintain continuous readiness rather than scrambling before an inspection.
So how do you get ready?
Conduct Mock Surveys
- Simulate a real survey experience.
- Include staff interviews, document reviews, and facility inspections.
- Identify and fix compliance gaps.
- Repeat regularly, not just before the survey window.
Pro Tip: Consider using external consultants for objective assessments and staff coaching.
Review and Update Policies
- Ensure every policy is current, approved, and aligned with actual practice.
- Eliminate conflicting or obsolete procedures.
- Make policies easily accessible to staff.
Review and Update Policies
- Ensure every policy is current, approved, and aligned with actual practice.
- Eliminate conflicting or obsolete procedures.
- Make policies easily accessible to staff.
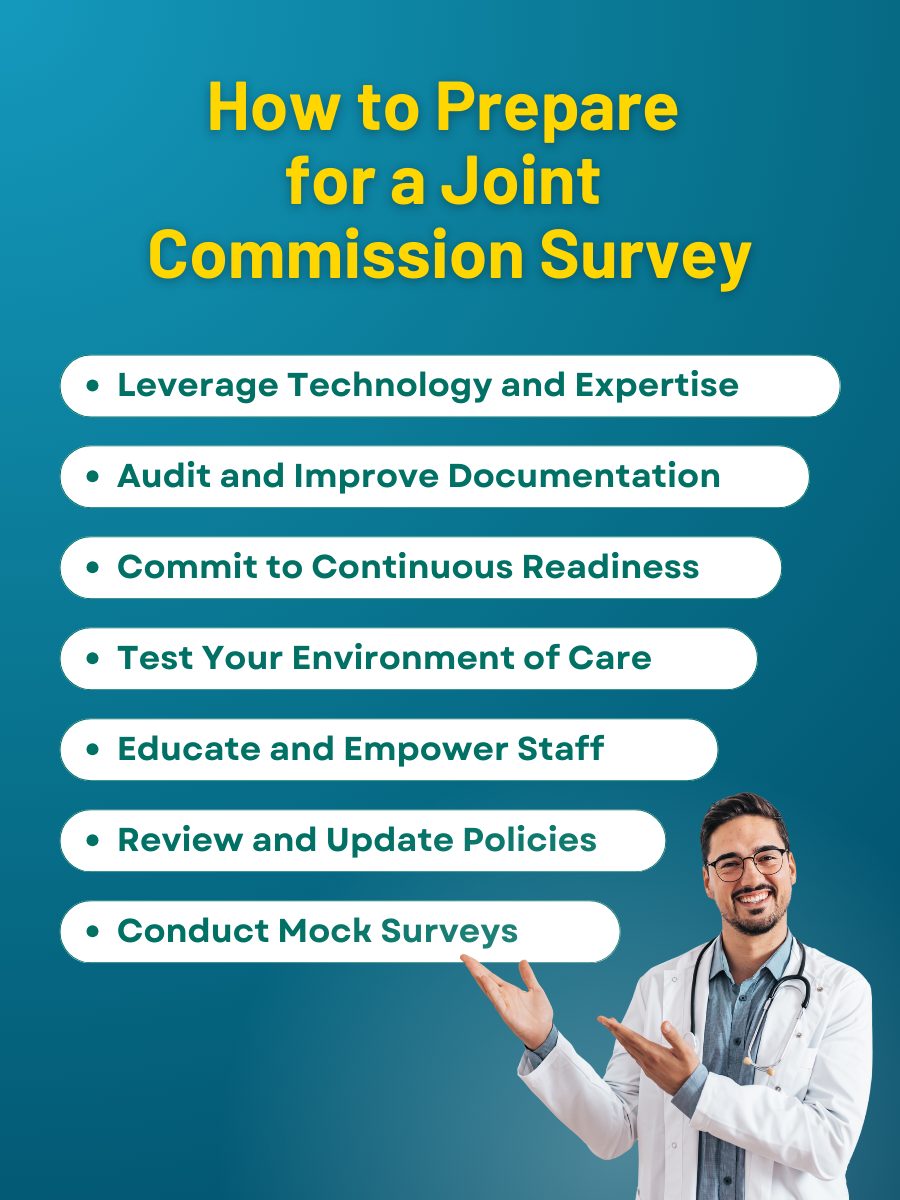
Educate and Empower Staff
- Hold regular training sessions on NPSGs and other key standards.
- Role-play survey interview questions.
- Foster a culture where staff ask questions rather than guess.
- Emphasize that everyone plays a role in safety—from nursing to facilities to dietary services.
Tip: Staff knowledge and engagement are the single strongest predictors of successful surveys.
Audit and Improve Documentation
- Review a sample of patient records for completeness and consistency.
- Standardize documentation practices.
- Address gaps in timeliness, signatures, and required elements.
Test Your Environment of Care
- Check corridors and exits for obstructions.
- Verify fire extinguishers are inspected and tagged.
- Review emergency plans with staff.
- Conduct realistic drills.
Leverage Technology and Expertise
- Use accreditation prep software to track compliance items.
- Consider external consultants to supplement internal expertise.
- Document everything. If it’s not documented, surveyors will assume it didn’t happen.
Commit to Continuous Readiness
- Embed accreditation requirements into daily operations.
- Don’t wait for the survey window to address gaps.
- Use monthly safety huddles, quarterly policy reviews, and ongoing training.
By normalizing readiness, you avoid panic and deliver safer care every day.
Final Thoughts: Joint Commission Compliance is an Investment in Safety
Let’s be honest: accreditation is hard work. It requires time, money, and constant vigilance.
But it’s worth it.
Joint Commission compliance isn’t about pleasing surveyors, it’s about protecting patients, staff, and your organization’s future.
✅ Fewer adverse events.
✅ Reduced liability exposure.
✅ Higher staff morale and retention.
✅ Better payer relationships.
✅ Marketing advantage that builds patient trust.
At its best, accreditation is not a box to check but a framework for excellence. It’s a way of saying: We take this seriously. We don’t cut corners. We will never stop improving.
If you’re preparing for a survey now, my advice is simple: start today. Review your policies, train your staff, audit your records, and embrace the mindset that readiness is every day, not once every three years.
Because at the end of the day, accreditation isn’t about passing an inspection. It’s about delivering care that is safe, effective, and worthy of the trust patients place in us.
How ICANotes Supports Joint Commission Compliance for Behavioral Health Providers
Joint Commission surveys don’t just look at what your policies say—they evaluate whether those policies are actually reflected in daily practice, documentation, and staff behavior. That’s where the ICANotes Behavioral Health EHR makes a measurable difference.
Structured Clinical Documentation That Meets Accreditation Standards
ICANotes’ pre-configured templates for intake assessments, progress notes, treatment plans, and discharge summaries are specifically designed to align with behavioral health documentation standards. Templates help ensure:
-
Risk assessments (e.g., suicide risk) are consistently documented.
-
Treatment goals are measurable, time-bound, and individualized.
-
Discharge planning includes aftercare, referrals, and patient understanding.
Audit-Ready Records With Less Manual Work
Surveyors often spot-check documentation for completeness, legibility, and timeliness. ICANotes helps you stay ready with:
-
Timestamped, legible entries stored in a secure, cloud-based system.
-
Version control and access logs for compliance audits.
-
Alerts and required fields to reduce missing elements.
Compliance-Driven Workflows and Role-Based Permissions
ICANotes allows organizations to configure role-based access to documentation, helping support HIPAA compliance and Joint Commission standards for information security. Built-in workflows guide staff through processes such as:
-
Treatment plan reviews and sign-offs.
-
Medication reconciliation tracking.
-
Staff credentialing and onboarding records (with integration options).
Seamless Integration With Billing and Reporting
From CMS documentation requirements to payer audits, ICANotes helps behavioral health organizations demonstrate that services are medically necessary, well-documented, and tied to measurable outcomes. This reduces risk and supports:
-
Evidence of standards compliance (ESC).
-
Denial prevention with proper coding and progress documentation.
-
Transparency in performance improvement initiatives.
Continuous Readiness, Not Last-Minute Scrambling
Because ICANotes standardizes workflows and embeds documentation best practices into the day-to-day operations of your team, you can build a culture of continuous readiness, the very mindset Joint Commission surveyors look for.
Frequently Asked Questions






