The Impact of Chronic Illness on Mental Health — A Guide for Clinicians
The onset and formal diagnosis of a chronic illness undoubtedly brings about a myriad of complex emotional reactions including depression, anxiety, fear, and grief. While these emotional reactions are common and not always indicative of a deeper mental health concern, there is evidence to support a correlative relationship between chronic illness and mental health conditions. Individuals living with diabetes are 2 to 3 times more likely to develop depression. What may be startling is that those individuals diagnosed with both diabetes and depression are at a 46% increased risk for all-cause mortality compared to those with diabetes who do not show depressive symptoms [1].
While there is a growing recognition of the connection between mental and physical health, effectively treating chronic illness requires a stronger integration of mental health, primary care, and specialty care services. [1] As clinicians working with individuals with either a chronic illness or depression or other mental health condition, it is important to recognize and understand the bidirectional relationship and how to address it in a clinical setting.
Throughout this article, we will establish a baseline understanding about the correlative relationship between chronic illness and mental health, identify key challenges faced by both the individual and clinician in a therapeutic setting, and explore strategies for best practice.
Understanding the Connection Between Mental Health and Chronic Illness
There is ample evidence to support the correlative relationship between being diagnosed and living with a chronic illness and the onset of a mental health diagnosis. For example, a 2021 cross-sectional study found that four types of chronic diseases (cholesterol disease, kidney disease, coronary heart disease, and asthma) were significantly associated with mental health problems [2].
Inversely, individuals who are diagnosed with depression are at an increased risk for developing chronic physical conditions including diabetes, heart disease, stroke, osteoporosis, and Alzheimer's disease [3]. This can be due to a variety of reasons including an overall decrease in physical activity, socialization, and poor nutrition, as well as the physiological changes in body function as a result of depression, including inflammation, reduced blood circulation, heart rate abnormalities, and increased stress hormones.
While it is widely understood that the diagnosis of a chronic illness can deeply impact an individual’s mental health, thus simultaneously impacting the chronic condition, the emotional component of a diagnosis is often overlooked. Unfortunately, in cases where an individual is living with a chronic illness and is in need of significant self care as a form of symptom management, depression inherently makes it difficult to do so [1]. In fact, according to the American Diabetes Association, when examining the impact of depression on diabetes, evidence supports a significant impairment to glycemic control, physical activity, higher weights, and diabetes-related organ functioning [4].
Key Mental Health Challenges Faced by Patients with Chronic Illness
A. Depression
Depression is the most commonly associated mental health condition alongside a chronic illness. Individuals faced with a chronic illness will undergo a variety of changes to their life including activities of daily living, medication management, energy levels, and relationships. These significant changes can bring about strong feelings of isolation and depression. According to the CDC, 51% of Parkinson’s patients, 42% of cancer patients, 27% of diabetes patients, 23% of cerebrovascular patients, 17% of cardiovascular patients, and 11% of Alzheimer’s patients also have depression.
B. Anxiety Disorders
Anxiety can be seen often co-occurring with a chronic illness both at the onset or diagnosis, as well as during illness maintenance. Uncertainty around the trajectory of the illness can play a significant role in an individual’s ability to manage anxiety around it, as well as anxiety around factors of life that are impacted by the illness including job security, travel, relationships, finances, and medication management. According to the National Library of Medicine, roughly 50% of individuals diagnosed with a chronic illness report moderate to severe anxiety throughout the course of their illness [5].
Best Practices for Clinicians: Supporting the Mental Health of Patients with Chronic Illness
Clinicians working with clients who are navigating chronic illness should be aware of the correlation between chronic illness and certain mental health conditions. While working through the complexities of a new diagnosis, special care should always be paid to the client’s mental health ongoing. The following practices can be used as a guide for care for this special population.
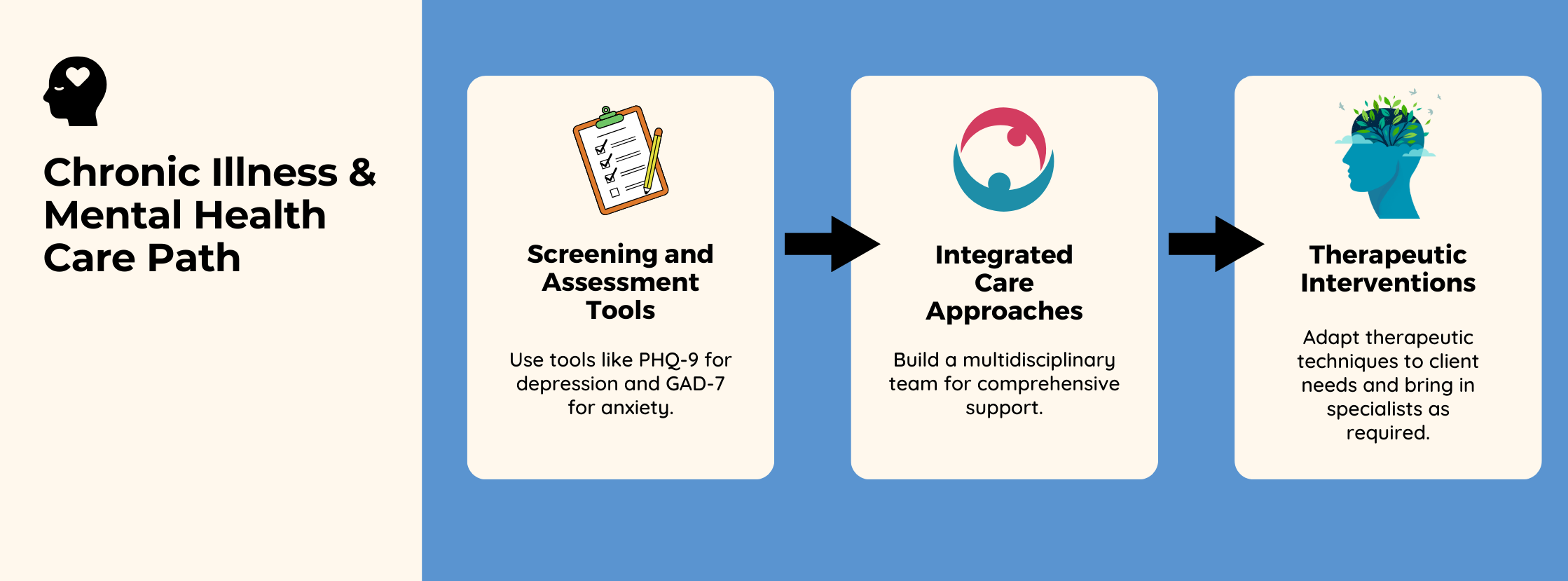
Screening and Assessment Tools
Assessment for mental health conditions like depression and anxiety are essential tools throughout the treatment process. It is also important to keep in mind that while these symptoms may not be present at the diagnosis of an illness, they may begin to present themselves as the client continues to navigate significant changes and challenges throughout the illness progression while navigating symptoms and life stressors related to the diagnosis. Some tools that might prove useful in this ongoing assessment include the PHQ-9 for depression, GAD-7 for anxiety.
Integrated Care Approaches
Due to the physical components of a chronic health condition, it is important to weave together a multidisciplinary care team that can address the needs of the whole case. This may include physicians, social workers, dieticians, home health workers, and insurance care navigators alongside mental health support. Ensuring that a client has needs met across the spectrum of what may present itself throughout the treatment course, ensures that the client feels and is well cared for in all capacities so they can focus on their health, knowing that they have the support needed in every arena.
Therapeutic Interventions
A variety of therapeutic interventions can be used to support clients for ongoing mental health support and should be determined by the clinician’s specialty skillset, as it matches the client’s needs. This can include, but is not limited to Cognitive Behavioral Therapy (CBT), Narrative Therapy, or Acceptance and Commitment Therapy (ACT). However, due to the complex nature of navigating a chronic illness alongside a mental health condition, it is important for the primary clinician to keep in mind the potential need for specialized care, either through themselves or by bringing in a specialist. The choice within this matter would again depend on the expertise of the primary clinician to be aware of what areas are outside of their professional scope.
Some examples of specialty needs may include:
- Grief Counseling
- Trauma Therapy
- Mindfulness-Based Stress Reduction
- Family or Couples Counseling
- Eye Movement Desensitization and Reprocessing (EMDR)
Throughout the therapeutic relationship, it is essential that the client’s unique experience remain the focal point of all care. While some sessions may focus on disease management, others may center around relationships, grief, or financial barriers. Supporting an individual with a chronic illness may require a long-term treatment outline that allows for long periods of not needing any support at all. It is important to remember that progress may look different for each individual due to the unique and complex nature of how the chronic illness and mental health conditions present themselves across the span of a client’s life.
How ICANotes Supports Clinicians Who Work With Clients Managing Chronic Illness
Incorporating ICANotes into clinical practice can significantly enhance the treatment clinicians provide to clients managing chronic illness. With its robust electronic health record (EHR) system, ICANotes streamlines the documentation process, allowing clinicians to focus more on patient care and less on administrative tasks. The platform offers customizable templates for psychiatric assessments and treatment plans, which are essential for tailoring care to the unique needs of each client with a chronic illness.
ICANotes facilitates integrated care by providing tools for medication management and electronic lab orders, ensuring a comprehensive approach to both mental and physical health care. This integration is crucial for addressing the complex interplay between chronic illnesses and mental health conditions.
ICANotes empowers clinicians to deliver holistic and efficient care, ultimately enhancing the quality of life for individuals living with chronic illnesses.
Sign up for a free trial (no credit card required) or schedule a demo to explore how ICANotes can support your work with clients.
About the Author

Kaylee, a certified grief counselor and social worker, has dedicated the past decade to reshaping our understanding and support of grief. With experience at a nonprofit hospice, she's empowered individuals to navigate their grief journeys, recognizing that loss extends beyond death. As an author, speaker, and event organizer, Kaylee fosters spaces for acknowledging and embracing life's most challenging moments. Her work has been featured across various media, amplifying voices and broadening awareness of the diverse sources of grief in our lives.
Recent Posts
Sources
- https://publichealth.jhu.edu/2021/the-intersection-of-mental-health-and-chronic-disease
- https://www.sciencedirect.com/science/article/abs/pii/S2212657023000491
- https://www.nimh.nih.gov/health/publications/chronic-illness-mental-health
- https://diabetesjournals.org/care/article/27/9/2154/22613/Relationship-of-Depression-and-Diabetes-Self-Care#ref-9
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4768533/

