Blog > Treatment Strategies > How to Write a Grief Treatment Plan
How to Write a Grief Treatment Plan: Goals, Objectives, and Examples
A grief treatment plan is a structured, clinician-led framework that supports clients through their grief journey as they struggle to adapt to loss. It defines personalized treatment goals, measurable objectives, and therapeutic interventions to help clients process grief, maintain functioning, and adjust after a significant loss. This guide shows mental health professionals when a grief treatment plan is appropriate and how to write one, including setting effective SMART goals in grief therapy.

Last Updated: December 29, 2025

Grief is a universal experience. Within each of our lifetimes, we will experience losses that trigger grief to varying degrees, impacted by a number of unique factors, from person to person, and loss to loss. Due to the wide range of intensity around each grief experience, many individuals are able to engage with natural support systems and do not seek professional mental health services. The need for professional support is not as clear cut as you may think. Some individuals will seek support due to intense feelings of hopelessness and anhedonia, others due to an overall lack of natural social supports, and others will find that grief support is needed among additional mental health concerns already being addressed by a professional.
As a therapist or counselor, your job is to support individuals in grief as they navigate their complex feelings associated with the loss, adjust to life without the deceased, and encourage a re-engagement into life while maintaining a lasting connection with the person who has died. While there are some modalities and strategies to supporting anyone who is experiencing grief, such as William Worden's Four Tasks of Mourning, or Elizabeth Kubler-Ross' 5 Stages of Grief, there may be times when a higher level of intervention may be needed due to issues with persistent complex bereavement, disenfranchised grief, and underlying mental health conditions triggered by grief, such as trauma and clinical depression. This guide will examine the different types of grief and how you can develop a customized treatment plan for each client's unique needs.
Clear and thoughtful treatment planning is essential in grief work. While grief is a natural response to loss, some clients benefit from structured, goal-directed support that can be documented and reviewed over time. As grief presentations vary widely, clinicians need practical frameworks that support ethical care, continuity, and accurate documentation without pathologizing normal grief.
What is Grief?
Grief is a term used to describe the feelings, behaviors, and thoughts someone experiences due to the loss of something or someone close to their heart. When you hear the term “grief,” you likely think of losing a loved one. This is the most common loss associated with grief, however grief can be experienced through the loss of something meaningful to a person. This may include, but is not limited to job loss, the diagnosis of a life-limiting or terminal illness, divorce or other loss of a relationship, aging, and mobility.
Each of these losses, whether they are publicly recognized as loss or not, contain feelings of grief and mourning. Grief is the internal feeling associated with grief, while mourning is the external expression of those internal feelings. These two experiences combined make-up a term we call "bereavement." Due to the complexity of each grief process, it is impossible to clearly define a grief reaction that is standard across all bereaved individuals. In clinical practice, grief is described in broad patterns to support assessment and treatment planning.
What is a Grief Treatment Plan?
A grief treatment plan is a structured, documented plan that outlines goals, objectives, and interventions to support a client coping with loss. It is used when grief significantly affects emotional well-being, daily functioning, or mental health and requires more than informal support.
The plan identifies key grief-related concerns, sets measurable goals, and guides care over time. Its purpose is not to eliminate grief, but to reduce distress, support adaptation, and help clients function while integrating their loss.
Grief treatment plans are individualized and flexible. They reflect the client’s circumstances and are reviewed and adjusted as grief evolves to support ethical, clinically appropriate care.
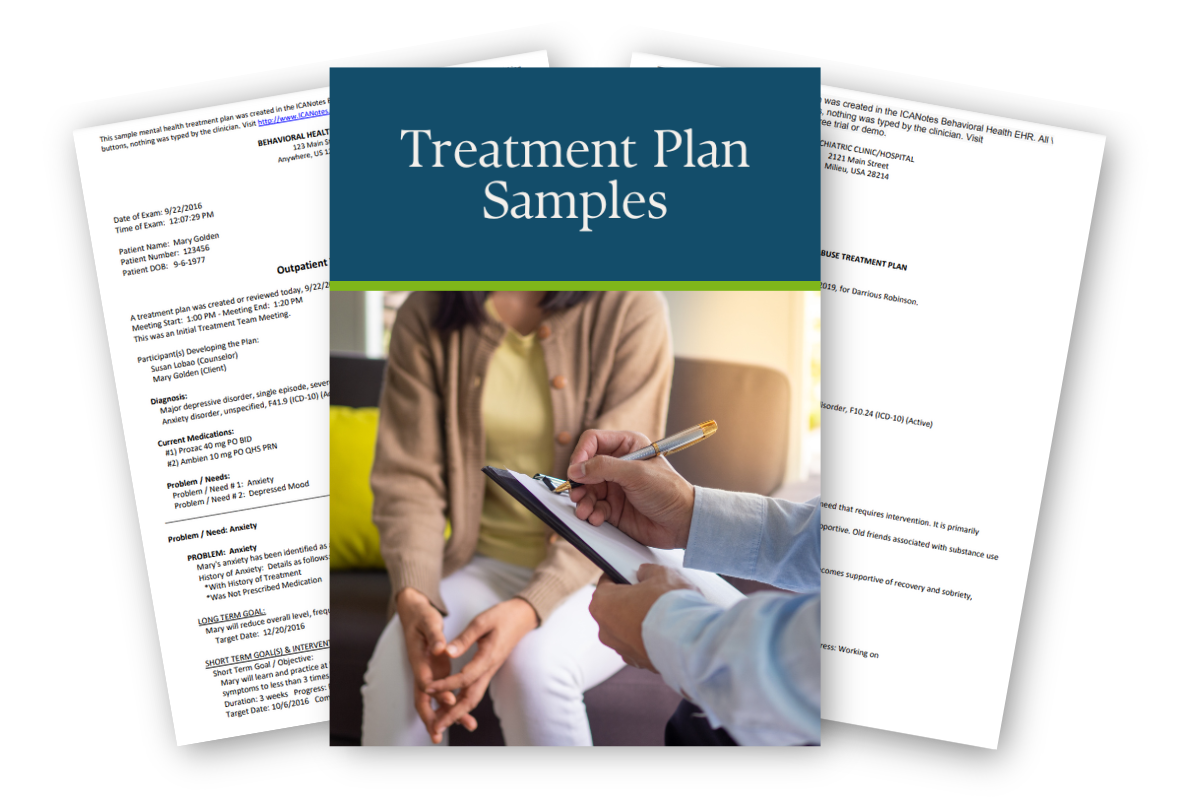
Access Our Sample Treatment Plan Library
Get instant access to our full library of sample treatment plans.
When is a Treatment Plan for Grief and Loss Clinically Appropriate?
Grief is a normal response to loss, and many clients adapt over time with support and routine. In these cases, formal treatment planning may not be necessary. A grief treatment plan is appropriate when grief does not ease over time or begins to significantly disrupt emotional well-being, daily functioning, or mental health.
Normal Grief vs Grief Requiring Intervention
Normal grief often includes sadness, longing, disrupted sleep, and emotional fluctuation. These reactions may be intense but usually lessen over time, allowing clients to maintain basic responsibilities and experience moments of relief.
Grief may require clinical intervention when distress is persistent, worsening, or functionally limiting. Signs include emotional numbness, preoccupation with the loss, avoidance of reminders, or a sense of being unable to move forward. In these cases, a structured treatment plan can support adaptation and reduce impairment.

Functional Impairment Indicators
Functional impairment is one of the clearest indicators that treatment planning may be appropriate. Clinicians may consider formal planning when grief interferes with:
- Work, school, or caregiving responsibilities
- Relationships and social engagement
- Sleep, appetite, or basic self-care
- Concentration, decision-making, or emotional regulation.
When these difficulties persist or worsen over time, treatment goals and documented interventions can help stabilise functioning and support recovery.
Risk Factors and Comorbidities
Certain factors increase the likelihood that grief will become complex or prolonged. These include sudden or violent loss, limited social support, prior trauma, or unresolved relationship dynamics with the deceased. A history of anxiety, depression, trauma-related disorders, or substance use can also complicate the grief process.
Grief that occurs alongside other mental health conditions often benefits from coordinated, goal-directed treatment. In these cases, a treatment plan helps clinicians address overlapping symptoms while respecting the individual grief experience.
Clinical Considerations and DSM-5-TR
The DSM-5-TR recognises prolonged grief disorder as a diagnosable condition when grief responses are persistent, severe, and impairing beyond culturally expected timeframes. However, most grief does not meet diagnostic criteria and does not require pathologisation.
A grief treatment plan does not require a formal diagnosis. Its purpose is to support clinical judgment, guide care, and document progress when grief becomes disruptive or complex. Careful assessment, cultural awareness, and ongoing review help ensure treatment remains appropriate and client-centred.
Types of Grief and Treatment Planning Considerations
Grief presents in different patterns over time. Recognizing these patterns helps clinicians determine when supportive care is sufficient and when structured treatment planning is appropriate. These categories are clinical reference points, not fixed stages.
Acute Grief
Typical presentation
Acute grief commonly occurs in the first months following a loss. Clients may experience intense sadness, yearning, guilt, disrupted sleep, poor concentration, emotional numbness, or physical distress. Emotions often fluctuate, and moments of relief or connection may occur alongside pain.
Treatment focus
The clinical focus is typically on emotional support, validation, and stabilization. Psychoeducation, normalization of grief responses, and strengthening existing coping strategies are often sufficient.
When formal planning is usually unnecessary
In many cases, acute grief does not require a formal treatment plan. Clients are often able to maintain basic functioning and gradually adapt with time, social support, and routine.
Indicators that planning may be warranted
Structured treatment planning may be appropriate if acute grief intensifies over time, interferes with daily functioning, or is accompanied by significant avoidance, persistent distress, or comorbid mental health concerns.
Integrated Grief
Common clinical patterns
Integrated grief reflects ongoing adjustment to loss. Clients may return to daily routines while continuing to experience sadness, longing, or emotional pain at times. The loss becomes part of their lived experience rather than the central focus of daily functioning.
Normal oscillation of symptoms
Grief reactions may resurface around anniversaries, holidays, or reminders. This fluctuation is expected and does not indicate regression. Grief is not linear, and periods of stability can coexist with renewed emotional pain.
Treatment planning considerations during reintegration
Treatment planning during this phase may focus on maintaining functioning, reinforcing coping skills, and supporting meaning-making. Formal plans are often brief and flexible, with goals centered on resilience, role functioning, and emotional regulation.
Complicated Grief
Defining characteristics
Complicated grief involves persistent, intense distress that does not ease with time. Clients may experience ongoing preoccupation with the loss, intrusive memories, strong guilt, avoidance of reminders, or a sense that life cannot move forward.
Clinical risks
This presentation is associated with increased risk of depression, anxiety, trauma-related symptoms, social withdrawal, and functional impairment. Clients may struggle to engage in work, relationships, or self-care.
When structured treatment planning is essential
Formal, structured treatment planning is often necessary in cases of complicated grief. Clear goals, measurable objectives, and documented interventions help guide care, monitor progress, and support sustained clinical engagement while respecting the individual grief process.
Core Components of an Effective Grief Treatment Plan
An effective grief treatment plan provides structure without prescribing how a client should grieve. It clarifies the focus of care, supports clinical judgment, and allows progress to be reviewed and adjusted over time. These core components help ensure plans remain ethical, individualized, and clinically useful.
Treatment Goals for Grief and Loss
Treatment goals for grief should be client-centered and outcome-focused. They describe what the client is working toward, rather than how quickly grief should resolve. Effective goals focus on improving functioning, reducing distress, and supporting healthy adaptation to loss.
Goals should avoid pathologizing normal grief responses. The aim is not to eliminate sadness, longing, or emotional pain, but to help clients engage in daily life, regulate emotions, and cope with grief in sustainable ways.
Examples of appropriate goal framing include:
- Improve the client’s ability to manage grief-related distress without avoidance.
- Support re-engagement in work, relationships, or caregiving roles.
- Increase emotional regulation and coping skills related to loss.
- Reduce functional impairment associated with grief.
Measurable Objectives
Objectives differ from goals in that they define how progress will be observed and evaluated. While goals describe the desired outcome, objectives break that outcome into specific, measurable steps that can be reviewed over time.
Effective objectives are time-bound and observable. They help clinicians track progress while allowing flexibility as grief fluctuates. Objectives should be realistic and aligned with the client’s stage of grief and capacity for change.
Examples of objectives linked to grief presentations include:
- Client will resume one social or routine activity per week within four weeks.
- Client will practice identified coping strategies during periods of grief-related distress.
- Client will report improved sleep consistency over a defined review period.
- Client will reduce avoidance of grief-related reminders with clinician support.
Clinical Interventions
Clinical interventions describe the therapeutic methods used to help clients meet their goals and objectives. Interventions should be selected based on the client’s needs, grief presentation, and clinical history, rather than applied uniformly.
Interventions must align clearly with stated goals and objectives. For example, interventions aimed at reducing avoidance should support functional re-engagement, while interventions addressing rumination or guilt should support emotional regulation and meaning-making.
Grief treatment plans should remain flexible. As grief evolves, goals, objectives, and interventions may need to be reassessed and adjusted. Regular review helps ensure care remains appropriate, responsive, and centered on the client’s experience.
Sample Treatment Plan for Grief and Loss
The following example reflects how a grief treatment plan may be documented in clinical practice. It is provided for educational purposes and should be adapted to the individual client’s presentation, context, and clinical judgment.

Sample Grief Treatment Plan
Client Presentation
Client is a 46-year-old adult presenting with grief following the death of a long-term partner nine months ago. Client reports persistent sadness, sleep disturbance, reduced concentration, and social withdrawal. Grief-related distress increases around reminders of the loss. Client continues to meet basic responsibilities, but reports decreased motivation and difficulty experiencing pleasure. No current suicidal intent reported.
Primary Problem
Unresolved grief contributing to emotional distress, functional impairment, and avoidance of grief-related reminders.
Long-Term Treatment Goals
- Client will adapt to the loss in a way that allows for improved daily functioning and emotional regulation.
- Client will reduce grief-related distress while maintaining a healthy emotional connection to the deceased.
Short-Term Goals
- Increase the client’s ability to manage acute grief-related distress.
- Improve consistency in daily routines and social engagement.
Objectives
- Client will identify and practice at least two coping strategies to manage grief-related distress within four weeks.
- Client will resume participation in at least one social or routine activity per week within one month.
- Client will reduce avoidance of identified grief triggers through gradual exposure over a six-week period.
- Client will report improved sleep consistency, defined as five or more nights per week of adequate sleep, within six weeks.
Interventions
- Provide psychoeducation regarding grief, mourning, and the non-linear nature of the grief process.
- Utilize cognitive and behavioral strategies to address avoidance, rumination, and grief-related guilt.
- Support emotional regulation through grounding, mindfulness, and relaxation techniques.
- Implement behavioral activation to encourage gradual re-engagement in meaningful activities.
- Monitor mood, sleep, and functional impairment throughout treatment.
Review and Adjustment Plan
Treatment progress will be reviewed every four to six weeks. Goals and objectives will be adjusted based on changes in symptom severity, functional capacity, and client feedback. Increased grief intensity around anniversaries or reminders will be anticipated and addressed within the treatment plan. Continued treatment will be guided by clinical progress and client needs.
Expected Outcome
Client demonstrates improved coping with grief-related distress, increased engagement in daily activities, and greater emotional flexibility while continuing to process the loss.
Therapeutic Interventions Used in Grief Treatment Plans
Clients process grief in different ways, and therapeutic interventions should be selected based on individual needs and clinical context. The most effective approach depends on factors such as the type of loss, symptom presentation, and treatment goals. In some cases, combining interventions may provide better support than using a single approach.
1. Cognitive Behavioral Therapy
Cognitive behavioral therapy helps clients identify unhelpful thought patterns and behaviors that contribute to grief-related distress. In grief treatment plans, CBT focuses on improving coping, reducing avoidance, and supporting healthier interpretations of the loss.
With CBT, clinicians can:
- Identify and address unhelpful behaviors or avoidance patterns.
- Introduce adaptive coping strategies.
- Support the development of a new narrative around the loss.
Use cognitive restructuring to challenge negative thought patterns.
2. Acceptance and Commitment Therapy
Acceptance and commitment therapy helps clients relate differently to grief by increasing psychological flexibility rather than avoiding painful emotions. In grief treatment plans, ACT supports acceptance, present-moment awareness, and values-based action.
With ACT, clinicians can:
- Help clients identify personal values
- Support acceptance of difficult emotions related to loss
- Encourage present-focused awareness through mindfulness
- Reduce experiential avoidance
- Promote engagement in meaningful activities despite emotional pain.
3. Traumatic Grief Therapy

Some cases of grief also involve trauma, which can result from an unexpected or violent death or even being present and witnessing the loved one as they passed. Trauma can often mask grief and make it difficult to accept the feelings or go through the normal grieving process. Traumatic grief therapy focuses on the trauma response alongside the grief itself, disentangling the two emotions to help the client heal.
4. Companioning
Companioning focuses on presence, empathy, and validation rather than analysis or problem-solving. The clinician provides a supportive, non-judgmental space where clients can express grief openly, offering reassurance and emotional support by walking alongside them through the grieving process.
5. Complicated Grief Therapy
Complicated grief therapy supports clients experiencing prolonged, intense grief that significantly interferes with daily functioning. Treatment helps reduce fixation on the loss, address avoidance, and support acceptance and adaptation, often integrating elements of acceptance-based approaches.
6. Group Therapy
Group therapy allows grieving clients to share experiences with others who have experienced similar losses. It can reduce isolation, normalize grief responses, and provide emotional support, particularly for clients with limited personal support systems.
7. Bibliotherapy
Bibliotherapy encourages clients to engage with written material related to grief and loss to support reflection and emotional processing. Reading about shared experiences can help clients feel validated, understood, and less alone as they navigate grief.
8. Art Therapy
Art therapy offers a creative outlet for expressing grief when verbal communication is difficult. Through activities such as drawing, painting, or collage, clients can explore emotions, regulate distress, and reconnect with meaning in a supportive therapeutic context.
9. Play Therapy
Play therapy is commonly used with children who are grieving a significant loss. Through play, storytelling, or symbolic activities, children can express emotions, process experiences, and develop coping skills in a developmentally appropriate way.
10. Interpersonal Therapy
Interpersonal therapy addresses grief within the context of relationships and social roles. Treatment explores the client’s relationship with the deceased and examines how the loss has affected current relationships, communication, and patterns of connection or withdrawal.
You can also ask your client to speak honestly about their memories of their loved ones and how the event has affected their relationships with others. For instance, some grieving people may pull away from their significant other, friends, or family and self-isolate.
SMART Goals for Grief Therapy
SMART goals can support grief therapy by providing structure without imposing unrealistic expectations. When goals are specific, measurable, and time-bound, they help clinicians and clients focus on functional progress while recognizing that grief does not follow a fixed timeline.
In grief treatment, SMART goals should prioritize coping, functioning, and emotional regulation rather than eliminating grief. Goals should remain flexible and be reviewed or adjusted as grief fluctuates over time
Examples of SMART Goals for Grief and Loss
Short-term SMART goals often focus on stabilisation and day-to-day functioning. Examples include:
- Client will identify and use at least two coping strategies during periods of acute grief-related distress over the next four weeks.
- Client will resume one routine or social activity per week within one month.
- Client will establish a consistent sleep routine on at least five nights per week over a three-week period.
Long-term SMART goals support adaptation and reintegration. Examples include:
- Client will engage in work, caregiving, or social roles with reduced grief-related disruption within six months.
- Client will report improved emotional regulation when experiencing grief triggers over a defined review period.
- Client will develop a personal narrative that integrates the loss while maintaining future-oriented goals.
Measuring Progress Without Invalidating Grief
Progress in grief therapy should be measured through changes in functioning, coping, and emotional regulation rather than the absence of grief. Continued sadness or longing does not indicate treatment failure. Instead, clinicians should assess whether clients are better able to manage distress, engage in daily life, and respond flexibly to grief-related triggers.
Using SMART goals in this way allows clinicians to document meaningful progress while respecting the ongoing and individual nature of grief.
Documenting Progress and Adjusting Grief Treatment Plans
Accurate documentation plays a key role in effective grief treatment. Clear records support continuity of care, inform clinical decision-making, and help ensure treatment remains appropriate as grief evolves.
Monitoring Symptom Change and Functional Improvement
Progress in grief treatment is best assessed through changes in functioning, coping, and emotional regulation. Clinicians should note shifts in sleep, concentration, social engagement, and daily routines, recognizing that progress may be gradual and non-linear.
Documentation should capture both gains and setbacks. Increased grief does not necessarily indicate a lack of progress. Notes should reflect how clients respond to distress and use coping strategies.
Revising Goals as Grief Evolves
Grief treatment plans should be reviewed regularly and updated as the client’s needs change. Early goals may focus on stabilization and basic functioning, while later goals may shift toward meaning-making, reintegration, or long-term adjustment.
Revising goals is a normal part of grief treatment. Adjustments should be documented clearly, with a rationale linked to observed changes in symptoms, functioning, or life circumstances. Flexible planning helps ensure care remains responsive rather than prescriptive.
Ethical Documentation Considerations
Ethical grief documentation requires careful language. Clinicians should avoid framing normal grief responses as pathology or measuring success by the absence of sadness. Notes should reflect respect for the client’s individual grief process, cultural context, and personal values.
Documentation should be objective, clinically relevant, and free from judgment. Clear descriptions of behaviors, functional impact, and client-reported experiences support ethical care and professional standards.
Avoiding Over-Treatment of Healthy Grief
Not all grief requires ongoing clinical intervention. As clients demonstrate improved coping and functioning, clinicians should consider tapering or concluding treatment. Documentation should reflect the clinical reasoning behind reducing session frequency or closing treatment.
Avoiding over-treatment protects clients from unnecessary pathologization and supports ethical practice. Effective grief treatment planning recognizes when support is no longer needed, and documents progress toward resolution or transition appropriately.
Write Better Grief Treatment Plans with ICANotes
No matter how grief presents for your clients, accurate and consistent documentation is essential for tracking progress and adjusting treatment plans over time. Clear records help ensure continuity of care while preventing over-treatment of healthy grief. However, time-consuming documentation can disrupt clinical flow and reduce time spent with clients.
With ICANotes, you can efficiently document grief treatment plans using intuitive templates and assessment tools designed for mental health professionals. ICANotes provides a robust, easy-to-use EHR that supports compliant documentation, collaboration, and clinical best practices, helping reduce documentation burden so you can focus on client care. Schedule a demo or start a free trial to see how ICANotes can support your practice.
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
- Complete Notes in Minutes - Purpose-built for behavioral health charting
- Always Audit-Ready – Structured documentation that meets payer requirements
- Keep Your Schedule Full – Automated reminders reduce costly no-shows
- Engage Clients Seamlessly – Secure portal for forms, messages, and payments
- HIPAA-Compliant Telehealth built into your workflow
Complete Notes in Minutes – Purpose-built for behavioral health charting
Always Audit-Ready – Structured documentation that meets payer requirements
Keep Your Schedule Full – Automated reminders reduce costly no-shows
Engage Clients Seamlessly – Secure portal for forms, messages, and payments
HIPAA-Compliant Telehealth built into your workflow
Frequently Asked Questions
Kaylee, a certified grief counselor and social worker, has dedicated the past decade to reshaping our understanding and support of grief. With experience at a nonprofit hospice, she's empowered individuals to navigate their grief journeys, recognizing that loss extends beyond death. As an author, speaker, and event organizer, Kaylee fosters spaces for acknowledging and embracing life's most challenging moments. Her work has been featured across various media, amplifying voices and broadening awareness of the diverse sources of grief in our lives.