Mental health professionals face unique emotional and cognitive demands that make intentional self-care essential for ethical, sustainable practice. This guide explores the evidence-based strategies clinicians need to stay grounded — including a therapist burnout self-check, practical self-care tips, and a printable mental health self-care checklist to support long-term resilience and well-being.

Last Updated: November 21, 2025

What You'll Learn
- Why self-care is essential for mental health professionals and how it supports ethical, sustainable clinical practice.
- How Maslow’s Hierarchy of Needs applies to clinician well-being and what foundational needs must be met to prevent burnout.
- Early signs and symptoms of therapist burnout, compassion fatigue, and secondary traumatic stress—and how to identify them in yourself.
- Evidence-based self-care tips for mental health professionals, including emotional, cognitive, physical, relational, and professional strategies.
- How to build a realistic, sustainable self-care routine that fits into a busy clinical schedule.
- How administrative workflows and documentation burden impact clinician self-care, and what you can do to reduce stress.
- A practical mental health self-care checklist you can use daily or weekly, plus a downloadable expanded PDF version for ongoing support.
Contents
- Why Self-Care is Essential for Mental Health Professionals
- Understanding Clinician Needs Through Maslow's Hierarchy of Needs
- How to Know if You're Experiencing Therapist Burnout
- Understanding the Unique Stressors Clinicians Face
- Evidence-Based Self-Care Tips for Mental Health Professionals
- A Mental Health Self-Care Checklist for Clinicians
- How ICANotes Supports Clinician Self Care Through Better Workflows
- FAQs: Self-Care for Mental Health Professionals
- Final Thoughts: Self-Care is Ethical Care
Mental health professionals give extraordinary emotional energy to clients each day. While meaningful, this level of empathic labor can quietly take a toll — making clinician self-care essential for ethical, sustainable practice.
This updated 2025 guide incorporates classic concepts like Maslow’s Hierarchy of Needs, a practical therapist burnout self-assessment, and a research-backed list of self-care tips for mental health professionals, along with an easy mental health self-care checklist clinicians can use to stay grounded and well.
Why Self-Care Is Essential for Mental Health Professionals
Mental health clinicians routinely support clients through trauma, crisis, grief, and emotional dysregulation. Without intentional self-care, this work can lead to:
- Compassion fatigue
- Secondary traumatic stress (STS)
- Burnout
- Emotional exhaustion
- Reduced empathy
- Difficulty maintaining boundaries
- Decreated clinical effectiveness
Ethical guidelines (including those from APA, NASW, and ACA) emphasize clinician well-being as a core professional competency. A regulated, supported clinician is better equipped to make sound judgments, provide appropriate interventions, and maintain therapeutic boundaries.
Understanding Clinician Needs Through Maslow's Hierarchy of Needs
Maslow’s model helps clinicians understand why certain types of self-care feel restorative while others don’t. Applying the hierarchy to clinician wellness illuminates the foundations required for sustainable therapeutic work.
1. Physiological Needs (Foundation Level)
Even the most skilled clinician cannot function well without:
- Enough sleep
- Regular meals
- Hydration
- Physical movement
- Adequate rest between sessions
These are often the first sacrifices clinicians make — and the fastest route to burnout.
2. Safety Needs
These include:
- Financial security
- A predictable clinic schedule
- Clear documentation workflows
- Professional liability coverage
- Safe work environments
- Stable routines
When administrative burdens are overwhelming or unpredictable, the clinician’s “safety” layer becomes disrupted.
3. Love & Belonging
Isolation is a major risk for therapists, especially in solo practice. Healthy clinician belonging includes:
- Consultation groups
- Peer supervision
- Supportive professional networks
- Time with friends and family
4. Esteem Needs
Clinicians thrive when they feel:
- Competent
- Effective
- Confident
- Appreciated
Continuing education, skill-building, and supportive feedback all strengthen this level.
5. Self-Actualization
This is where clinicians feel aligned with their purpose. It grows through:
- Creative clinical work
- Meaningful supervision
- Value-aligned practice decisions
- Time for reflection
- Professional growth
Maslow’s model highlights why foundational self-care — sleep, rest, connection — is not indulgent but essential.

How to Know if You're Experiencing Therapist Burnout
Burnout in mental health professionals often emerges gradually. Key signs include:
Emotional Indicators
- Feeling emotionally drained before the day begins
- Loss of empathy or feeling “numb” in sessions
- Irritability, impatience, or cynicism
- Difficulty transitioning out of “clinical mode”
Physical & Cognitive Indicators
- Chronic fatigue
- Poor concentration
- Headaches or muscle tension
- Sleep disruption
- Forgetfulness or difficulty making decisions
Professional Indicators
- Increased charting avoidance
- Reduced sense of accomplishment
- Dreading client sessions
- Contemplating leaving the profession
- Feeling ineffective even when clients are progressing
Relational Indicators
- Withdrawing from colleagues
- Reduced motivation to socialize
- Feeling emotionally unavailable in personal relationships
When to Take Action
Therapist burnout becomes clinically significant when symptoms persist for two weeks or longer or interfere with work, relationships, or sleep.
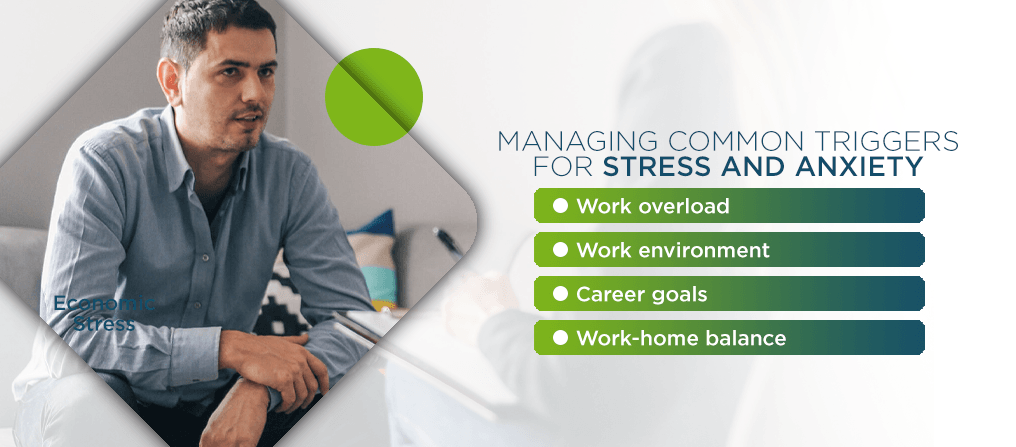
Understanding the Unique Stressors Clinicians Face
Self-care for mental health professionals goes beyond general wellness advice. Clinicians face distinct challenges:
1. Emotional Labor and Empathic Strain
Listening deeply and holding space for others’ trauma requires significant emotional energy.
2. High Caseloads and Administrative Burden
Documentation, scheduling, billing, and insurance requirements can create intense workload pressure.
3. Boundary Complexity
Clinicians often prioritize clients’ needs, unintentionally minimizing their own.
4. Isolation in Practice
Private practitioners may lack day-to-day peer support or consultation.
5. Exposure to Trauma
Therapists treating trauma survivors are at elevated risk for vicarious trauma and anxiety.
Understanding these risks helps clinicians identify the type of self-care that will be most protective and restorative.
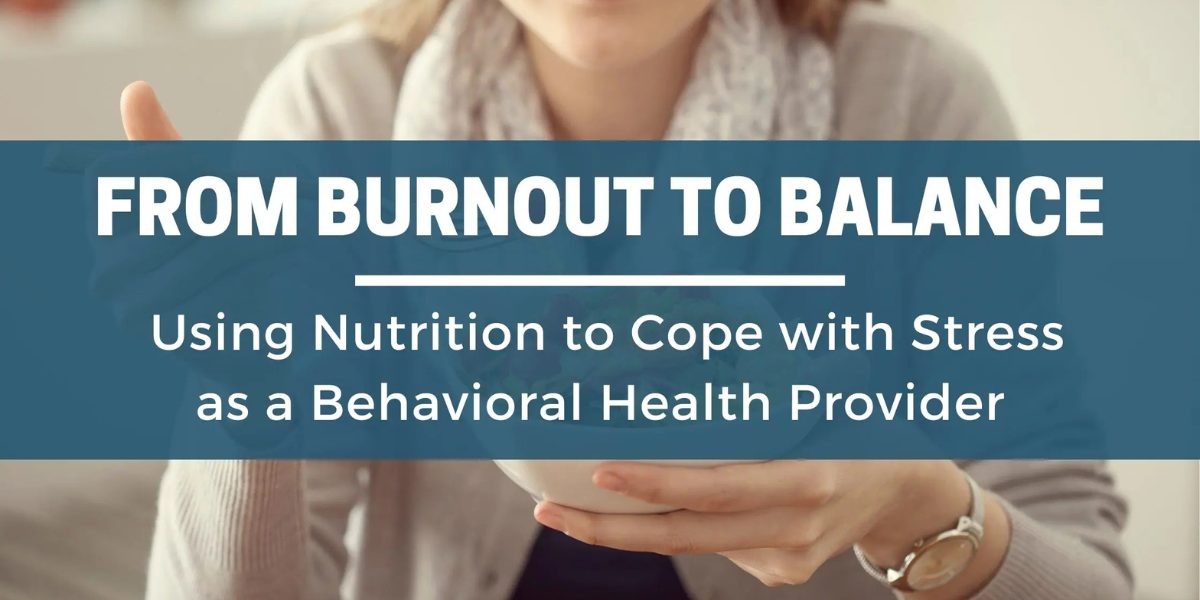
Evidence-Based Self-Care Tips for Mental Health Professionals
Self-care for mental health professionals must go beyond generic wellness advice. Clinicians carry unique emotional, cognitive, and relational burdens that require intentional, research-backed strategies. The following evidence-based self-care tips focus specifically on the demands of therapeutic work, helping you protect your well-being, sustain compassion, and continue providing high-quality care.
1. Emotional & Psychological Self-Care
Prioritizing your emotional well-being supports clinical judgment and resilience.
- Use reflective journaling or clinical debriefing after difficult sessions
- Notice countertransference without self-criticism
- Normalize seeking therapy for yourself
- Build a regular consultation or supervision routine
- Build emotional transition rituals between sessions (e.g., grounding practices, music, or breathwork)
2. Cognitive Self-Care
Protect your mental bandwidth and manage the thought patterns that shape your clinical effectiveness.
- Practice cognitive reframing when you notice negative internal dialogue
- Set realistic expectations for productivity
- Limit perfectionism in documentation
- Use mindfulness to reduce cognitive overload
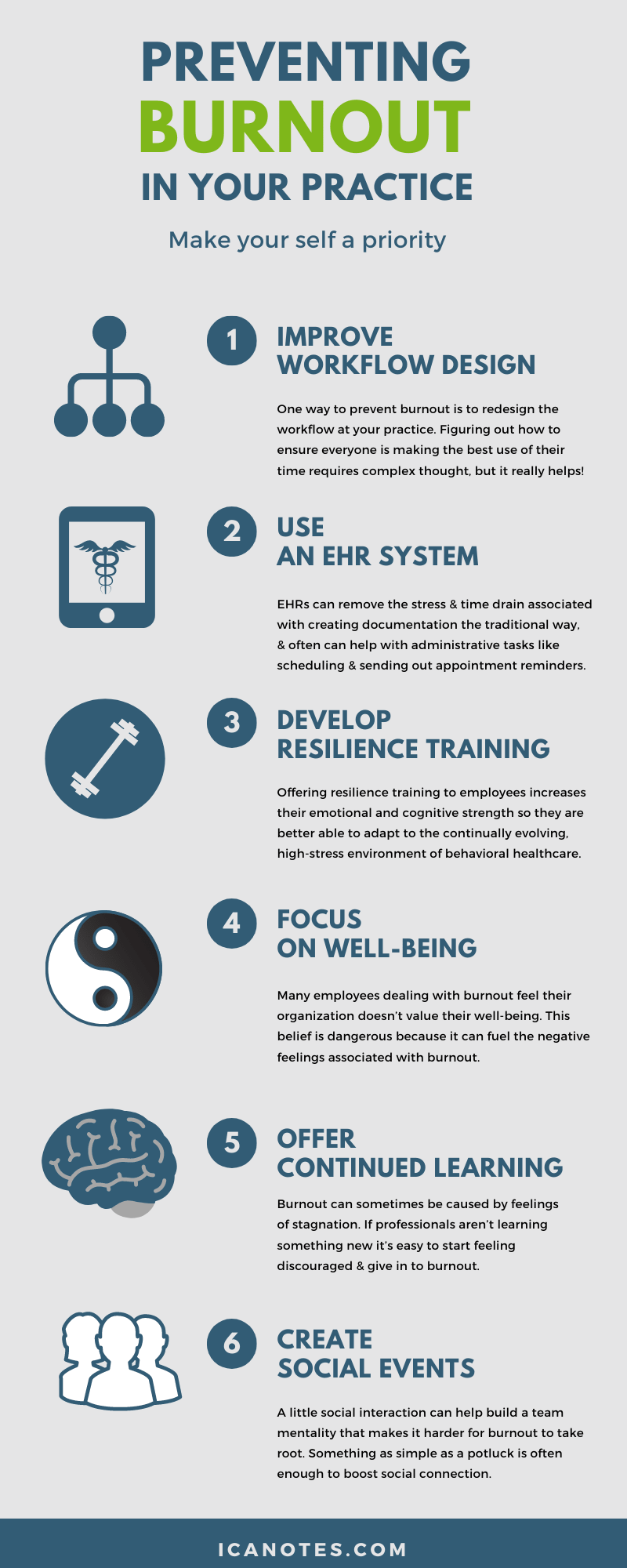
3. Professional Self-Care
Strengthening your clinical foundation reduces overwhelm and improves confidence.
- Maintain a manageable caseload

- Schedule administrative time rather than squeezing it between clients
- Engage in continuing education that inspires rather than drains
- Use structured documentation tools to reduce charting burden
- Join peer groups, consultation circles, or professional communities
4. Physical Self-Care
The mind-body connection is central to clinician well-being.
- Stand, stretch, or walk between sessions
- Practice breathing exercises before emotionally heavy appointments
- Organize your workspace ergonomically
- Create morning and evening routines that support your nervous system
5. Social & Relational Self-Care
Healthy relationships replenish the emotional reserves clinicians depend on.
- Seek peer support
- Connect regularly with non-clinical friends
- Protect evenings and weekends as personal time
- Practice saying “no” without guilt
6. Restorative & Values-Based Self-Care
This does not need to be religious; it can be value-driven.
- Engage in hobbies that are not client-focused
- Spend time in nature
- Build spiritual or mindfulness practices
- Reconnect with the purpose behind your work
A Mental Health Self-Care Checklist for Clinicians
A mental health self-care checklist helps clinicians quickly assess their emotional, physical, and professional wellness, making it easier to maintain balance and prevent therapist burnout. Use the abbreviated checklist below for everyday reference, and download the complete version for a more thorough guide you can keep in your office or planner.
Daily Self-Care Checklist
Weekly Self-Care Checklist
Looking for a complete, printable tool to support ongoing wellness?
Download the full Mental Health Self-Care Checklist PDF—a comprehensive guide designed specifically for therapists, counselors, and behavioral health providers.
How Workflows and Documentation Impact Clinician Self-Care
Many behavioral health professionals experience therapist burnout not because of clinical work, but because of documentation burden.
Time spent:
- rewriting narratives
- tracking treatment plans
- cleaning up notes for audits
- reworking poorly structured documentation
- managing denials caused by documentation errors
…directly reduces the time clinicians have for self-care, supervision, and rest.
Optimizing administrative workflows is one of the most overlooked — and effective — forms of professional self-care.
How ICANotes Supports Clinician Self-Care Through Better Workflows
ICANotes is designed to remove much of the administrative strain that contributes to provider and therapist burnout. Clinicians using ICANotes report improved work-life balance because the software:
- Eliminates hours of weekly documentation with structured, menu-driven notes
- Supports medical necessity and audit-readiness automatically
- Includes a built-in patient portal and telehealth tools
- Streamlines treatment plans with intuitive workflows
- Helps reduce billing pressure through integrated revenue cycle features
- Now includes AI-powered tools like Ambient Listening and a Readability Enhancer to further reduce documentation burden
When administrative tasks are lighter, clinicians have more emotional bandwidth for clients, and for themselves.
FAQs: Self-Care for Mental Health Professionals
Final Thoughts: Self-Care is Ethical Care
Self-care isn’t indulgent; it’s essential for effective, ethical, and sustainable practice. Mental health professionals who care for themselves are more present, empathetic, creative, and grounded in their clinical work.
You take care of your clients every day — you deserve tools and routines that take care of you, too.
Ready to reclaim your time and reduce documentation stress?
Try ICANotes free and see how much easier clinician self-care becomes when your EHR does the heavy lifting.
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
- Complete Notes in Minutes - Purpose-built for behavioral health charting
- Always Audit-Ready – Structured documentation that meets payer requirements
- Keep Your Schedule Full – Automated reminders reduce costly no-shows
- Engage Clients Seamlessly – Secure portal for forms, messages, and payments
- HIPAA-Compliant Telehealth built into your workflow
Complete Notes in Minutes – Purpose-built for behavioral health charting
Always Audit-Ready – Structured documentation that meets payer requirements
Keep Your Schedule Full – Automated reminders reduce costly no-shows
Engage Clients Seamlessly – Secure portal for forms, messages, and payments
HIPAA-Compliant Telehealth built into your workflow
Related Posts
About the Author
Dr. October Boyles is a behavioral health expert and clinical leader with extensive expertise in nursing, compliance, and healthcare operations. With a Doctor of Nursing Practice (DNP) and advanced degrees in nursing, she specializes in evidence-based practices, EHR optimization, and improving outcomes in behavioral health settings. Dr. Boyles is passionate about empowering clinicians with the tools and strategies needed to deliver high-quality, patient-centered care.