Blog > Documentation > Case Management Notes: Tips, Examples and Templates
How to Write an Effective Case Management Note (With Examples and Templates)
Writing effective case management notes is essential for tracking client progress, coordinating care, and ensuring documentation meets professional and legal standards. This comprehensive guide covers everything case managers and social workers need to know — from choosing the right note format (SOAP, DAP, BIRP) to documenting treatment plan progress and protecting client privacy in sensitive cases. You’ll find detailed case management notes examples and a downloadable case management notes checklist for easy reference.

Last Updated: August 29, 2025


What You'll Learn
-
How to structure a case management note template with all the essential components
-
Best practices for writing objective, legally sound, and privacy-protected documentation
- How to protect client privacy when documenting sensitive topics
-
Real-world case management note examples across multiple settings and formats (SOAP, DAP, BIRP, GIRP)
Contents
- Best Practices for Writing Effective Case Management Notes
- Case Notes in Social Work: Unique Considerations
- How to Protect Client Privacy in Case Notes
- Case Management Note Formats and Examples
- Key Components of a Case Management Note Template
- Common Case Management Documentation Errors
- Technology and Software for Case Management Notes
Case management notes are foundational in social work, serving as a reliable record of a client’s journey, ensuring continuity of care, and improving outcomes by enabling social workers and other professionals to collaborate efficiently. Well-crafted case management notes document the delivery of social services, reflect client progress, and support compliance, legal, and ethical requirements.
What is a Case Management Note?
A case management note is a written record that documents a case manager’s interaction with a client. These notes help ensure continuity of care, track progress toward treatment goals, and support accountability in multidisciplinary teams. In mental health and social work, these notes also serve legal, clinical, and operational functions, especially when justifying services for insurance reimbursement or coordinating services across agencies.
Best Practices for Writing an Effective Case Management Note
High-quality case notes must be accurate, complete, clear, concise, timely, and readable. Effective documentation in social work also requires that every case management note is factual and objective to support the client’s needs and ensure clear communication with colleagues.
Ensure Case Notes are Accurate and Complete
One of the best practices for writing your notes is ensuring they are accurate and complete. Not only should you include a brief description of the interaction, but you may also want to add details relevant to this specific case that would be helpful to another person reading your notes. The note must include your client’s name, date of birth, and medical record number. After writing your note, reread it to check for accuracy. You should also always add your signature and the date to your case management note. Incomplete, inaccurate, or unfinished notes are not acceptable.
Write Clearly and Concisely
More is not always better. When it comes to writing your case management notes, you should keep them clear and concise. Focus on the information that is relevant to your goals for case management. If you include too much unnecessary detail, it may be challenging to find the pivotal information you're looking for in your case management notes. A well-structured case note example can serve as a guide for maintaining clarity and conciseness.
Complete Your Case Management Notes the Same Day
Your case management notes should be completed in a timely manner. It is best practice for notes to be completed on the same day. If you wait until the next day or several days after, you will not be able to retain the details from the interaction with your client. It is crucial to carve out space in your schedule to write your notes. Write your notes as quickly as possible after making contact with a client.
Keep Case Notes Organized and Readable
Case manager notes need to be readable. Typically, typing these notes makes it easier for other staff members to decipher and access them. Your software can also check the text for spelling and grammar issues. Keep in mind that you want someone else to be able to read your notes and understand everything you've included. If your notes aren't legible and an emergency arises, this can become a liability issue. Don't use abbreviations or shorthand that other social worker notes wouldn't be able to understand. It is also important to organize your case management notes chronologically, with your most recent notes starting first.
Align Case Notes with Goals and Objectives
Creating case management notes that reference treatment plan goals and objectives ensures your documentation is directly tied to the client’s overall care plan. Each note should connect the day’s interaction to measurable progress, barriers, or next steps related to established objectives. For example, if a client’s treatment plan includes the goal of achieving stable housing within three months, your case management note might document outreach to a housing authority, assistance completing a rental application, or discussion of budgeting resources. By aligning notes with these specific objectives, you create a clear record of how services provided support the client’s broader treatment plan, while also demonstrating accountability and progress over time.
Free Download: Case Management Note Checklist
Download our free Case Management Note Checklist to ensure every note you write is clear, compliant, and aligned with your client’s goals—perfect for busy social workers who want stronger outcomes in less time.
When writing case notes in social work, you may be documenting more than clinical care:
- Multidisciplinary collaboration with school, housing, court, or child welfare systems
- Cultural sensitivity and inclusive language
- Strength-based perspectives emphasizing client autonomy
Social work documentation often balances service delivery with advocacy, so clarity and ethics are especially important.
How to Protect Client Privacy in Case Notes
Sensitive topics like domestic violence, substance use, immigration status, or legal involvement must be handled with extra care. Protect confidentiality by:
- Avoiding unnecessary personal detail that doesn't directly impact care
- Using non-identifying references when documenting third-party risks (e.g., "partner," "family member")
- Limiting information to what is clinically relevant and legally required
- Following HIPAA and 42 CFR Part 2 guidelines
- Documenting safety concerns using facts, not speculation
If in doubt, consult a supervisor before including high-risk content.
Case Management Note Formats and Examples
Several commonly accepted formats exist for writing case management notes in social work. Using note templates increases efficiency and ensures critical information is not missed.
| Format | Stands For | Best Use in Case Management |
|---|---|---|
| SOAP | Subjective, Objective, Assessment, Plan | Useful when payer or clinical teams expect a medical-style structure; clearly separates observed facts from assessment and next steps. |
| DAP | Data, Assessment, Plan | Concise, facts-forward documentation for outreach, check-ins, and brief encounters where logistics and coordination are primary. |
| BIRP | Behavior, Intervention, Response, Plan | Ideal when tracking observable behaviors and outcomes tied to services provided (e.g., referrals, advocacy, skills coaching). |
| GIRP | Goal, Intervention, Response, Plan | Best for documenting progress toward treatment plan goals (e.g., housing, employment, benefits), linking each contact to a goal. |
| PIRP | Problem, Intervention, Response, Plan | Effective for issue-focused updates (transportation barriers, missed appointments, paperwork hurdles) with clear actions and follow-up. |
Choose a format that aligns with your organization’s workflow and documentation needs.

SOAP Note Example (Mental Health Setting)
Subjective: Client reports increased anxiety in crowded places.
Objective: Client avoided group activities, appeared restless during session.
Assessment: Symptoms consistent with social anxiety disorder; progress toward goal stalled this week.
Plan: Schedule small group exposure activity; review coping strategies at next session.

DAP Note Example (Substance Use Setting)
Data: Client attended session, disclosed relapse (alcohol consumption 2x/week).
Assessment: Motivated to get back on track, insight into triggers present.
Plan: Develop a relapse prevention plan, sponsor check-in.

BIRP Note Example (Community Social Work)
Behavior: Client did not return required paperwork, reported barriers with transportation.
Intervention: Provided bus voucher, assisted with form completion.
Response: Client expressed gratitude, paperwork completed.
Plan: Follow up on benefits status next week.

GIRP Note Example (Case Management, Elder Care)
Goal: Maintain independent living status.
Intervention: Coordinated home health aid referral.
Response: Client receptive.
Plan: Confirm care schedule, review adaptation next visit.
Key Components of a Case Management Note Template
Regardless of the note format used, a comprehensive case management notes template should include:
1. Client Information
- Full name, date of birth, medical record number, date/time of contact
2. Purpose of Contact
- Why the interaction occurred (e.g., follow-up, referral, assessment, crisis intervention)
3. Description of Interaction
- Objective summary of the conversation, services provided, or actions taken
4. Treatment Plan Progress
- Reference current treatment goals and document any progress, setbacks, or changes
5. Interventions and Resources Provided
- Any referrals, support offered, educational materials shared, or advocacy efforts made
6. Client Response
- How the client reacted or participated (e.g., engaged, declined service, reported improvement)
7. Follow-Up Plan
- Next steps, scheduled appointments, or future coordination needed
8. Signature and Credentials
- Name, title, and credentials of the case manager completing the not
Social Work Case Notes Examples in Different Settings

Hospital Discharge Planning (SOAP Format)
Subjective: Client concerned about accessing medication post-discharge.
Objective: Client lacks insurance; pharmacy identified as low-cost alternative.
Assessment: Needs support navigating Rx program.
Plan: Submit application to community health fund.

Outpatient Mental Health (DAP Format)
Data: Client reports receiving a job interview offer after applying to 12 jobs.
Assessment: Client's mood is improved. Remains anxious about transportation to job.
Plan: Provide bus voucher and revisit employment goal next session.

Substance Use Recovery (BIRP Format)
Behavior: Client disclosed cravings after conflict with roommate.
Intervention: Reviewed coping skills worksheet; role-played refusal techniques.
Response: Client engaged and reported reduced urge.
Plan: Follow up in group therapy next week.

School-Based Social Work (GIRP Format)
Goal: Improve classroom attendance.
Intervention: Collaborated with parent and teacher to develop morning routine.
Response: Parent agreed to implement checklist.
Plan: Check-in after one week.
Common Case Management Documentation Errors
Avoid these pitfalls to ensure your notes are clinically sound and legally defensible:
- Generalizations: Instead of writing "Client is doing better," write "Client attended three scheduled appointments this week and reported feeling less anxious at work."
- Grammar or Spelling Mistakes: A note that reads "clinet missd meds" can create confusion. Correctly document: "Client missed two doses of prescribed medication this week."
- Personal Opinions or Unverified Diagnoses: Avoid "Client seems lazy." Replace with "Client reported difficulty completing household tasks due to ongoing fatigue."
- Casual Language or Abbreviations: Instead of "Pt. super stressed RN," use "Client expressed high stress related to current housing situation."
- Judgmental or Biased Phrasing: Avoid "Client is non-compliant." Use "Client did not attend scheduled appointment and reported transportation barriers."
Use objective, behavioral language grounded in facts.
Frequently Asked Questions About Social Work Case Management Notes
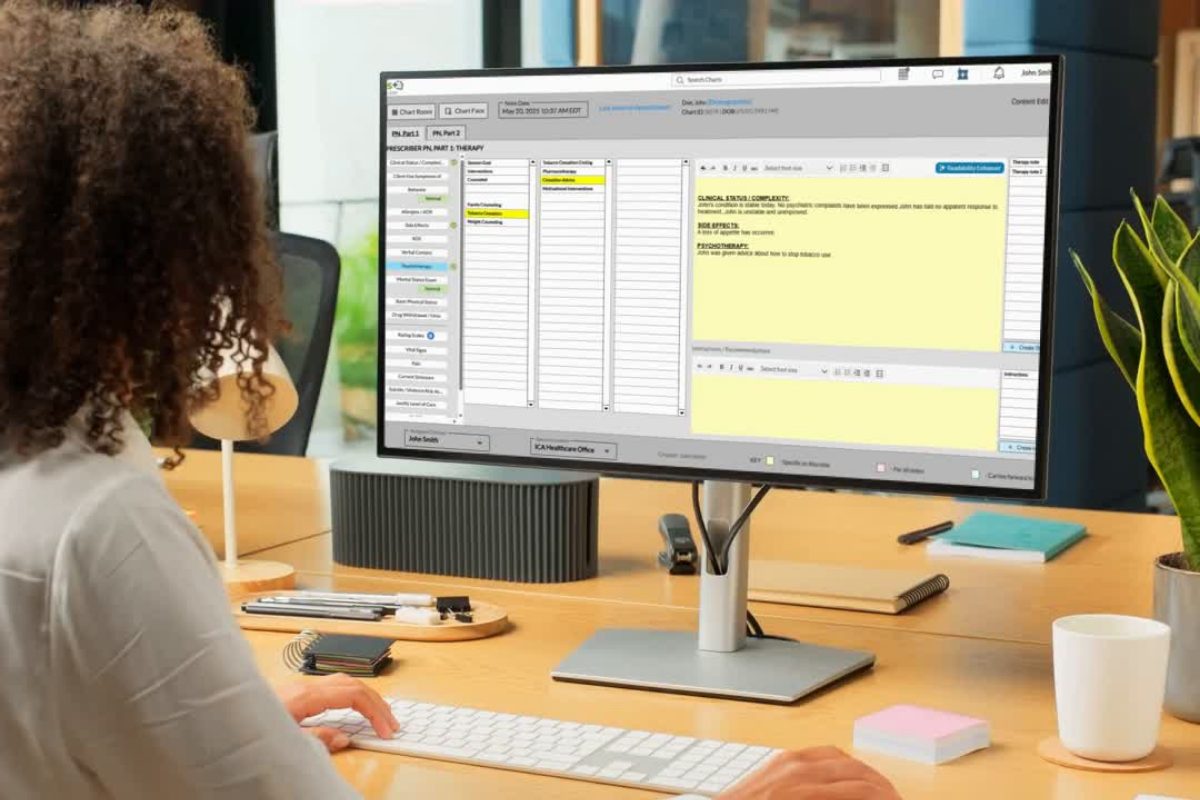
Technology and Software for Case Management Notes
Documentation doesn’t have to be a burden. Modern case management software, like ICANotes, streamlines documentation and ensures adherence to best practices in social work.
Key Features:
-
Access notes securely from any device
-
Use built-in menu-driven templates for case management notes
-
Integrated scheduling, billing, and communication
-
Let clients complete forms and history intake online via a patient portal
- Share updates with the care team through secure messaging
Digital case notes facilitate collaboration among social workers, counselors, supervisors, and social work case teams. Whether you're writing case notes in social work or documenting progress in outpatient behavioral health, ICANotes makes it easier to stay compliant and organized.
Book a demo or sign up for a free trial and find out how you can write a case management note in 3 minutes.
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
- Complete Notes in Minutes - Purpose-built for behavioral health charting
- Always Audit-Ready – Structured documentation that meets payer requirements
- Keep Your Schedule Full – Automated reminders reduce costly no-shows
- Engage Clients Seamlessly – Secure portal for forms, messages, and payments
- HIPAA-Compliant Telehealth built into your workflow
Complete Notes in Minutes – Purpose-built for behavioral health charting
Always Audit-Ready – Structured documentation that meets payer requirements
Keep Your Schedule Full – Automated reminders reduce costly no-shows
Engage Clients Seamlessly – Secure portal for forms, messages, and payments
HIPAA-Compliant Telehealth built into your workflow
Related Posts
Donald Morrison graduated from UNC Charlotte in 2004. He has since worked as a school-based therapist, inpatient social work supervisor and outpatient clinician. Donald currently works in private practice, and he is also an adjunct faculty member at the UNC Charlotte School of Social Work. In addition, Donald serves as a clinical supervisor to LCSW associates, and he regularly presents at area mental health conferences and seminars.







Case Notes in Social Work: Unique Considerations